Abstract
Purpose/background
[18F]fluoroethylcholine (18FECH) has been shown to be a valuable PET-tracer in recurrent prostate cancer (PCa), but still has limited accuracy. RM2 is a gastrin-releasing peptide receptor (GRPr) antagonist that binds to GRPr on PCa cells. Recent studies suggest that GRPr imaging with PET/CT is a promising technique for staging and restaging of PCa. We explore the value of GRPr-PET using the 68Ga-labeled GRPr antagonist RM2 in a selected population of patients with biochemically recurrent PCa and a negative/inconclusive 18FECH-PET/CT.
Material and methods
In this retrospective study 16 men with biochemical PCa relapse and negative (n = 14) or inconclusive (n = 2) 18FECH-PET/CT underwent whole-body 68Ga-RM2-PET/CT. Mean time from 18FECH-PET/CT to 68Ga-RM2-PET/CT was 6.1 ± 6.8 months. Primary therapies in these patients were radical prostatectomy (n = 13; 81.3%) or radiotherapy (n = 3; 18.7%). 14/16 patients (87.5%) had already undergone salvage therapies because of biochemical relapse prior to 68Ga-RM2-PET/CT imaging. Mean ± SD PSA at 68Ga-RM2-PET/CT was 19.4 ± 53.5 ng/ml (range 1.06–226.4 ng/ml).
Results
68Ga-RM2-PET/CT showed at least one region with focal pathological uptake in 10/16 patients (62.5%), being suggestive of local relapse (n = 4), lymph node metastases (LNM; n = 4), bone metastases (n = 1) and lung metastasis with hilar LNM (n = 1). Seven of ten positive 68Ga-RM2 scans were positively confirmed by surgical resection and histology of the lesions (n = 2), by response to site-directed therapies (n = 2) or by further imaging (n = 3). Patients with a positive 68Ga-RM2-scan showed a significantly higher median PSA (6.8 ng/ml, IQR 10.2 ng/ml) value than those with a negative scan (1.5 ng/ml, IQR 3.1 ng/ml; p = 0.016). Gleason scores or concomitant antihormonal therapy had no apparent impact on the detection of recurrent disease.
Conclusion
Even in this highly selected population of patients with known biochemical recurrence but negative or inconclusive 18FECH-PET/CT, a 68Ga-RM2-PET/CT was helpful to localize PCa recurrence in the majority of the cases. Thus, 68Ga-RM2-PET/CT deserves further investigation as a promising imaging modality for imaging PCa recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy and radiotherapy (RT) are standard therapies for patients with primary prostate cancer (PCa) [1]. Despite good clinical response after primary therapy, PCa recurs in 20–50% of cases, depending on stage at diagnosis [1]. PCa recurrence can be reliably detected by an increase of the prostate specific antigen (PSA) in serum [1, 2]. Identification of the exact site of tumor recurrence (e.g., lymph node metastases or bone metastases) is critical for further decision-making. Unfortunately, to date, none of the conventional imaging modalities such as transrectal ultrasound, computed tomography (CT), magnetic resonance imaging (MRI) or bone-scintigraphy provides a sufficient diagnostic accuracy for reliable detection of primary or recurrent PCa [2, 3] in patients with low PSA levels who are most likely to benefit from local therapies. Therefore, there is a need for better imaging modalities for staging and re-staging of PCa and treatment monitoring.
Positron emission tomography (PET) with 11C- or 18F–labeled choline derivatives is superior to MRI and CT for recurrent PCa [4, 5] but the sensitivity of choline-PET/CT for detecting sites of tumor strongly depends on the PSA (Prostate specific antigen) value at the time of imaging, Gleason score, and other clinical factors [4]. Therefore, there is a clear need for other imaging agents to localize recurrent prostate cancer. Most attention has been paid to tracers targeting the prostate-specific membrane antigen (PSMA), the androgen receptor and the gastrin-releasing peptide receptor (GRPr) (for review see [6]).
The GRPr (also known as bombesin receptor) and its ligand, the gastrin-releasing peptide (GRP), are physiologically expressed in the central nervous system and the gastrointestinal tract [7]. An overexpression of GRPr has been observed in a variety of malignant tumors but most consistently in PCa and its percursors [7]. An autoradiographic study found markedly increased binding of radiolabeled bombesin (125I–Tyr4-bombesin) in primary PCa as well as in prostatic intraepithelial neoplasia. In contrast, normal and hyperplastic prostate tissue demonstrated no or very low binding of 125I–Tyr4-bombesin [8]. Consequently, various GRPr targeting radiotracers haven been investigated by several groups [9–12]. To avoid side effects provoked by agonists and because of a higher number of bindings sites, GRPr antagonists are preferred to GRPr-agonists [13]. 68Ga-RM2 (also known as BAY86–7548) is an antagonistic PET tracer binding to the human GRPr on PCa cells that shows favorable kinetic and dosimetric properties and has been demonstrated to be a promising tracer for detecting of primary prostate cancer [10, 12]. However, the number of reports on GRPr imaging in recurrent PCa is still scarce [9–11, 14].
Thus, we investigated the diagnostic value of 68Ga-RM2-PET/CT in patients with biochemical recurrent PCa and negative or inconclusive 18FECH-PET/CT, which was the standard of care at our institution at that time. In addition, we explored the impact of variables such as PSA, antihormonal therapy (AHT) and Gleason score on diagnostic performance.
Material and methods
Design, patients
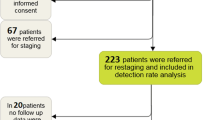
This retrospective analysis comprises 16 men with histologically confirmed PCa after primary therapy and biochemical relapse based on rising PSA. Until the end of 2013, 18FECH-PET/CT was the standard of care for prostate cancer relapse at our institution. Due to the fact that we have access to RM2-PET/CT, some patients with negative or inconclusive 18FECH-PET/CT were investigated with RM2-PET/CT between 2013 and 2014. When PSMA-PET/CT was newly established at our center in 2014, consequently several patients from this cohort underwent a PSMA-PET/CT.
“Negative” or “inconclusive” (i.e., only questionable findings, not deemed to justify further treatment decisions by the referring PCa specialist) results on clinical routine 18FECH-PET/CT read by experienced observers led to subsequent 68Ga-RM2-PET/CT on compassionate-use basis. All patients gave written informed consent for the retrospective data analysis. The retrospective data analysis was reviewed and approved by the local Ethics Committee (N° 562/15). 68Ga-RM2-PET/CT was performed on a compassionate-use basis as a choline-PET/CT was negative or inconclusive. Mean age at 18FECH-PET/CT and 68Ga-RM2-PET/CT was 64.1 ± 8.6 and 64.6 ± 8.9 years (mean value ± standard deviation). Gleason score and PSA (ng/ml) at 18FECH-PET/CT and 68Ga-RM2-PET are shown in Table 1. Median time from primary PCa therapy and 68Ga-RM2-PET/CT until last visit was 79.4 months and 10.9 months, respectively. Detailed information about primary therapies is shown in Supplement 1.
Synthesis of 68Ga-RM2
Radiolabelling of RM2 with 68GaCl3 was performed with the fully automated synthesis module Pharmtracer from Eckert & Ziegler (Berlin, Germany). The 68Ge/68Ga generator was eluted with HCl (0.1 M, 7 ml). The eluate was loaded on a cation exchange resin (Strata x-c, Phenomenex) and 68Ga(III) was eluted from the cartridge into the reaction vial using a 97.6% acetone/0.02 M HCl solution. The reaction vial contained 60 μg RM2 in 2 ml sodium acetate buffer (0.2 M, pH 4.0) and 200 μl ethanol. Labeling was accomplished by heating the reaction mixture at 95 °C for 10 min. The solution was then passed over a C18 light cartridge (Waters, USA), washed with 3 ml saline and eluted with 1 ml 50% ethanol. The final product was constituted by addition of 7 ml saline and sterilized by filtration using Millex 0.22 μm filter (Millipore, USA). The decay-corrected yield was >90% and the radiochemical purity of the final product was >98%. The product was sterile and pyrogen-free (<0.5 EU ml−1). The specific activity of 68Ga-RM2 was in the range of 15–25 GBq μmol−1 depending on the age of the generator.
18FECH-PET/CT and 68Ga-RM2-PET/CT imaging
All patients fasted for at least 4 h (h) before the administration of the radiopharmaceutical and were asked to void before starting the study. For 18FECH imaging patients underwent a PET scan (from base of skull to proximal thighs; 2 min. Per bed position) starting 45 min post injection (p.i.) of 255.2 ± 40.5 MBq 18FECH. For 68Ga-RM2 imaging patients underwent a PET scan (from base of skull to proximal thighs; 2 min per bed position) starting 1 h p.i. of 231.2 ± 63.3 MBq 68Ga-RM2. Scans were either performed on a GEMINI TF PET/CT or a GEMINI TF BIG BORE PET/CT (both Philips Healthcare, Cleveland, OH). Time per bed position was 2 min. For 18FECH-PET/CT and 68Ga-RM2-PET/CT. PET- and CT-slice thickness was 3 mm. Depending on contraindications and availability of previous CT images, whole body CT scan was performed as contrast-enhanced diagnostic CT (120 kVp, 100–400 mAs, dose modulation) or low-dose CT (120 kVp, 25 mAs) for attenuation correction.
PET/CT-image analysis
All 68Ga-RM2-PET/CTs were re-analyzed by two board-certified nuclear medicine specialists in consensus. Presence of lesions suspicious for PCa on PET images was defined as any focal uptake of 68Ga-RM2 greater than physiological local background. The uptake of 68Ga-RM2 was quantified by standardized uptake values (SUV) normalized to the patient’s body weight. Local recurrence and metastases (LNM or other) were visually delineated in the slice with the highest tracer uptake and the SUVmax was recorded (in case of more than one lesion per site the lesions with the highest SUV was chosen for SUV measurement). Because of the small tumor size, no SUVmean values were determined because they would have been heavily influenced by partial volume effects. For determination of background activity, a circular regions of interest was placed in the center of the musculus gluteus maximus (see Table 2).
Patient follow-up and reference standard
Follow-up visits and prostate cancer treatment after 68Ga-RM2-PET/CT took place according to the clinical routine of the attending urologists and radiation oncologist. Clinical follow-up (last visit) for the current analysis was 10.9 ± 13.7 (median 7.0 / range: 33.4–4.6) months after 68Ga-RM2-PET/CT. Median time from 68Ga-RM2-PET/CT to the event of confirmation or nonconformation of 68Ga-RM2-PET/CT-results (imaging, surgery, radiotherapy) was 5.3 ± 5.9 (median 2.1, range: 18.2–0-.2) months (Table 2).
Immunohistochemistry anti-GRPr/anti-BB2
Immunohistochemistry was used to confirm GRPr expression in tumor samples obtained after the 68Ga-RM2-PET/CT scan. Two μm tissue slices from LNM were prepared and stained for Bombesin (BB)2 receptor. Heat-induced antigen retrieval was performed at 95 °C (30 min/pH 6.1) using Dako antigen retrieval buffer S1699. Afterwards, incubation with Rabbit anti-BB2 antibody (BB2 antibody ab39963, Lot: GR75800–1, 1:300; Abcam, UK) at room temperature (20 min) was realized followed by staining with an EnVision TM Flex Visualization system (DAKO K8000) using the AutostainerPlus (DAKO, Hamburg, Germany). After washing (PBS and water), counterstaining with hematoxylin and eosin was performed. Staining of normal pancreas parenchyma was used as a positive control for BB2 receptors.
Statistics
Descriptive statistics was done by calculating mean ± standard deviation (SD), median and interquartile range (IQR). Due to the lack of Gaussian distribution (D’Agostino & Pearson omnibus normality test) continuous variables were compared with a two-sided Mann-Whitney test or with a two-sided Wilcoxon matched-pairs signed rank test. Categorical variables were compared by Fischer’s exact test. All statistics were done with GraphPad Prism 6.
Results
Patient characteristics / history
Mean initial PSA at diagnosis of PCa was 18.5 ± 13.5 ng/ml (median 14.4 ng/ml). Seven of 16 men had a T2 stage (43.8%) and 9/16 a T3 stage (56.2%) (Supplement 1). Radical prostatectomy including lymphadenectomy or radiotherapy as primary therapy were performed in 13/16 (81.3%) and 3/16 men (18.7%), respectively (Supplement 1). After 21.2 ± 36.0 months (median 9.5 months, IQR 19.3) the first biochemical recurrence was observed in all 16 men. Thereupon in 14/16 men at least one salvage therapy was conducted (Table 1). The 13/14 men had a radiotherapy of the prostatic fossa, (6/14) had a metastases-directed therapy. Intermittent AHT was administered in 8/16 men prior to 68Ga-RM2-PET/CT.
Clinical setting at 18FECH-PET/CT and 68Ga-RM2-PET/CT
18FECH-PET/CT was performed in all patients to localize recurrent PCa in the setting of biochemical recurrence. Fourteen of 16 18FECH-PET/CTs did not show any pathologic findings, 2/16 were inconclusive (Table 2). 68Ga-RM2-PET/CT was performed mean 6.1 ± 6.8 months (median 2.9 months, IQR 8.5) after 18FECH-PET/CT. Mean 4.7 ± 3.0 (median 4.1) years after the event of first biochemical relapse the 68Ga-RM2-PET/CT was conducted.
Median PSA at time of 18FECH-PET/CT (2.4 ng/ml, IQR 4.9 ng/ml, range: 0.74–26 ng/ml) was significantly lower as compared to median PSA at 68Ga-RM2-PET/CT (5.5 ng/ml, IQR 6.8, range: 1.06–226.4 ng/ml). AHT was administered to 4/16 (25%) of the patients at time of 68Ga-RM2-PET/CT and to 5/16 (31.3%) at the time of 18FECH-PET/CT (p = 1.00).
Findings on 68Ga-RM2-PET/CT
After injection of RM2, no side effects were observed. Results of all 16 68Ga-RM2-PET/CTs are summarized in Table 2. Overall, 68Ga-RM2-PET/CT was abnormal in ten of the 16 patients (63%). The two patients with inconclusive results on 18FECH-PET/CT (patients N°4, N°12) showed clearly positive findings on 68Ga-RM2-PET/CT: The 18FECH-PET/CT of patient N°4 depicted only mild tracer accumulation in left presacral lymph nodes (LN) and LNs at the aortic bifurcation, whereas the 68Ga-RM2-PET/CT revealed intense tracer accumulation in these LNs (presacral/aortic bifurcation) and additional focal tracer uptake of right iliac LNs. In patient N°12, the 68Ga-RM2-PET/CT showed multiple bone lesions (e.g., scapula, sternum, vertebral body, acromion) while there was only one mildly metabolically active lesion on 18FECH-PET/CT. SUVs (standard uptake values) of lesions suspicions for local recurrence or metastases ranged from 2.0 to 8.1 (Table 2). Mean SUV of background (musculus gluteus maximus) was 0.38 ± 0.09.
Impact of PSA-level, Gleason score and antihormonal therapy on 68Ga-RM2-PET/CT
Patients with a positive 68Ga-RM2 scan showed a significantly higher PSA value (median 6.8 ng/ml, IQR 10.2 ng/ml, range: 1.53–226.4 ng/ml) than those with a negative scan (median 1.5 ng/ml, IQR 3.1 ng/ml, range: 1.06–7.0 ng/ml (p = 0.016) (Fig. 1a). Distribution of Gleason scores (stratified as low-risk vs. high-risk cases, i.e., Gleason 6-7a vs. Gleason 7b-9) showed no significant association (p = 0.63) with negative and positive results on 68Ga-RM2-PET/CT (Fig. 1b). The 2/10 of the patients with a positive 68Ga-RM2-PET/CT were under AHT compared to 2/6 of the men with a negative 68Ga-RM2-PET/CT (p = 0.60) (Table 1).
(a) PSA values (median 1.5 ng/ml) in patients with negative results of 68Ga-RM2-PET/CT was significantly lower than PSA values (median 6.8 ng/ml) of patients with positive results (p = 0.016). (b) Distribution of Gleason scores showed no association with negative and positive findings on 68Ga-RM2-PET/CTs (p = 0.63; stratified as low-risk vs. high-risk cases, i.e. Gl. 6-7a vs. Gl. 7b-9) (p = 0.63)
Confirmation of 68Ga-RM2-PET/CT results
For the ten men with a positive 68Ga-RM2-PET/CT, the findings were confirmed by surgical resection and histology of the lesions (n = 2; including immunohistochemistry, see Fig. 3A, B), by response to site-directed therapies (n = 2) or by further imaging (n = 3) (Table 2). For the remaining three men with a positive 68Ga-RM2-PET/CT, the presence of PCa manifestations was not confirmed in two patients (biopsy with further imaging n = 1, further imaging n = 1) and is still unclear in one patient (mean follow-up 10.9 ± 13.7 (median 7.0) months) (Table 2). All these non-confirmed positive findings concerned patients with suspected local recurrence (i.e., three of four cases with suspected local recurrence in total) (Table 2).
68Ga-RM2-PET/CT was negative in six patients. A subsequent 68Ga-HBED-CC-PSMA-PET/CT was also negative in two of these patients. In two additional cases, a 68Ga-HBED-CC-PSMA-PET/CT strongly suggested the presence of LNM. Of the remaining two patients with a negative 68Ga-RM2-PET, one patient showed the unusual finding of a solitary bone metastasis of the skull on bone-scan and CT, while the skull has been outside the field of view (FOV) in the 68Ga-RM2- and the 18FECH-PET/CT. The remaining patient with negative 68Ga-RM2-scan received no further imaging studies but received AHT and showed a stable PSA at the level of 2 ng/ml (Table 2).
As representative examples, 68Ga-RM2- and 18FECH-PET and corresponding CT sections of patients N° 4, 5 and 12 are shown in Fig. 2a-c. Because of detected presacral and iliac LNM by 68Ga-RM2-PET/CT, patient N°4 underwent a salvage lymph node dissection with histological confirmation of these lesions. He had a PSA decline after therapy (Fig. 2a). In patient N°5 (Fig. 2b) a salvage radiotherapy of suspicious iliac and presacral LNM was performed which was followed by a marked PSA decline (Fig. 3).
18FECH-PET/CT and 68Ga-RM2-PET with corresponding CT from three patients. (a) In patient N°4 68Ga-RM2-PET/CT uncovered presacral and parailiac (not shown) LNM. (b) In patient N°5 68Ga-RM2-PET/CT detected parailiac and presacral (not shown) LNM. (c) In patient N°12 68Ga-RM2-PET/CT showed multiple bone lesions while 18FECH-PET/CT showed only one lesion with slight tracer uptake in the left scapula
Discussion
The aim of our investigation was to explore the value of GRPr-PET in a selected population of patients with biochemically recurrent PCa with prior non-contributory (negative/inconclusive) 18FECH-PET/CT using the 68Ga-labeled GRPr antagonist RM2. We demonstrate that even in this highly selected, most challenging cohort of patients, 68Ga-RM2-PET/CT detected at least one region with focal pathological uptake in 62.5% of the patients (10/16). In seven of these ten cases, positive findings were confirmed by histopathology or by clinical follow-up (Table 2).
Literature on PET-Imaging using GRPr ligands in patients with PCa-recurrence and information about true-positive (confirmed) lesions are rare and largely different (also due to the different tracers used). In the literature, the number of individuals with PCa relapse undergoing a RM2-PET/CT is apparently low (Kähkönen et al. n = 3 [10], Minamimoto et al. n = 7 [14], Mather et al. n = 6 [15], Sah et al. n = 5 [11]). So far, data from 21 men with PCa recurrence undergoing PET imaging with various radiolabeled GRPr ligands (among others 68Ga-RM2) are available [10, 11, 14, 16], and we were able to contribute the clinical data from 16 PCa patients undergoing a 68Ga-RM2-PET/CT. Considering these 21 patients and the patients from our cohort (n = 16), pathological focal uptake on GRPr-PET was detected in 23/37 cases. The majority of the patients (11/23 = 48%) had the suspicion of lymph node metastases (LNM) alone, while only 2/23 (9%) and 4/23 (17%) patients where suspected to suffer from both LNM and bone metastases (BM), and BM alone, respectively (among other manifestations and combinations). Information on a confirmation of these lesions is not completely given in the published studies [10, 11, 14, 16]. Furthermore, the available data from the 14 patients (literature and our cohort) without suspicious findings on GRPr-PET indicates that in 6/14 (43%) patients bone metastases were finally discovered by follow-up imaging (for comparison: 3/14 (21.5%) local relapses, 2/14 (14%) LNM, 3/14 (21.5%) no suspicious lesion) [10, 11, 14, 16]. In our cohort only 1/16 individuals showed bone metastases in the PET FOV; in this patient 68Ga-RM2-PET detected more bone lesions than 18FECH-PET/CT (Table 1). Taken together, these findings suggest that GRPr PET may be of limited sensitivity for the detection of bone metastases in PCa which warrants further investigation.
We note that most of the true positive GRPr PET/CT findings were observed in lymph node metastases, but this may be due to patient selection. Only two patients developed osseous metastases during follow-up. In one patient these metastases were detected by GRPr PET/CT; in the other patient a solitary skull metastasis was outside of the field-of-view of the GRPr PET/CT scan. Two presumable false positive findings were observed in the prostate bed, these may be caused by artifacts from activity in the urinary bladder.
Generally, imaging in cases of biochemical PCa-recurrence with PSA-values below 1 ng/ml and a slow PSA-doubling time (suspicion of local relapse in the prostate fossa) is of course a relevant clinical issue in order to verify or exclude local relapse of PCa-recurrence. Furthermore, imaging (e.g., with RM2-PET/CT or PSMA-PET/CT) at PSA-levels clearly >1 ng/ml (e.g., median PSA 5.45 ng/ml in our cohort) is of great importance in order to follow the strategy of metastasis-directed therapy such as salvage lymph node dissection or target radiotherapy increasingly performed in many European countries [17].
It is difficult to state a clear association between the PSA level and the probability of positive findings of 68Ga-RM2-PET/CT. In our study we observed that the median PSA level was significantly higher in patients with positive findings compared to those with negative findings on 68Ga-RM2-PET/CT. Pooling the available data from the literature and our study, PSA values of patients with positive GRPr PET scans (n = 23) ranged from 0.36–226.4 ng/ml (mean: 22 ng/ml, median: 7.2 ng/ml), PSA from negative GRPr PET scans (n = 14) ranged from 1.06–282 ng/ml (mean: 56.7 ng/ml, median 6.9 ng/ml) [10, 11, 14, 16], thus showing a wide overlap.
Data about comparison of PET-CT results from 68Ga-RM2-PET/CT versus 68Ga-HBED-PSMA-PET/CT are scarce. Four of six patients with negative 68Ga-RM2-PET/CT also underwent 68Ga-HBED-PSMA-PET/CT during follow-up (mean 5.8 ± 3.9, median 5.4 months after 68Ga-RM2-PET/CT), which was also negative in two patients, while in two patients 68Ga-HBED-PSMA-PET/CT suggested the presence of LNM. In contrast to this sequential imaging approach, Minamimoto et al. investigated seven patients with recurrent PCa using both 68Ga-RM2-PET/CT and 68Ga-HBED-PSMA-PET/CT within mean 42.9 ± 25.2 days (range 13–85 days) [14]. They found that the locations of suspected metastases were almost the same for both tracers (n = 5 LNM, n = 1 LNM + bone metastases, n = 1 local relapse detected only by 68Ga-HBED-PSMA- but not 68Ga-RM2-PET/CT). Periaortal LNM were more clearly visualized by 68Ga-RM2-PET/CT in two patients due to the lack of tracer accumulation in the small intestine. These findings underline that additional work, such as imaging studies using both tracers, is needed to understand the expression of PSMA and GRPr in different types and stages of prostate cancer and the merits of the respective molecular imaging techniques [14].
Limitations
Limitations of our study are the small number of patients investigated, the heterogeneity of the patients concerning PCa stages, tumor burden, PSA level and Gleason score at time of biochemical relapse and that most of the findings were not histologically confirmed. Due to the nature of PCa, even if recurrent, most patients present with considerable survival rates associated with several differential PCa therapies in their history (different adjuvant therapies after primary therapy and prior to RM2-PET/CT), this also caused heterogeneity in our cohort.
Furthermore, the time between 18FECH-PET and 68Ga-RM2-PET/CT (mean 6.1 ± 6.8 months) and the higher PSA level at 68Ga-RM2-PE[18] T/CT might cause bias in results. One cannot exclude that at least some of the initial 18FECH-PET-negative patients would have been positive in a follow-up 18FECH-PET scan after this time period. Performance of 68Ga-RM2-PET/CT only in those patients with preceding negative/inconclusive 18FECH-PET/CT represents a selection of highly challenging patients which probably reduced the chance of positive findings on the subsequent 68Ga-RM2-PET/CT. This suggests that the true detection rate might have been higher in a more general population of PCa patients with biochemical relapse.
Conclusion
In the scenario of PCa relapse and a negative/inconclusive 18FECH-PET/CT, a consecutive 68Ga-RM2-PET/CT generated important information for clinical decision-making in the majority of the patients examined in our study. Thus, 68Ga-RM2 is potentially a valuable new PET tracer for imaging PCa relapse. Larger prospective clinical trials are warranted to determine the role of 68Ga-RM2-PET/CT for PCa imaging in the clinical setting.
References
Han M, Partin AW, Zahurak M. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003;169(2):517–23. doi:10.1097/01.ju.0000045749.90353.c7.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65(1):124–37. doi:10.1016/j.eururo.2013.09.046.
Hovels AM, Heesakkers RA, Adang EM. The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol. 2008;63(4):387–95. doi:10.1016/j.crad.2007.05.022.
Picchio M, Briganti A, Fanti S, Heidenreich A, Krause BJ, Messa C, et al. The role of choline positron emission tomography/computed tomography in the management of patients with prostate-specific antigen progression after radical treatment of prostate cancer. Eur Urol. 2011;59(1):51–60. doi:10.1016/j.eururo.2010.09.004.
Cimitan M, Evangelista L, Hodolic M, Mariani G, Baseric T, Bodanza V, et al. Gleason score at diagnosis predicts the rate of detection of 18F-choline PET/CT performed when biochemical evidence indicates recurrence of prostate cancer: experience with 1,000 patients. J Nucl Med. 2015;56(2):209–15. doi:10.2967/jnumed.114.141887.
Jadvar H. Molecular imaging of prostate cancer: PET radiotracers. AJR Am J Roentgenol. 2012;199(2):278–91. doi:10.2214/AJR.12.8816.
Jensen RT, Battey JF, Spindel ER, Benya RV. International Union of Pharmacology. LXVIII. Mammalian bombesin receptors: nomenclature, distribution, pharmacology, signaling, and functions in normal and disease states. Pharmacol Rev. 2008;60(1):1–42. doi:10.1124/pr.107.07108.
Markwalder R, Reubi JC. Gastrin-releasing peptide receptors in the human prostate: relation to neoplastic transformation. Cancer Res. 1999;59(5):1152–9.
Wieser G, Mansi R, Grosu AL, Schultze-Seemann W, Dumont-Walter RA, Meyer PT, et al. Positron emission tomography (PET) imaging of prostate cancer with a gastrin releasing peptide receptor antagonist--from mice to men. Theranostics. 2014;4(4):412–9. doi:10.7150/thno.7324.
Kahkonen E, Jambor I, Kemppainen J, Lehtio K, Gronroos TJ, Kuisma A, et al. In vivo imaging of prostate cancer using [68Ga]-labeled bombesin analog BAY86-7548. Clin Cancer Res. 2013;19(19):5434–43. doi:10.1158/1078-0432.CCR-12-3490.
Sah BR, Burger IA, Schibli R, Friebe M, Dinkelborg L, Graham K, et al. Dosimetry and first clinical evaluation of the new 18F-radiolabeled bombesin analogue BAY 864367 in patients with prostate cancer. J Nucl Med. 2015;56(3):372–8. doi:10.2967/jnumed.114.147116.
Roivainen A, Kahkonen E, Luoto P, Borkowski S, Hofmann B, Jambor I, et al. Plasma pharmacokinetics, whole-body distribution, metabolism, and radiation dosimetry of 68Ga bombesin antagonist BAY 86-7548 in healthy men. J Nucl Med. 2013;54(6):867–72. doi:10.2967/jnumed.112.114082.
Mansi R, Wang X, Forrer F, Waser B, Cescato R, Graham K, et al. Development of a potent DOTA-conjugated bombesin antagonist for targeting GRPr-positive tumours. Eur J Nucl Med Mol Imaging. 2011;38(1):97–107. doi:10.1007/s00259-010-1596-9.
Minamimoto R, Hancock S, Schneider B, Chin F, Jamali M, Loening AM, et al. Pilot comparison of 68Ga-RM2 PET and 68Ga-PSMA PET in patients with biochemically recurrent prostate cancer. J Nucl Med. 2015; doi:10.2967/jnumed.115.168393.
Mather SJ, Nock BA, Maina T, Gibson V, Ellison D, Murray I, et al. GRP receptor imaging of prostate cancer using [Tc]Demobesin 4: a first-in-man study. Mol Imaging Biol. 2014; doi:10.1007/s11307-014-0754-z.
Mather SJ, Nock BA, Maina T, Gibson V, Ellison D, Murray I, et al. GRP receptor imaging of prostate cancer using [(99m)Tc]Demobesin 4: a first-in-man study. Mol Imaging Biol. 2014;16(6):888–95. doi:10.1007/s11307-014-0754-z.
Pfister D, Porres D, Heidenreich A, Heidegger I, Knuechel R, Steib F, et al. Detection of recurrent prostate cancer lesions before salvage lymphadenectomy is more accurate with (68)Ga-PSMA-HBED-CC than with (18)F-Fluoroethylcholine PET/CT. Eur J Nucl Med Mol Imaging. 2016;43(8):1410–7. doi:10.1007/s00259-016-3366-9.
Rigatti P, Suardi N, Briganti A. Pelvic/retroperitoneal salvage lymph node dissection for patients treated with radical prostatectomy with biochemical recurrence and nodal recurrence detected by [11C]choline positron emission tomography/computed tomography. Eur Urol. 2011;60(5):935–43. doi:10.1016/j.eururo.2011.07.060.
Acknowledgements
We thank Piramal Imaging for providing the precursor to support this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was reviewed and approved by the local Ethics Committee (N° 562/15). Informed consent was obtained from all individual participants included in the study.
Disclosure / conflict of interest
CAJ, GW, IP, HCR, VD, UW, WSS, MB, ALG and RM declared that no competing interests or financial disclosures exist. PTM received financial support for ongoing research by GE and Piramal Imaging WAW received study support for ongoing research by Piramal Imaging, Endocyte and Ipsen Pharmaceuticals.
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Wieser, G., Popp, I., Christian Rischke, H. et al. Diagnosis of recurrent prostate cancer with PET/CT imaging using the gastrin-releasing peptide receptor antagonist 68Ga-RM2: Preliminary results in patients with negative or inconclusive [18F]Fluoroethylcholine-PET/CT. Eur J Nucl Med Mol Imaging 44, 1463–1472 (2017). https://doi.org/10.1007/s00259-017-3702-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3702-8