Abstract
Purpose
The goal of this study is to determine the technical accuracy of segmental perfusion parameters assessed with quantitative cardiac PET imaging in the evaluation of coronary artery disease (CAD) in patients with stable angina.
Methods
A cohort of patients who participated in the EVINCI protocol underwent an evaluation of coronary anatomy by invasive coronary angiography (ICA) and/or coronary computed tomography angiography (CCTA) and PET myocardial perfusion imaging with H2 15O, 13NH3 or 82Rb. PET studies were analyzed by two independent observers blinded to clinical and instrumental data, and classified as positive or negative for significant CAD using only segmental perfusion measurements and cut-off values from literature.
Results
On a per-patient basis, the overall inter-observer agreement on PET results was 90 % (kappa = 0.79), indicating substantial agreement. On a per-vessel basis, the inter-observer agreement on PET results was 88 % (kappa = 0.74) in the RCA territory, 94 % (kappa = 0.84) in the LAD territory and 94 % (kappa = 0.85) in the LCX territory.
Segmental PET measurements correctly identified 85 % of the patients, resulting in a global sensitivity of 86 %, a specificity of 84 %, a positive predictive value (PPV) of 69 % and a negative predictive value (NPV) of 93 %.
In vessel-based analyses, quantitative perfusion parameters had a sensitivity, specificity, PPV and NPV of 92 %, 82 %, 42 % and 99 %, respectively, for the detection of significant coronary stenoses in all major coronary arteries.
Conclusions
The assessment of absolute myocardial perfusion parameters measured at a segment level lead to reliable and accurate identification of patients with significant coronary stenosis at ICA and/or CCTA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent years have witnessed the increasing diffusion of cardiac positron emission tomography (PET) for myocardial perfusion imaging. With tracers like 15O-water (H2 15O), 13N-ammonia (13NH3) and 82Rubidium (82Rb) [1–4], cardiac PET has gained acceptance in the detection of physiologic severity of coronary artery disease (CAD) and microcirculatory impairment, which both represent important information with regards to patient treatment and risk stratification [5–10].
One of the major advantages of cardiac PET is its ability to quantify myocardial blood flow (MBF) at rest and during stress in absolute terms (ml/g/min) and thus to calculate the myocardial flow reserve (MFR) [6, 11]. The availability of reliable tracer kinetic models and several software packages has enabled this kind of measurement quickly and accurately also in clinical routine practice [11, 12]. Non-invasive MBF and MFR quantification is currently considered part of a comprehensive approach to evaluate CAD, improving the identification of early-stage disease, microvascular dysfunction and multivessel CAD, and also improving the characterization of CAD burden [6, 13–15].
Recent studies have shown the incremental diagnostic value of quantitative MBF measurements as an adjunct to the visual analysis of cardiac PET images, in demonstrating the perfusion defect area [5, 6, 13–17].
With all perfusion tracers, MBF quantification with cardiac PET has always demonstrated good repeatability [18–20] and reproducibility [12, 19, 21–24]. Moreover, MBF and MFR measurements have shown great diagnostic performance in predicting significant CAD, with levels of sensitivity and specificity higher than 85 % [5, 17, 25, 26].
The goal of our study is to determine the accuracy of segmental MBF/MFR measurements assessed with quantitative cardiac PET imaging in the evaluation of CAD in a cohort of patients that participated to the Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischaemic Heart Disease (EVINCI) study [27]. The peculiarity of this study is that the diagnostic accuracy of absolute segmental MBF/MFR values was assessed blinded to patients’ clinical data and to visual analysis of PET images, using MBF/MRF cut-off values from literature, by two independent observers, in order to evaluate both the inter-observer reproducibility of clinical decisions and the objective performance of MBF/MFR segmental values independently of clinical information.
Methods
Patients
All patients included in this study participated in the EVINCI study, which prospectively enrolled patients with intermediate probability of CAD (20–90 %) [27]. All patients’ data were anonymised.
PET image acquisition and analysis
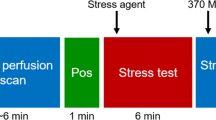
Image acquisition procedures were based on international guidelines [28], defined by the PET core lab centers and implemented throughout the consortium prior to the beginning of the study [27].
PET data were analyzed with the cardiac PET modeling software package (PCARDP) available in PMOD (PMOD version 3.5, PMOD Technologies, Zurich, Switzerland). MBF at rest and during stress was calculated from model fitting of the arterial input function and tissue time–activity curve, according to the correct method for each tracer; in particular, the Hermannsen et al. method was used for H2 15O PET processing [29], the de Grado et al. method for 13NH3 PET processing [22, 30] and the Lortie et al. method for 82Rb PET processing [31]. The left ventricular wall was divided into 17 segments: septal (apical septal, midinferoseptal, midanteroseptal, basal inferoseptal and basal anteroseptal), anterior (apical anterior, midanter- ior and basal anterior), lateral (apical lateral, midlateral and basal lateral), inferior (apical inferior, midinferolateral, midinferior, basal inferolateral and basal inferior) and apical [32]. MFR was calculated as the ratio of stress MBF to rest MBF.
All PET images were analyzed by two independent, expert observers (R.S., V.B.), who, at the time of PET analysis, were completely unaware of the patients’ demographic, clinical and instrumental data.
Myocardial perfusion PET studies were classified as positive or negative for significant CAD solely on the basis of segmental MBF/MFR measurements, without visual analysis of PET images and without considering global or regional values. Such classification was performed according to criteria derived from the most established literature for each tracer. Regarding H2 15O, PET studies were considered positive for significant CAD when more than one contiguous segment showed stress MBF comprised between 2.0 and 2.3 ml/g/min or if at least one segment showed stress MBF <2.0 ml/g/min [26]. For 13NH3, PET studies were considered positive when more than one contiguous segment showed stress MBF <1.85 ml/g/min or when at least one segment showed stress MBF < 1.85 ml/g/min and MFR < 2.0 [5, 17]. Regarding 82Rb, PET studies were considered positive if at least one segment showed MFR <1.7 [33, 34].
For H2 15O and 13NH3, these literature cut-offs were confirmed by receiver operating characteristic (ROC) curve analysis in the present study. In particular, the H2 15O cut-off was stress MBF < 2.05 ml/mg/min, and the 13NH3 cut-offs were stress MBF < 1.79 ml/g/min and MFR < 2.06. Therefore, the cut-offs derived from literature were used at a segment level for both the per-patient and the per-vessel analyses. The attribution of each segment to vascular territory was based on standard assumptions [32].
Coronary anatomy study
Coronary anatomy was evaluated by coronary computed tomography angiography (CCTA) or invasive coronary angiography (ICA). Both procedures were performed according to international guidelines [35], defined by the CCTA and ICA core lab centers and implemented throughout the EVINCI consortium prior to the beginning of the study [27].
The positivity or negativity of ICA and CCTA examinations were defined by the respective core-lab centers, according to the EVINCI protocol [27]. In brief, at ICA, coronary stenoses were considered significant when occurring in at least one major coronary artery (left main, left anterior descending [LAD], left circumflex [LCX] and right coronary [RCA] arteries) with a reduction in lumen diameter >50 % in the left main stem or >70 % elsewhere or between 30 % and 70 % with a fractional flow reserve (FFR) ≤ 0.80. At CCTA, the examinations were considered abnormal if at least one major coronary artery had a diameter stenosis >50 %.
Statistical analysis
Quantitative variables were expressed as mean ± standard deviation (SD), and categorical variables as percentages. Inter-observer agreement has been assessed as percentage of concordant PET results and using the kappa statistic. A P value of less than 0.05 was considered statistically significant. SPSS 22 software was used for statistical analysis.
Results
Description of the population
A total of 126 patients (Table 1) underwent myocardial perfusion imaging by PET and images were available and suitable for the analyses. Of them, 77 patients underwent cardiac PET with H2 15O, 42 patients with 13NH3 and 7 patients with 82Rb. These patients were included in the evaluation of inter-observer agreement.
Of all 126 subjects, 5 patients had nor CCTA neither ICA results available, 23 patients had a positive CCTA result but no ICA result to confirm it, 13 patients had a negative CCTA result (no ICA) [36] and for the remaining 85 patients, ICA results were available. The final analysis on diagnostic accuracy included only patients for which cardiac PET measurements and either ICA result (N = 85) or a negative CCTA result (N = 13, in consideration of the high NPV of CCTA) [36] were available. Therefore, 98 patients (Table 1) were included in the final analysis on diagnostic accuracy, consisting of 73 subjects with H2 15O PET and 25 subjects with 13NH3 PET (no subject with 82Rb PET). Among them, obstructive CAD was diagnosed at ICA in 29 (30 %) patients, while non-obstructive CAD (at CCTA or ICA) was observed in 69 (70 %) patients.
Inter-observer agreement
Patient-based analysis
Overall, the inter-observer agreement on PET results was 90 %, with a kappa of 0.79, which indicates substantial agreement. In particular, the inter-observer agreement (and kappa coefficients) on H2 15O, 13NH3 and 82Rb PET results were, respectively, 86 % (k = 0.71), 95 % (k = 0.89) and 100 % (k = 1), indicating, respectively, substantial, almost perfect and perfect agreements. The observational data of the two observers are shown in Table 2.
Vessel-based analysis
The overall inter-observer agreement on PET results was 88 % (kappa of 0.74) in the RCA territory, 94 % (kappa of 0.84) in the LAD territory and 94 % (kappa of 0.85) in the LCX territory.
The detailed inter-observer agreement and kappa coefficients on H2 15O, 13NH3 and 82Rb PET results for all vascular territories are shown in Table 3.
Diagnostic accuracy
Patient-based analysis
Segmental MBF PET measurements correctly identified 83 (85 %) patients with significant coronary artery stenoses at ICA or without significant stenoses either at CCTA or ICA, resulting in a global sensitivity of 86 %, a specificity of 84 %, a PPV of 69 % and an NPV of 93 % (Fig. 1).
Considering MBF measurements derived from H2 15O PET, segmental parameters correctly classified a total of 64 (88 %) patients with significant coronary stenoses at ICA or without significant stenoses either at CCTA or ICA, of which 21 of the 22 patients had positive findings and 43 of the 51 had negative findings. Quantitative analysis with H2 15O resulted in a sensitivity of 95 %, a specificity of 84 %, a PPV of 72 % and an NPV of 98 % (Fig. 1). Considering MBF derived from 13NH3 PET, segmental parameters correctly classified a total of 19 (76 %) patients with significant coronary stenoses at ICA or without significant stenoses either at CCTA or ICA, of which 4 of the 7 had positive findings, and 15 of the 18 patients had negative findings. Quantitative analysis with 13NH3 resulted in a sensitivity of 57 %, a specificity of 83 %, a PPV of 57 % and an NPV of 83 % (Fig. 1).
Vessel-based analysis
In vessel-based analyses, overall quantitative MBF had a sensitivity of 92 %, a specificity of 82 %, a PPV of 42 % and an NPV of 99 % for the detection of significant coronary stenoses in all major coronary arteries. Sensitivity, specificity and predictive values for quantitative parameters derived from H2 15O and 13NH3 in each vascular territory are shown in Table 4 and Fig. 2.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy on a per-vessel basis of segmental quantitative PET perfusion parameters. Legend – 13NH3: 13N-ammonia; H2 15O: 15O-water; LAD: left anterior descending artery; LCX: left circumflex artery; NPV: negative predictive value; PPV: positive predictive value; RCA: right coronary artery
Discussion
The present study was conducted to evaluate the reliability and technical accuracy of PET-derived segmental MBF and MFR measurements to detect significant obstructive CAD in the particular and unfavourable condition of knowing solely the quantitative data, in order to test their performance by themselves and not filtered by clinical interpretations. PET perfusion values were calculated by two independent observers, blinded to demographic and clinical data, and examinations were classified as positive or negative according to cut-off values suggested throughout the literature [5, 17, 26, 33, 34].
Overall, classification of PET examinations from segmental perfusion values provided reliable results, with an inter-rater agreement from substantial to almost perfect at both patient- and vessel-level analyses. This result is in line with previous findings [5], and suggests that, even if segmental parameters may seem more variable and thus less reproducible than regional or global values, the diagnostic classification derived from them proved to be very reliable.
Segmental MBF/MFR measurements provided an accuracy of 85 % to classify patients with or without significant CAD. Besides, also the vessel-level analysis yielded good accuracy (83 %), with overall sensitivity and specificity of 92 % and 82 %, respectively.
In clinical practice, quantitative PET myocardial perfusion imaging has been demonstrated as a useful tool for the detection of significant CAD. Quantitative MBF values integrate and enhance the qualitative assessment of myocardial perfusion imaging [5, 9, 13, 14, 17, 25, 26]. Traditionally, MBF rest values are also corrected for blood pressure and cardiac rate at the moment of the examination, specifically in order to avoid overestimation in anxious or overly excited patients, with consequent undue decrease in MFR. Conversely, our study assesses the reliability and accuracy of MBF/MFR values by themselves and without any of these possible corrective factors. In spite of this, our results show levels of accuracy, sensitivity and specificity greater than 80 %, which mirrors previously published studies that demonstrated sensitivity and specificity ranging from 76 % to 96 %, and from 80 % to 90 %, respectively [5, 6, 25, 26, 37, 38]. Our findings suggest segmental values by themselves represent a robust and reliable measurement.
Our levels of sensitivity both on a per-patient (86 %) and on a per-vessel basis (92 %) are higher than that reported in other similar studies [5], suggesting that the use of segmental values could be suitable to highlight subtle alterations that, with global values, would be otherwise missed.
Among patients with significant stenosis at ICA, only 4 % were not correctly classified by quantitative perfusion parameters (1/73 for H2 15O PET, 3/25 on 13NH3 PET). On a per-vessel analysis, quantitative values did not correctly identify only 3 of the 37 significantly stenotic vessels (8 %).
Interestingly, the NPV is very high in both patient- and vessel-level analyses, confirming the important role of quantitative PET in ruling out obstructive CAD [26]. However, the PPV is rather low in all analyses, suggesting that the presence of a positive PET examination (according to the cut-offs in literature) does not necessarily stand for flow-limiting CAD. This finding is in line with previous studies [26], and reflects the well-known discrepancy between the impairment in myocardial perfusion and the presence of epicardial disease. Such a mismatch could not represent the presence of real false positive results, but more likely represents the effects of coronary microvascular disease and/or non critical atherosclerotic lesions on myocardial perfusion as measured by PET [15, 39]. It is well know that coronary stenosis (even with FFR measurement) and perfusion provide different and complementary information, which could be discordant [40–42].
One of the strengths of our study is the inclusion of subjects from the EVINCI study, which is a large multicenter European study designed to compare the diagnostic accuracy of noninvasive anatomic and functional imaging in identifying patients with significant CAD defined by ICA. PET examinations were performed with different PET perfusion tracers, thus enabling us to evaluate diagnostic performance with all available tracers, considered together and separately.
Another strength of the present study is the fact that all PET examinations have been evaluated by two independent observers that were unaware of both clinical and CTA/ICA information. This ensures that all measurements were performed objectively and no subjective interpretation has been applied to the results; thus, the accuracy values are related on the performance of only segmental MBF/MFR quantitative parameters.
This study has some limitations. The decision to not be aware of patients’ clinical and instrumental data and thus to not consider confounding factors could be a limitation of this study, leading us to be too conservative in the results. Previous studies have shown MBF is related to age, sex and several CAD risk factors; so, the choice to not consider these data in the interpretation could have lowered the accuracy values [26, 43]. Besides, the choice to not visually evaluate PET images could have limited the capacity to test the incremental value of quantitative MBF/MFR measurements over visual or semiquantitative evaluation. However, our goal was to determine the real reliability and performance of PET segmental quantitative parameters “per se”, without the added value of subjective clinician interpretation, and we found that even in this unfavourable situation the levels of accuracy remain high.
The selection of cut-off values from the literature is a critical point to be addressed. We choose, to the best of our knowledge, cut-off values derived from the most ascertained works in the literature for each tracer. In some cases (H2 15O, 13NH3), cut-off values derived from numerous populations could be retrieved [17, 26] and they were confirmed by post-hoc ROC curve analysis in the present studies. In other cases (82Rb), more variable data were found. We choose the most used threshold for CAD, which is MFR < 1.7 for positivity [33, 34], and not a threshold of stress MBF. However, even though we had chosen a stress MBF threshold [34], our results would not have changed. Naturally, since for the 82Rb patients we had no angiographic data available for comparison, in this particular group, the interobserver classification agreement does not imply an accurate diagnosis of obstructive CAD.
Another limitation could be the fact that 13 patients with negative CCTA included in this analysis were not referred to ICA. Actually, according to the EVINCI protocol, these patients should have had also negative functional stress tests for regional ischemia. All these patients had no regional perfusion defects at qualitative PET and also negative stress echocardiography or stress magnetic resonance results.
Moreover, the limited number of patients with positive ICA, especially in the subgroup who underwent 13NH3 PET, could be a potential limitation, and may have contributed to lower sensitivity and PPV. Finally, the vessel-level analysis has been conducted under the assumption of standard vascular territory distribution. This assumption could have led to less accurate assignment of segmental perfusion alteration to culprit vessels, given the morphologic variability of the coronary tree [44].
Conclusions
Quantitative measurements of MBF and MFR parameters with cardiac PET represent a valuable tool for clinical practice to better identify patients with functionally relevant coronary stenoses. Such measurements could have great impact on decision-making and on patients’ risk stratification. This is the first study to assess the performance of absolute quantitative perfusion parameters isolated from clinical information in order to assess their technical reliability. We demonstrated that the assessment of MBFs and MFR absolute values at a segment level lead to reliable and accurate identification of patients with significant coronary stenosis at ICA. This could represent a further step toward the use of quantitative PET myocardial perfusion imaging in clinical practice.
References
deKemp RA, Ruddy TD, Hewitt T, Dalipaj MM, Beanlands R. Detection of serial changes in absolute myocardial perfusion with Rb-82 PET. J Nucl Med. 2000;41:1426–35.
Kuhle WG, Porenta G, Huang SC, Buxton D, Gambhir SS, Hansen H, et al. Quantification of regional myocardial blood-flow using N-13 ammonia and reoriented dynamic positron emission tomographic imaging. Circulation. 1992;86:1004–17.
DiCarli M, Czernin J, Hoh CK, Gerbaudo VH, Brunken RC, Huang SC, et al. Relation among stenosis severity, myocardial blood-flow, and flow reserve in patients with coronary-artery disease. Circulation. 1995;91:1944–51.
Ahn JY, Lee DS, Lee JS, Kim SK, Cheon GJ, Yeo JS, et al. Quantification of regional myocardial blood flow using dynamic H2(15)O PET and factor analysis. J Nucl Med. 2001;42:782–7.
Fiechter M, Ghadri JR, Gebhard C, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Diagnostic value of 13N-ammonia myocardial perfusion PET: added value of myocardial flow reserve. J Nucl Med. 2012;53:1230–4.
Schindler TH, Schelbert HR, Quercioli A, Dilsizian V. Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging. 2010;3:623–40.
Schindler TH, Quercioli A, Valenta I, Ambrosio G, Wahl RL, Dilsizian V. Quantitative assessment of myocardial blood flow—clinical and research applications. Semin Nucl Med. 2014;44:274–93.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography: added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150–6.
Dorbala S, Di Carli MF. Cardiac PET perfusion: prognosis, risk stratification, and clinical management. Semin Nucl Med. 2014;44:344–57.
Neglia D, Michelassi C, Trivieri MG, Sambuceti G, Giorgetti A, Pratali L, et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation. 2002;105:186–93.
Saraste A, Kajander S, Han C, Nesterov SV, Knuuti J. PET: is myocardial flow quantification a clinical reality? J Nucl Cardiol. 2012;19:1044–59.
Nesterov SV, Deshayes E, Sciagrà R, Settimo L, Declerck JM, Pan X-B, et al. Quantification of myocardial blood flow in absolute terms using 82Rb PET imaging - results of RUBY-10 study. JACC Cardiovasc Imaging. 2014;7:1119–27.
Yoshinaga K, Katoh C, Manabe O, Klein R, Naya M, Sakakibara M, et al. Incremental diagnostic value of regional myocardial blood flow quantification over relative perfusion imaging with generator-produced rubidium-82 PET. Circ J. 2011;75:2628–34.
Kajander SA, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, et al. Clinical value of absolute quantification of myocardial perfusion with 15O-water in coronary artery disease. Circ Cardiovasc Imaging. 2011;4:678–84.
Liga R, Marini C, Coceani M, Filidei E, Schlueter M, Bianchi M, et al. Structural abnormalities of the coronary arterial wall--in addition to luminal narrowing--affect myocardial blood flow reserve. J Nucl Med. 2011;52:1704–12.
Parkash R, deKemp RA, Ruddy TD, Kitsikis A, Beauschene L, Williams K, et al. Potential utility of rubidium 82 PET quantification in patients with 3-vessel coronary artery disease. J Nucl Cardiol. 2004;11:440–9.
Hajjiri MM, Leavitt MB, Zheng H, Spooner AE, Fischman AJ, Gewirtz H. Comparison of positron emission tomography measurement of adenosine-stimulated absolute myocardial blood flow versus relative myocardial tracer content for physiological assessment of coronary artery stenosis severity and location. JACC Cardiovasc Imaging. 2009;2:751–8.
Kaufmann PA, Gnecchi-Ruscone T, Yap JT, Rimoldi O, Camici PG. Assessment of the reproducibility of baseline and hyperemic myocardial blood flow measurements with 15O-labeled water and PET. J Nucl Med. 1999;40:1848–56.
El Fakhri G, Kardan A, Sitek A, Dorbala S, Abi-Hatem N, Lahoud Y, et al. Reproducibility and accuracy of quantitative myocardial blood flow assessment with 82Rb PET: comparison with 13N-ammonia PET. J Nucl Med. 2009;50:1062–71.
Schindler TH, Zhang X-L, Prior JO, Cadenas J, Dahlbom M, Sayre J, et al. Assessment of intra- and interobserver reproducibility of rest and cold pressor test-stimulated myocardial blood flow with 13N-ammonia and PET. Eur J Nucl Med Mol Imaging. 2007;34:1178–88.
Harms HJ, Nesterov SV, Han C, Danad I, Leonora R, Raijmakers PG, et al. Comparison of clinical non-commercial tools for automated quantification of myocardial blood flow using oxygen-15-labelled water PET/CT. Eur Heart J Cardiovasc Imaging. 2014;15:431–41.
Slomka PJ, Alexanderson E, Jacome R, Jimenez M, Romero E, Meave A, et al. Comparison of clinical tools for measurements of regional stress and rest myocardial blood flow assessed with 13N-ammonia PET/CT. J Nucl Med. 2012;53:171–81.
Nitzsche EU, Choi Y, Czernin J, Hoh CK, Huang SC, Schelbert HR. Noninvasive quantification of myocardial blood flow in humans. A direct comparison of the [13N]ammonia and the [15O]water techniques. Circulation. 1996;93:2000–6.
Prior JO, Allenbach G, Valenta I, Kosinski M, Burger C, Verdun FR, et al. Quantification of myocardial blood flow with 82Rb positron emission tomography: clinical validation with 15O-water. Eur J Nucl Med Mol Imaging. 2012;39:1037–47.
Kajander S, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, et al. Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122:603–13.
Danad I, Uusitalo V, Kero T, Saraste A, Raijmakers PG, Lammertsma AA, et al. Quantitative assessment ofmyocardial perfusion in the detection of significant coronary artery disease. J Am Coll Cardiol. 2014;64:1464–75.
Neglia D, Rovai D, Caselli C, Pietilä M, Teresinska A, Aguadé-Bruix S, et al. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015. doi:10.1161/CIRCIMAGING.114.002179.
Hesse B, Tagil K, Cuocolo A, Anagnostopoulos C, Bardies M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging. 2005;32:855–97.
Hermansen F, Rosen SD, Fath-Ordoubadi F, Kooner JS, Clark JC, Camici PG, et al. Measurement of myocardial blood flow with oxygen-15 labelled water: comparison of different administration protocols. Eur J Nucl Med Mol Imaging. 1998;25:751–9.
DeGrado T, Hanson M, Turkington T, DeLong D, Brezinski D, Vallee J, et al. Estimation of myocardial blood flow for longitudinal studies with 13N-labeled ammonia and positron emission tomography1. J Nucl Cardiol. 1996;3:494–507.
Lortie M, Beanlands RSB, Yoshinaga K, Klein R, DaSilva JN, deKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging. 2007;34:1765–74.
Cerqueira MD. Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart: A Statement for Healthcare Professionals From the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Anagnostopoulos C, Almonacid A, El Fakhri G, Curillova Z, Sitek A, Roughton M, et al. Quantitative relationship between coronary vasodilator reserve assessed by 82Rb PET imaging and coronary artery stenosis severity. Eur J Nucl Med Mol Imaging. 2008;35:1593–601.
Johnson NP, Gould KL. Physiological basis for Angina and ST-segment change. JACC Cardiovasc Imaging. 2011;4:990–8.
Bluemke DA, Achenbach S, Budoff M, Gerber TC, Gersh B, Hillis LD, et al. Noninvasive coronary artery Imaging - Magnetic resonance angiography and multidetector computed tomography angiography - A scientific statement from the American Heart Association Committee on cardiovascular imaging and intervention of the council on cardiovascular radiology and intervention, and the councils on clinical cardiology and cardiovascular disease in the young. Circulation. 2008;118:586–606.
Chow BJW, Abraham A, Wells GA, Chen L, Ruddy TD, Yam Y, et al. Diagnostic accuracy and impact of computed tomographic coronary angiography on utilization of invasive coronary angiography. Circ Cardiovasc Imaging. 2009;2:16–23.
Sciagrà R. Quantitative cardiac positron emission tomography: the time is coming! Scientifica. 2012;2012:1–16.
Danad I, Raijmakers PG, Appelman YE, Harms HJ, de Haan S, van den Oever MLP, et al. Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2012;54:55–63.
Neglia D, L'Abbate A. Myocardial perfusion reserve in ischemic heart disease. J Nucl Med. 2009;50:175–7.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. J Am Coll Cardiol. 2013;62:1639–53.
Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc Imaging. 2012;5:193–202.
Reddy KG, Nair RN, Sheehan HM, Hodgson JM. Evidence that selective endothelial dysfunction may occur in the absence of angiographic or ultrasound atherosclerosis in patients with risk factors for atherosclerosis. J Am Coll Cardiol. 1994;23:833–43.
Czernin J, Muller P, Chan S, Brunken RC, Porenta G, Krivokapich J, et al. Influence of age and hemodynamics on myocardial blood-flow and flow reserve. Circulation. 1993;88:62–9.
Javadi MS, Lautamäki R, Merrill J, Voicu C, Epley W, McBride G, et al. Definition of vascular territories on myocardial perfusion images by integration with true coronary anatomy: a hybrid PET/CT analysis. J Nucl Med. 2010;51:198–203.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Information on grants and other forms of financial support
This work was supported by a grant from the European Union FP7- CP-FP506 2007 (grant agreement no. 222915, EVINCI [Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischemic Heart Disease]). It was also supported in part by the Centre of Excellence in Molecular Imaging in Cardiovascular and Metabolic Research, the Academy of Finland, the Cardiovascular Biomedical Research Unit of the Royal Brompton & Harefield National Health Service Foundation Trust, the National Institute for Health Research Cardiovascular Biomedical Research Unit at St Bartholomew’s Hospital, the Ministry of Science and Higher Education, Poland and unrestricted grants and products from General Electric Healthcare. This work forms part of the research themes contributing to the translational research portfolio of the NIHR Cardiovascular Biomedical Research Unit at Barts, which is supported and funded by the National Institute for Health Research.
All authors had no relationship with industry and financial associations from within the past 2 years that might pose a conflict of interest in connection with the submitted article.
All procedures have been approved by the appropriate institutional and/or national research ethics committee and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Berti, V., Sciagrà, R., Neglia, D. et al. Segmental quantitative myocardial perfusion with PET for the detection of significant coronary artery disease in patients with stable angina. Eur J Nucl Med Mol Imaging 43, 1522–1529 (2016). https://doi.org/10.1007/s00259-016-3362-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-016-3362-0