Abstract
Recent development in molecular imaging enables measurement of fibrillar amyloid plaque in Alzheimer (AD) brain using positron emission tomography (PET). Three tracers (florbetapir, flutemetamol, florbetaben) have been approved by FDA and EMA for use in clinical assessment of memory impairment to exclude AD. The use of amyloid PET imaging is considered to be appropriate in patients with persistent and progressive unexplained mild cognitive impairment (MCI), in patients with established dementia with atypical clinical course or aetiology and in young patients with atypical-onset dementia. The focus of amyloid PET has so far been to understand the time course of amyloid plaque levels in AD and to use amyloid PET to discriminate between AD and patient with mild cognitive impairment (MCI) who will most likely or less likely convert to AD, respectively, at clinical follow-up. Very few studies have so far directly tested the added value of amyloid imaging as biomarker in diagnostic procedure and patient management in a clinical context. The present study reviews studies describing the possible role of PET amyloid imaging in excluding AD as well as strengthen the diagnosis of AD and detecting prodromal AD. Some studies report as a change in diagnosis following amyloid PET imaging and in therapeutic management and planning for the future for the patient and their family. Future clinical studies are needed to evaluate the appropriate clinical use of amyloid PET imaging in relation to cerebral glucose PET imaging, and CSF biomarkers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Modern molecular imaging has provided new exciting tools to investigate the brain and understand functional disturbances as well the time course of different pathological changes. Several neurodegenerative brain disorders are characterized by proteinopathies. For Alzheimer’s disease (AD) which is the most common neurodegenerative disorder the current predominant hypothesis for the cause of AD is related to dysfunction in brain of processing, deposition and clearance of amyloid-β proteins. The introduction of amyloid positron emission tomography (PET) imaging with the radiotracer 11C-Pittsburgh compound B (11C-PIB) 10 years [1] ago have provided new and valuable insight into the dynamic processes and time course of deposition of fibrillar amyloid in brain from preclinical to clinical stages of AD [2–4]. Several 18F amyloid PET tracers suitable for clinical application have now been tested and three 18F-labelled amyloid PET tracers 18F-florbetapir [5], 18F-florbetaben [6], 18F-flutemetamol [7] have during 2012–2014 been approved by US Food and Drug Administration (FDA) and European medical agency (EMA) for use in clinical assessment of patients with cognitive problems to exclude AD. The 18F amyloid PET tracers with longer half life (110 min) in comparison to 11C-PIB (20 min) are more suitable for use at clinical centres to which the 18F-compound have to be transported due to lack of own cyclotron.
PET studies have shown that the deposition of amyloid in brain precedes the decline in regional cerebral glucose metabolism (18F-FDG PET) which in time course is followed by impairment of neurotransmitter function, atrophy and cognitive decline [2, 8]. Patients with mild cognitive (MCI) with a positive amyloid PET scan have a great risk to convert to AD in comparison to MCI patients with a negative amyloid PET scan [9, 10]. A negative amyloid PET scan in demented patients can exclude AD.
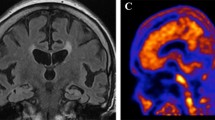
The diagnostic imaging biomarkers field is present under rapid development and its robustness and predictive value in clinical praxis are under investigation. While PET imaging has provided deep insight into the understanding of amyloid pathology in and relation to other pathological disease processes there is still lacking methods for in vivo measures of smaller amyloid peptides, oligomers. In addition on-going research studies on development of new PET tracers for imaging of tau deposition in different stages of AD [11] as well as PET tracers for study of inflammatory processes (astrocytosis, microglia activation) [11–13] in brain will further increase the understanding the time course AD disease pathology and clinical progression (Fig. 1).
Tentative time course of pathological processes at different stages of Alzheimer’s disease [33]
This manuscript will provide a critical review of the usefulness of PET amyloid imaging in a clinical setting.
New diagnostic criteria for Alzheimer’s disease
Two major sets of new clinical diagnostic criteria for AD have been recently proposed by the International Working Group (IWG) [14–16] and the National Institutet of Aging-Alzheimer Association (NIA-AA) [17–19] with the aim to better define clinical phenotypes and to intergrade biomarkers into the diagnostic procedure and thereby be able to diagnose a pre-dementia stage of AD [14, 15] or MCI due to AD [17, 18]. In the recent published IWG-2 criteria [16], amyloid PET and CSF biomarkers (Aβ42, tau, p-tau) are suggested to be considered as diagnostic AD pathological markers. Decline in cerebral glucose metabolism measured by 18F-FDG and atrophy measured by MRI are suggested by the IWG-2 to reflect time course of disease progression and neurodegeneration (Table 1) [16].
Criteria for appropriate use of amyloid PET imaging in clinical setting
The Alzheimer Association and the Society of Nuclear Medicine and Molecular Imaging convened an Amyloid Imaging Taskforce (AIT) to evaluate the potential clinical use of amyloid PET imaging in clinical assessment of patients with cognitive impairment [20, 21]. According to their recommendations (Table 2) it is motivated to perform a clinical amyloid PET scan in patients with persistent or progressive unexplained persistent MCI and in AD patients with an atypical course or an etiologically mixed presentation and in patients with progressive dementia and atypically early age onset (usually defined as 65 years less in age). It is, however, not appropriate to perform amyloid PET scans in patients who fulfil the diagnostic criteria for AD (>65 years) or in people who are asymptomatic or show subjective memory complains (Table 3). Furthermore, the recommendations consider it is inappropriate to perform an amyloid PET scan to determine dementia severity, based upon family history of risk factors as Apolipoprotein E(APOE) genotype or as substitute for genetic testing of autosomal dominant AD [20]. It is also inappropriate to perform an amyloid PET scan for non-medical reasons including assurance or legal, employment decisions [20].
Diagnostic value of 11C-PIB PET imaging in memory clinic setting
18F-FGD PET is already an established method for use in diagnostic process of uncertain cases in some memory clinics. A few number of studies have compared the practical value of 18F-FDG and 11C-PIB PET in a clinical setting. When 154 patients underwent 11C-PIB and 18F-FDG at the Memory clinic of the VU University Medical Centre in Amsterdam, 66 % of the AD patients were found to show positive 11C-PIB scan compared to 28 % for patients with frontotemporal dementia (FLTD), 80 % with Lewy body dementia (LDB) and 30 % for other dementia. The 18F-FDG uptake pattern was comparable with the diagnosis of AD in 58 % of the cases compared to 33 % of the FTLD cases [22]. The use of PET imaging in diagnostic procedure changed the diagnosis in 23 % of the patients. It was estimated that the diagnostic confidence increased from 71 to 87 % after the PET examinations [22]. When 39 % of the patients were clinically followed up after 2 year then clinical diagnosis remained in 96 % of the patients [22]. This study illustrates the clinical observation of AD patients where 11C-PIB PET does not show presence of amyloid fibrillar plaque pathology. Usually as also pointed out by the authors the % of PIB negative AD patients is less than 39 % as observed in the present study [22]. A higher concordance of 84 % between clinical diagnosis and 11C-PIB PET was observed in a study of 140 patients from the University of California, San Francisco (UCSF) Memory and Aging Centre [23]. The primary diagnosis was only changed in 9 % of the cases after PET [23]. Autopsy studies were performed in twenty-four of the patients which showed 96 and 96 % agreement with earlier performed 11C-PIB and 18F-FDG investigations, respectively [23]. When fifty-seven patients underwent 11C-PIB scans at the Copenhagen Memory Clinic, Copenhagen University Hospital, Rigshospitalet [24] to confirm or to rule out AD, 47 % of the patients showed presence of amyloid plaque deposition in the brain which led to that 23 % of the patients were reclassified following the 11C-PIB PET investigation [24]. It is estimated from the present study that overall confidence of the diagnosis increased in 49 % of the patients after the PET scan [24]. When thirty-four patients at the Marqués de Valdecilla University hospital, Santander, Spain underwent 11C-PIB and 18F-FDG [25] a clear separation between non-amnestic and amnestic MCI patients was observed with 11C-PIB while 18F-FDG PET was found to be useful in FTLD patients [25]. It was concluded that both 11C-PIB and 18F-FDG can provide valuable information in diagnostic procedure of cognitive impairment [25].
Diagnostic value of 18F-amyloid PET imaging in memory clinic setting
18F-florbetapir was the first 18F-amyloid PET imaging tracer that was approved by FDA 2012 and EMA 2013 and has been followed by the approval of 18F-florbetaben by EMA 2013, FDA 2014 and flutemetamol by FDA 2013, EMA 2014, respectively. Since all three 18F-amyloid PET tracers were approved quite recently there is still quite few scientific reports published regarding their clinical value in diagnostic routine of assessment of cognitive impairment. A limiting factor for introducing these PET tracers for clinical use is for some countries the issue of reimbursement of the costs of the PET scans.
In a large study of 229 subjects from 39 centres in US the impact of 18F-florbetapir PET scanning on the diagnosis and management was evaluated in patients with progressive impairment [26]. The patients were enrolled in the study with a history of cognitive decline and uncertain diagnosis and thirty-six percent had dementia and 64 percent cognitive impairment. Forty-nine percent of the patients showed a positive 18F-florbetapir scan. The diagnosis was changed in 54.6 % of the cases with and increase in the diagnosis of Ad and it was estimated that the diagnostic confidence increased by 21.6 % and the prescription of cholinesterase inhibitors and memantine increased by 17.7 % in cases with positive amyloid PET scan [26].
In a smaller series of 30 patients, 18F-florbetapir PET investigations were performed at a cognitive evaluation centre of urban dementia centre at Mount Sinai, New York [27]. The clinical assessment of the memory impairment also included neuropsychological assessment as well as neurological examination [27]. The 18F-florbetapir imaging caused change in diagnosis of 10 of the 30 patients (33 %) and clarified the diagnosis in 9 patients (30 %) [27]. It was concluded that the 18F-florbetapir scan in patients with positive scan added important diagnostic certainty and also possibility to help patients and family in the planning of future care and treatment [27]. Similar observations were also observed in evaluation of a small population of 11 patients at Duke University Medical Centre, Durham, US [28]. The clinician surveys were performed before and after 18F-flutemetamol PET scan in 11 patients with memory decline [28] in which six patients were amyloid PET positive and the diagnosis was changed in four of them and the treatment in three patients. In the five patients with negative amyloid PET scan the diagnosis was changed in four patients and the treatment plan in two patients [28]. It was concluded that the both a positive and negative 18F-florbetapir PET may have an impact on clinical decisions especially in cases where the cognitive decline has an uncertain aetiology [28].
When the use of AD biomarkers were investigated in large number of European Alzheimer Consortium Centres, seventy-nine percent of the responders expressed that they felt “very/extremely” comfortable delivering a diagnosis of MCI due to AD when both the biomarkers of amyloid (CSF Aβ 42, amyloid PET) and neuronal injury (18F-FDG) were abnormal and they also agreed that a combination of these biomarkers was a strongly indicative AD signature [29].
In a recent study in cognitive healthy subjects from 59 to 89 years age Jack et al. [30] studied the presence of brain amyloidosis (11C-PIB) and neurodegeneration (18F-FDG/MRI). Eighty-nine percent of the cognitive normal subjects at 89 years of age showed both positive 11C-PIB PET scan and reduced 18F-FDG PET uptake indicating that normal cognitive is possible despite pathological changes in brain at high age [30]. It has recently been suggested that a primary age-related tauopathy (PART) type of pathology might characterize a subset of SNAP (suspected non-Alzheimer pathophysiology) group [31]. Neurodegeneration as measured by FDG PET and CSF tau biomarkers appears to better reflect cognitive decline than amyloid PET imaging [32].
Conclusions
Molecular PET imaging techniques allow measurement of fibrillar amyloid plaque deposition in brain of patients with progressive cognitive impairment. The 18F amyloid PET tracers are presently introduced into the clinical setting and still more experience has to be obtained before significant conclusions can be made of their role in the management of patients with memory impairments. Other biomarkers including CSF biomarkers measuring Aβ42, tau, p-tau are also presently introduced at many memory clinics and other clinics already using CSF biomarkers as a part of the normal assessment. This is also the case for structural imaging with MRI as well as 18F-FDG. It is, therefore, important that international/national guidelines are developed as well as each memory clinic develops recommendations in which order these different biomarkers should be used. However, as illustrated in the present study, the clinical experience from different memory centres, the addition of amyloid PET scan to routine memory assessment battery provide valuable information which also led to change of diagnosis (in most cases from MCI to AD) in a varying proportion of the patients as well as treatment strategies. In addition, positive amyloid PET scan made the physician more confident in the diagnosis of AD which also increases the possibility for future plans with patient and their family. As pointed out by several authors a negative PET amyloid scan which rule out the fact that the patient express AD pathology is valuable for the further clinical management of the patient, especially patients where the diagnosis has been unsure. Visual reading is recommended as routine evaluation of the 18F amyloid PET tracers but quantitative techniques will probably be of great value in cases where the amyloid PET tracer uptakes are close to cutoff values and, therefore, might be difficult to judge with sole visual inspection whether the PET scan is negative or positive. Up to now most clinical studies have been performed using 18F-florbetapir in addition to e 11C-PIB but more clinical experience is needed from the use of 18F-florbetaben and 18F-flutemetamol. Important issues to discuss further involve the ethical issues concerning the disclosure of amyloid PET scans in assessment at early stages of memory assessment.
References
Klunk WE, Engler H, Nordberg A et al (2004) Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol 55:306–319
Nordberg A, Rinne J, Kadir A, Långström B (2010) The use of PET in Alzheimer’s disease. Nat Rev Neurol 6:68–87
Rowe CC, Villemagne VL (2013) Brain amyloid imaging. J Nucl Med Technol 41:11–18
Bentizinger TLS, Blazey T, Jack C et al (2013) Regional variability of imaging biomarkers in autosomal dominant Alzheimer’s disease. Proc Natl Acad Sci 110(47):E4502–E4509. doi:10.1073/pnas
Clark CM, Pontocorvo MJ, Beach TG et al (2012) Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-ß plaques: a prospective cohort study. Lancet Neurol 11:669–678
Villemagne VL, Mulligan RS, Pejoska S et al (2012) Comparison of 11C-PIB and 18F-florbetaben for Aß imaging in ageing and Alzheimer’s disease. Eur J Nucl Med Mol Imaging 39:983–989
Vandenberghe R, Van Laere K, Ivanoiu A et al (2010) 18F-flutemetamol amyloid imaging in Alzheimer’s disease and mild cognitive impairment: a phase 2 trial. Ann Neurol 68:1251–1259
Jack CR, Knopman DS, Jagust WJ et al (2013) Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol 12:207–216
Forsberg A, Engler H, Almkvist O et al (2008) PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol Aging 29:1456–1465
Nordberg A, Carter S, Rinne J et al (2013) A European multi-center PET study of fibrillar amyloid in Alzheimer’s disease. Eur J Nucl Med Mol Imaging 40:104–114
Shah M, Catafu AM (2014) Molecular insights into neurodegeneration: focus on Tau PET radiotracers. J Nucl Med 55:871–878
Carter SF, Scholl M, Almkvist O, Wall A, Engler H, Långström B, Nordberg A (2012) Evidence for astrocytosis in prodromal Alzheimer disease provided by 11 C-deuterium–L-deprenyl: a multitracer PET paradigm combining 11 C Pittsburgh compound B and 18 F-FDG. J Nucl Med 53:37–46
Kreisl WC, Lyoo CH, McGwier M, Snow J, Jenko KJ, Kimura N et al (2013) In vivo radioligand binding to translocator protein correlates with severity of Alzheimer’s disease. Brain 136:2228–2238
Dubois B, Feldman HH, Jacova C et al (2007) Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 6:734–746
Dubois B, Feldman HH, Jacova C et al (2010) Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol 9:1118–1127
Dubois B, Feldman HH, Jacova C et al (2014) Advancing research diagnostic criteria for Alzheimer’s disease: the IWG -2 criteria. Lancet Neurol 13:614–629
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer Dement 7:270–279
Sperling RA, Aisen PS, Beckett LA et al (2011) Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute of Aging-Alzheimer Association workgroups on the diagnostic guidelines for Alzheimer’s disease. Alzheimer Dement 7:280–292
Johnson KA, Minoshima S, Bohnen NI et al. (2013) Appropriate use criteria for amyloid PET: A report of the amyloid imaging task force, the society of nuclear medicine and molecular imaging and the Alzheimer association. Alzheimer and Dementia e 1–16
Johnson KA, Minoshima S, Bohnen NI et al (2013) Update on appropriate use criteria for amyloid PET imaging:dementia experts, mild cognitive impairment, and education. J Nucl Med 54:977–983
Ossenkoppele R, Prins ND, Pijnenburg YAL (2013) Impact of molecular imaging on the diagnostic process in a memory clinic. Alzheimer Dement 9:414–421
Sánchez-Juan P, Ghosh PM, Hagen J et al (2014) Practical utility of amyloid and FDG-PET in an academi dementia center. Neurology 82:230–238
Frederiksen KS, Hasselbalch SG, Hejl A-M et al (2012) Added diagnostic value of 11C-PIB-PET in memory clinic patients with uncertain diagnosis. Dement Geriatr Cogn Disorder 2:610–621
Banzo I, Jiménez-Bonilla J, Ortega-Nava F et al (2014) Amyloid imaging with 11C-PIB PET/CT and glucose metabolism with 18F-FDG PET/CT in a study on cognitive impairment in the clinical setting. Nucl Med Commun 35:238–244
Grundman M, Pontecorvo MJ, Salloway SP et al (2013) Potential impact of amyloid imaging on diagnosis and intended management in patients with progressive cognitive decline. Alzheimer Dis Assoc Disord 27:4–15
Mitis EM, Bender HA, Kostakoglu L et al (2014) A consecutive case series experience with [18F] florbetapir PET imaging in an urban dementia center: impact on quality of life, decision making and disposition. Mol Neurodegener 9:10
Zhannas AS, Doraiswamy PM, Shpanskaya KS et al (2014) Impact of 18F-florbetapir PET imaging of β-amyloid neuritic plaque density on clinical decision on clinical decision-making. Neurocase 4:466–473
Bochetta M, Galluzzi S, Kehoe PG et al (2014) The use of biomarkers for the etiologic diagnosis of MCI in Europe: an EADC survey. Alzheimer Dement. doi:10.1016/j.jalz.2014.06.006
Jack CR, Wister HJ, Weigand SD, Rocca WA et al (2014) Age-specific population frequencies of cerebral ß-amyloidosis and neurodegeneration among people with normal cognitive function aged 50–89 years: a cross—sectional study. Lancet Neurol 13:997–1005
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF et al (2014) Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol 128:755–766
Perani D (2014) FDG PET and amyloid PET-imaging: the diverging paths. Curr Opion Neurol 27:405–413
Nordberg A (2011) Molecular imaging in Alzheimer’s disease—new perspectives on biomarkers for early diagnosis and drug development. Alzheimer Res Ther 3:34.e.1–34.e.9
Acknowledgments
The supports from the Swedish Research Council (project 05817), the Strategic Research Program in Neuroscience at Karolinska Institutet, the Swedish Brain Power, the Old Servants foundation, the Gun and Bertil Stohne’s foundation, the Alzheimer Foundation in Sweden, Brain Foundation, the Regional Agreement on Medical Training and Clinical Research (ALF) between Stockholm County Council and the Karolinska Institutet, the JPND Project BIOMARKAPD, the EU FP7 large-scale integrating project INMiND (http://www.uni-muenster. de/INMiND) research are highly acknowledged.
Conflict of interest
The author declares no conflict of interest.
Human and animal studies
This study does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nordberg, A. The use of amyloid imaging in clinical praxis: a critical review. Clin Transl Imaging 3, 7–11 (2015). https://doi.org/10.1007/s40336-015-0100-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-015-0100-8