Abstract
Purpose
To report 5-year outcomes of a prospective registry study investigating posttherapy FDG PET/CT in women with locally advanced cervical cancer. A secondary analysis assessing the prognostic significance of HPV infection was performed.
Methods
Patients underwent definitive chemoradiation followed by a single FDG PET/CT scan for response assessment. A complete metabolic response (CMR) was defined as no evidence of FDG-avid disease. Patients were dichotomized according to HPV infection status into a ‘higher-risk’ group and a ‘lower-risk’ group, with the higher-risk group comprising those with alpha-7 strain HPV (subtypes 18, 39 and 45) and those who were HPV-negative and the lower-risk group comprising those with alpha-9 strain HPV (subtypes 16, 31, 33, 52 and 58) and those with mixed strains. Survival outcomes, patterns of failure and salvage therapy outcomes were investigated for their association with metabolic response and HPV status.
Results
In 105 patients the median prospective follow-up was 5.2 years. The 5-year cancer-specific, overall and progression-free survival rates in patients with a CMR were 97 %, 93 % and 86 %, respectively. In patients without a CMR, the corresponding 5-year survival rates were 36 %, 22 % and 0 % respectively (p < 0.01). PET response was associated with patterns of failure (p < 0.01), with the 5-year freedom from local, nodal and distant failure in patients with a CMR being 94 %, 90 % and 94 %, respectively. Of 16 patients who underwent salvage therapy, 12 had disease detected on the surveillance PET scan, and 8 achieved a post-salvage CMR of whom all were alive at a median of 4.9 years. DNA adequate for HPV analysis was extracted in 68 patients. The likelihood of a PET metabolic response was not influenced by HPV infection status, with 71 % and 75 % of higher-risk and lower-risk patients, respectively, achieving CMR (p = 0.83). Higher-risk patients had a poorer OS (HR 2.6, range 1.0 – 6.6, p = 0.05) in univariable analysis but not multivariable analysis (p = 0.11).
Conclusion
At 5 years CMR remains a powerful factor predicting survival after initial and salvage therapy. Metabolic response was not associated with HPV infection risk. Further studies are required to establish the association with HPV infection risk and survival after chemoradiation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Uterine cervical cancer continues to present a considerable burden of disease in the modern era, particularly in the developing world. It is the second most common malignancy in women by incidence [1], and accounts for 150,000 deaths annually [2]. Definitive chemoradiation is a standard treatment option for patients with locally advanced disease [3]. In this setting, posttherapy response on 18F-FDG PET scanning has been reported by our group and others to independently predict patient outcomes after chemoradiation [4–7]. Infection with specific subtypes of human papilloma virus (HPV) has been suggested to be of prognostic significance in patients treated with radiotherapy. In a recent study in 1,010 Taiwanese patients treated with radiotherapy (with or without chemotherapy), gene-chip analysis showed a significant association between HPV subtype and survival [8]. Patients infected with the alpha-7 strain of HPV (subtypes 18, 39 and 45) and those who were HPV-negative had a significantly higher risk of death than patients infected with the alpha-9 strain of HPV (subtypes 16, 31, 33, 52 and 58) and those with mixed infections. We hypothesized that a Caucasian population undergoing chemoradiation therapy might show a similar pattern of risk based on HPV infection status.
The purpose of this study was to report the long-term 5-year survival outcomes and patterns of failure in our previously reported cohort of patients who underwent posttherapy FDG PET/CT scanning after chemoradiation for locally advanced cervical cancer [6]. Additionally, we report a post-hoc analysis of the impact of pretreatment HPV infection status on patient outcomes and the association between HPV status and metabolic response.
Materials and methods
This research was performed in accordance of the ethical standards of the Peter MacCallum Cancer Centre institutional review board. Patients with locally advanced cervical cancer treated with chemoradiation therapy were enrolled into an institutional tumour registry from January 2002 to June 2007. Patient characteristics, staging, treatment, toxicities and follow-up details were prospectively recorded in our institutional database. Irradiation techniques have been previously described [6]. In brief, conventionally fractionated external beam radiotherapy was planned to 40 – 45 Gy to the pelvis with a nodal boost of 6 – 10 Gy or 5.4 – 9 Gy as required depending on nodal location and volume, with four to six cycles of weekly concurrent cisplatin chemotherapy at a dose of 40 mg/m2. A four-field box technique was used with corner shielding to reduce the dose to the intestine and rectum. Within 10 days of completion, a high dose-rate intracavitary brachytherapy boost was delivered twice weekly to a dose of 28 Gy in four fractions (or equivalent to a total tumour dose of 80 Gy, EQD 2 Gy). The ultrasound-guided conformal brachytherapy plan was confirmed on planning MRI for the first fraction, and subsequent fractions were confirmed on transabdominal ultrasonography in the treatment position. In the salvage setting, out-of-field recurrences were treated with 54 Gy of combined chemoradiation therapy and in-field local recurrences, where possible, were salvaged by hysterectomy.
All patients had histologically confirmed carcinoma of the uterine cervix, FIGO stage Ib to IVa and ECOG performance status 2 or less. Pretreatment assessment included pelvic examination under anaesthesia, whole-body FDG PET/CT, MRI of the pelvis and routine blood counts. Clinical follow-up of patients including thorough medical history and physical examination was performed 4 weeks after therapy, 3-monthly until 2 years after therapy, 6 monthly in years 3, 4 and 5, then yearly thereafter.
FDG PET/CT scans were performed using a GE Discovery LS or a GE Discovery STE dedicated PET/CT scanner with four-slice and eight-slice multidetector CT (MDCT), respectively (GE Medical Systems, Milwaukee, WI). Patients fasted for at least 6 h prior to intravenous injection of 370 MBq of 18F-FDG. Patients were routinely catheterized, hydrated, and diuresed. Posttherapy FDG PET/CT was performed between 3 and 6 months after completion of chemoradiation therapy. Metabolic changes after therapy were scored in a validated semiquantitative system as a complete metabolic response (CMR), a partial metabolic response (PMR) or progressive metabolic disease (PMD), as used in a previous study by our group [9]. In brief, a CMR was defined as no tracer uptake or the background level of FDG activity within the treated area of the disease, a PMR as residual FDG activity within the treated area of the disease, and PMD as increased intensity or distribution of FDG-avid disease. Post-irradiation inflammation was differentiated from residual tumour by pattern recognition of geographic regions of uptake demarcated by the high-dose treatment volume, an approach applied in previous studies by our group [10, 11].
A secondary retrospective analysis was performed to assess the prognostic significance of HPV infection status. HPV infection was determined by the PapType® HPV detection test (Genera Biosystems, Victoria, Australia) as previously described [12]. Briefly, all available formalin-fixed paraffin-embedded (FFPE) tumour blocks containing pretreatment biopsy samples were recalled. Sections were cut and assessed by a pathologist to determine tumour content, then DNA was extracted using a QIAamp DNA Blood mini kit (Qiagen, Valencia, CA). Extracted DNA was used in a PCR with general primers for detection of all HPV subtypes. The PCR reaction mix then hybridizes to HPV subtype-specific hybridization beads, which were analysed on a BD FACS array to determine the HPV status and specific subtype(s) of each sample. Patients were dichotomized according to HPV infection status into a ‘higher-risk’ group and a ‘lower-risk’ group as reported previously [13, 14], with the higher-risk group comprising those with alpha-7 strain HPV (subtypes 18, 39 and 45) and those who were HPV-negative and the lower-risk group comprising those with alpha-9 strain HPV (subtypes 16, 31, 33, 52 and 58) and those with mixed strains.
Statistical methods
Overall survival (OS), progression-free survival (PFS) and cancer-specific survival (CSS) estimates were obtained using Kaplan-Meier methods. The effects of candidate prognostic variables on OS were assessed using the log-rank test and Cox proportional hazards model. The candidate prognostic variables considered were pretreatment MRI-based tumour volume (continuous), FIGO stage (ordinal), metabolic response (CMR, PMR or PMD), number of nodes (categorized as 1, 2, 3 or 4+), node positivity (dichotomous) and the presence of uterine corpus invasion (dichotomous, yes/no). The associations between metabolic response on posttherapy FDG PET/CT and each of several failure types (local, nodal and distant) were tested using the exact log-rank test. In the subset analysis of patients with known HPV infection status, Kaplan-Meier curves were used to describe time to event outcomes (time to local failure, time to nodal failure, time to distant failure, PFS and OS) according to HPV status (higher risk vs. lower risk). The curves were compared using the exact log-rank test. Cox proportional hazards model was used to estimate the hazard ratio (HR) and corresponding 95 % confidence interval (CI) for HPV status and to adjust for possible confounding factors in the OS analysis. Associations between metabolic response and HPV infections were assessed using Barnard’s test. Barnard’s unconditional exact test is an alternative to Fisher’s conditional exact test. Barnard’s test is more powerful than Fisher’s exact test in the analysis of 2 × 2 contingency tables [15, 16]. In the HPV analysis, we assumed a prevalence of high-risk disease in 70 % of patients. A sample size of 105 would provide at least 80 % power to detect a difference in CMR rates between high-risk and low-risk infection of 30 % with 5 % alpha
Results
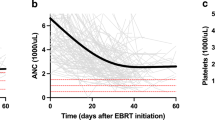
A total of 105 consecutive patients with a median follow-up of 5.19 years (range 1.4 – 8 years) were collected in the registry. Patient characteristics are presented in Table 1. The median time between the end of radiotherapy and the patient’s posttherapy PET scan was 4.9 months. At the time of posttherapy FDG PET/CT, 73 patients (70 %) had a CMR, 10 (9 %) had a PMR and 22 (21 %) had PMD. The 5-year OS and PFS rates were 72 % (95 % CI 64 – 81 %) and 60 % (95 % CI 51 – 70 %) in all patients, respectively. The corresponding OS and PFS rates in patients with a CMR were 93 % (95 % CI 87 – 99 %) and 86 % (95 % CI 51 – 70 %), respectively. Patients without a CMR had a much poorer survival (Fig. 1a), with a 5-year OS rate of only 22 % (95 % CI 11 – 44 %, p < 0.01). The 5-year CSS rate in patients with a CMR was 97 % (95 % CI 93 – 99 %) but only 26 % (95 % CI 13 – 51 %) in patients without a CMR (p < 0.01).
The univariable analysis for OS indicated that a metabolic response and a smaller MRI volume were associated with a better prognosis (p < 0.01). The risk of death in patients with a PMR was 19.58 times higher and in patients with PMD 19.46 times higher than in those with a CMR (Table 2). Node positivity was associated with OS with borderline significance (p = 0.06), whilst FIGO stage, number of involved nodes and uterine corpus invasion were not associated with survival. When assessed by multiple Cox regression using backwards elimination, metabolic response and smaller MRI volume remained statistically significant (p < 0.01 and p = 0.03, respectively). The HR of death in patients with PMR and PMD were 23.51 (95 % CI 7.35 – 75.19) and 21.17 (95 % CI 7.45 – 60.12), respectively.
Patterns of failure
There were 96 patients who had no distant disease on the posttherapy FDG PET/CT. Of these, 73 (76.0 %) had a CMR, 10 (10.4 %) had a PMR, and 13 (13.5 %) had PMD (in-field progressive FDG-activity within the cervix or pelvic nodes). In these patients without distant disease at posttherapy surveillance, the freedom from distant failure at 5 years was 84 % [95 % CI (76 – 92)], with strong evidence of an association between posttherapy metabolic response and distant failure rate (p < 0.01). Patients with a PMR had a hazard rate for distant failure 28 times (95 % CI [8 – 102]) the hazard rate of patients with a CMR (p < 0.01). Patients with a PMD had a hazard rate for distant failure 13 times (95 % CI [3 – 54]) the rate of patients with a CMR (p < 0.01). There were 84 patients who had no evidence of local cervical disease on the posttherapy FDG PET/CT. Of these, 73 (86.9 %) had a CMR, 4 (5.2 %) had a PMR, and 7 (8.3 %) had PMD. The freedom from local failure at 5 years in these patients was 94 % [95 % CIs (88 – 99)]. Of the 73 patients with a CMR, 4 patients had a local failure. In all cases this was the first site of failure, at a median time of 26.2 months. There were 77 patients that had no evidence of nodal or distant disease on the posttherapy PET. Of these 73 (94.8 %) had a CMR, and 4 (5.2 %) had a PMR (residual activity within the cervix). The freedom from nodal failure at 5 years in these patients was 88 % [95 % CIs (81 – 96)]. Patients with a posttherapy PMR had a hazard rate for nodal failure 77 times (95 % CI [9 – 916]) the hazard rate of patients with a CMR (p < 0.01). Figure 2 is a CONSORT style flow diagram showing the patterns of failure in the 105 included patients.
PET imaging in a patient with bulky primary cervical disease and bilateral iliac nodal involvement, including a right common iliac node (a) achieved a posttherapy CMR (b), but failed with an isolated para-aortic node 6 months later (c). She was subsequently salvaged with combined chemoradiation therapy to the para-aortic node, with a post-salvage CMR (d) and was alive without disease 6 years later at the time of reporting
Table 2 shows the univariable analysis of candidate prognostic factors for PFS on the subset of patients with CMR on posttherapy PET. Higher MRI volume and pretreatment node positivity were associated with poorer PFS in the univariable analysis (p < 0.01 and p = 0.01, respectively) and multivariable analysis (p < 0.01 for both). The HR for MRI volume in the multivariable analysis was 1.02 (95 % CI 1.01 – 1.03). Patients with involved nodes had a 11.33-fold increase in risk of progression per unit of time over patients without nodal involvement (95 % CI 2.04 – 62.81). In those patients with a CMR, freedom from local, nodal and distant failure at 5 years were 94 % (95 % CI 89 – 100 %), 90 % (95 % CI 83 – 97 %) and 94 % (95 % CI 89 – 100 %), respectively.
Salvage outcomes
A total of 18 patients had relapsed at a single site, of whom 16 had disease suitable for salvage treatment. The posttherapy PET scan detected the isolated residual disease in 12 of these 16 patients, whilst in the remaining 4 relapse was picked up by routine surveillance scans on later follow-up. Of the 16 patients undergoing salvage, 4 died at 1, 1.5, 1.8 and 2.5 years after the salvage therapy, with the remainder alive at the time of reporting. In 2 of these 16 patients, the isolated relapse was located in the cervix, and surgery in the form of hysterectomy or pelvic exenteration was used. In the remaining 14 patients, the site of relapse was in the lymph nodes, and definitive radiation (with or without concurrent chemotherapy) was used. The 2-year OS in patients undergoing salvage therapy was 78 % (95 % CI 58 – 100 %). The initial metabolic response in the 16 patients who subsequently underwent salvage therapy was CMR in 4, PMD in 8, and PMR in 4. All patients with an initial CMR were still alive at the time of reporting. A subset of 13 patients had a posttherapy PET scan for response assessment approximately 3 months after salvage chemoradiation therapy. Of these 13 patients, 8 achieved a post-salvage CMR with all 8 still alive at a median follow-up of 4.9 years. Figure 3 shows PET imaging in a patient in whom PET was used to guide the management of isolated nodal recurrence in the salvage setting.
HPV subgroup
FFPE pretreatment biopsy specimens were available in 70 patients, and DNA from 68 of these patients was extracted successfully for HPV PCR. Of these 68 patients, 5 (7.4 %) were HPV-negative, 12 (17.6 %) were infected with alpha-7 HPV strain (subtypes 18, 39 or 45), 46 (67.6 %) were infected with alpha-9 HPV strain (subtypes 16, 31, 33, 52 or 58) and 5 (7.4 %) had mixed alpha-7 and alpha-9 HPV infections. In total, 17 patients (25 %) were categorized as having ‘higher-risk’ HPV infection status and 51 (75 %) were categorized as having ‘lower-risk’ HPV infection status. In the higher-risk group, 12 patients (71 %) achieved a posttherapy CMR as compared to 38 patients (75 %) in the lower-risk group (difference of −4 % with 95 % CI −31 % to 18 %). The CMR rates did not appear to be different between the two groups (p = 0.83). Of the patients without a CMR, local failure on posttherapy PET was observed in three of the four patients (75 %) in the higher-risk HPV group, and in five of the eight patients (63 %) in the lower-risk HPV group (p = 0.29). Table 3 shows the time to event outcomes in the two HPV risk groups. OS curves in relation to infection status are shown in Fig. 1b. The OS analysis was repeated adjusting for MRI volume, FIGO stage, node positivity and uterine corpus invasion, and HPV status was not significantly associated with OS (p = 0.11).
Discussion
FDG PET scanning is a powerful and highly sensitive imaging modality in the staging of primary and recurrent cervical cancer [17]. The potential utility of posttherapy FDG PET is in the assessment of response to local therapy, the prediction of survival outcomes and the ability to inform early salvage procedures. Posttherapy FDG PET for response assessment, however, is not yet routinely recommended in the follow-up of patients with cervical cancer undergoing definitive chemoradiation therapy [18]. However, previous studies have demonstrated the impressive prognostic value of these scans. Grigsby et al. [4] reported a retrospective cohort of 152 women with a mean follow-up of 28 months in whom metabolic response after therapy was the most significant independent predictor of survival (p < 0.01). Women with no metabolic activity on posttherapy FDG PET/CT had a 5-year OS rate of 92 %, similar to our results showing a 5-year OS rate of 93 % in patients with a CMR. The authors further validated their findings in a prospective tumour registry of 92 patients [19], with a 3-year CSS rate of 96 % in patients with a CMR on posttherapy FDG PET/CT and 43 % in those without a CMR. These findings are also comparable with ours showing a 3-year CSS of 99 % in patients with a CMR and 44 % in those without. A recent retrospective study from Beriwal et al. [20] also investigated outcomes in patients with a posttherapy CMR. At a relatively short median follow-up of 15 months, the 3-year OS rate in 112 patients was 88 %.
In this study we found that FDG PET/CT also had prognostic utility in the assessment of patterns of failure and salvage therapy. Posttherapy PET response was strongly associated with risk of failure in this cohort, as patients with a CMR showed freedom from local, nodal and distant failure rates at 5 years of 94 %, 90 % and 94 %, respectively. In patients with isolated disease suitable for salvage therapy, clinical outcomes were very favourable. Definitive chemoradiation as a salvage therapy was used in the majority of the patients in this cohort (14 of 16). The detection of residual or recurrent disease on FDG PET/CT was critical to selection and planning of such therapy and the use of this modality provides a direct additional benefit in follow-up of such patients beyond those related to prognostic stratification. The 2-year OS in patients undergoing salvage therapy was 78 %. Interestingly, posttherapy response assessment using FDG PET/CT after salvage therapy appeared to be a similarly accurate predictor of survival. Of the 8 of 13 patients (61.5 %) who underwent posttherapy PET for response assessment and had a CMR, all 8 were still alive at a median follow-up of 4.9 years.
We also assessed the prognostic value of HPV infection status in this cohort. HPV infection is known to be a causative factor in cervical carcinoma. Over 100 HPV genotypes have been identified and classified in humans [21]. Evidence of HPV infection by subtypes 16 and 18 is found in approximately 70 % of patients with cervical cancer [22]. Two particular HPV species, alpha-7 (HPV 18, 39, 45, 59, 68 and 70) and alpha-9 (HPV 16, 31, 33, 35, 52, 58 and 67), have been found in over 80 % of all patients with cervical cancer. HPV infection status is postulated to directly influence the likelihood of response to chemoradiation therapy in other malignancies such as head and neck cancers [23, 24]. In our study, the likelihood of metabolic response was not different between the higher-risk HPV group (71 % CMR) and the lower-risk HPV group (75 % CMR, p = 0.83), and there was no significant difference in in-field metabolic control (p = 0.29). This suggests that the likelihood of in-field control after concurrent chemoradiation therapy may possibly not be related to HPV infection status in patients with cervical cancer. It may be that the high biological doses delivered with combination chemoradiation therapy and brachytherapy may potentially overcome any biological influence of HPV infection on local cervical tumour radiosensitivity. Whilst treatment de-escalation in patients with HPV-positive oropharyngeal cancer is presently an area of investigation in head and neck cancer [25], further work is required in the field of cervical cancer before this strategy can be adopted.
Several groups have investigated the association between HPV infection status and survival after radiation therapy alone (without concurrent chemotherapy) and have reported conflicting results [26–28]. The underlying mechanisms by which one species is more resistant to radiation therapy than another are yet to be fully elucidated. In vitro studies have revealed several features of HPV18 infection that differ from those of HPV16 infection, including enhanced E7 phosphorylation [29] and increased transformation [30]. Furthermore, HPV18 is associated with significantly less apoptosis than HPV16, affording one possible explanation for more radioresistant cervical cancer in patients with HPV18 infection [31]. Bachtiary et al. [26] investigated pretreatment biopsy samples from 106 Austrian women treated with radiotherapy alone and found that the presence of HPV infection with multiple subtypes in the same patient was inversely correlated with PFS (p < 0.01). By contrast, in two separate smaller Japanese cohorts of 84 patients from Osaka [27] and 40 patients from Gunma, no correlation between HPV infection subtype and survival after radiation therapy was noted. An analysis of 156 Taiwanese women [28] showed that HPV31 infection was associated with better survival after radiotherapy than infection with HPV16 or HPV18, and in turn HPV16 or HPV18 infection was associated with better survival than HPV58 infection.
The association between HPV infection and clinical outcomes following concurrent chemoradiation is not as well described. In a study of Taiwanese women by Wang et al. [32], 270 patients (26.7 %) underwent combined chemoradiation therapy. A significant association between HPV subtype (categorized as alpha-7 associated, alpha-9 associated, mixed and HPV-negative) and CSS was found. By comparison, in our study of 68 available specimens from a largely Caucasian patient cohort, there was a borderline significant association between HPV subgroup (alpha-7 and HPV-negative versus alpha-9 and mixed) in the univariable analysis (p = 0.05). This association was not statistically significant when accounting for other known prognostic variables (p = 0.11). Whilst the follow-up in this cohort was long at a median of 5.19 years, the power of our study was limited by the lower proportion of patients with viable DNA extracted (68 of 105) available for HPV subgroup analysis. A further weakness of this study was the variability in timing of posttherapy FDG PET (median 4.9 months). This reflected a change in practice at our institution from ordering posttherapy FDG PET from 3 to 4 months after therapy to 6 months after therapy during the study period. We hypothesize that this strategy may have reduced the likelihood of false-positive findings by ensuring adequate time for resolution of metabolic activity, and may have reduced false-negative findings by allowing time for population of micrometastatic disease to within the limits of PET spatial resolution.
Conclusion
We present 5-year outcomes in a prospectively collected cohort of patients with locally advanced cervical cancer undergoing a homogeneous work-up and treatment in a single institution. Posttherapy CMR on FDG PET/CT scanning was a powerful factor predicting patient survival both after initial definitive and after salvage radiation therapy. In our cohort HPV infection subtype was not an independent factor for predicting survival in multivariable analysis. Further investigation of the association between HPV infection status and outcome in larger cohorts of women from western populations is warranted.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi:10.1002/ijc.25516.
World Health Organization. Global burden of disease: 2004 update. Geneva: World Health Organization; 2008. p. 30.
Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997;350:535–40.
Grigsby PW, Siegel BA, Dehdashti F, Rader J, Zoberi I. Posttherapy [18F] fluorodeoxyglucose positron emission tomography in carcinoma of the cervix: response and outcome. J Clin Oncol. 2004;22:2167–71.
Grigsby PW, Siegel BA, Dehdashti F, Mutch DG. Posttherapy surveillance monitoring of cervical cancer by FDG-PET. Int J Radiat Oncol Biol Phys. 2003;55:907–13.
Siva S, Herschtal A, Thomas JM, Bernshaw DM, Gill S, Hicks RJ, et al. Impact of post-therapy positron emission tomography on prognostic stratification and surveillance after chemoradiotherapy for cervical cancer. Cancer. 2011;117:3981–8. doi:10.1002/cncr.25991.
Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW. Metabolic response on post-therapy FDG-PET predicts patterns of failure after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2012;83:185–90. doi:10.1016/j.ijrobp.2011.05.053.
Lee Y, Auh SL, Wang Y, Burnette B, Meng Y, Beckett M, et al. Therapeutic effects of ablative radiation on local tumor require CD8+ T cells: changing strategies for cancer treatment. Blood. 2009;114:589–95. doi:10.1182/blood-2009-02-206870.
Mac Manus MP, Hicks RJ, Matthews JP, McKenzie A, Rischin D, Salminen EK, et al. Positron emission tomography is superior to computed tomography scanning for response-assessment after radical radiotherapy or chemoradiotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2003;21:1285–92.
Hicks RJ, Mac Manus MP, Matthews JP, Hogg A, Binns D, Rischin D, et al. Early FDG-PET imaging after radical radiotherapy for non–small-cell lung cancer: inflammatory changes in normal tissues correlate with tumor response and do not confound therapeutic response evaluation. Int J Radiat Oncol Biol Phys. 2004;60:412–8.
Kalff V, Ware R, Heriot A, Chao M, Drummond E, Hicks RJ. Radiation changes do not interfere with postchemoradiation restaging of patients with rectal cancer by FDG PET/CT before curative surgical therapy. Int J Radiat Oncol Biol Phys. 2009;74:60–6.
Rischin D, Young RJ, Fisher R, Fox SB, Le Q-T, Peters LJ, et al. Prognostic significance of p16INK4A and human papillomavirus in patients with oropharyngeal cancer treated on TROG 02.02 phase III trial. J Clin Oncol. 2010;28:4142–8.
Wang CC, Lai CH, Huang YT, Chao A, Chou HH, Hong JH. HPV genotypes predict survival benefits from concurrent chemotherapy and radiation therapy in advanced squamous cell carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2012;84:e499–506. doi:10.1016/j.ijrobp.2012.06.031.
Lindel K, Burri P, Studer H, Altermatt H, Greiner R, Gruber G. Human papillomavirus status in advanced cervical cancer: predictive and prognostic significance for curative radiation treatment. Int J Gynecol Cancer. 2005;15:278–84.
Barnard GA. A new test for 2 × 2 tables. Nature. 1945;156:177.
Barnard GA. Significance tests for 2 × 2 tables. Biometrika. 1947;34:123–38.
Havrilesky LJ, Kulasingam SL, Matchar DB, Myers ER. FDG-PET for management of cervical and ovarian cancer. Gynecol Oncol. 2005;97:183–91.
Colombo N, Carinelli S, Colombo A, Marini C, Rollo D, Sessa C. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii27–32.
Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW. Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. JAMA. 2007;298:2289–95. doi:10.1001/jama.298.19.2289.
Beriwal S, Kannan N, Sukumvanich P, Richard SD, Kelley JL, Edwards RP, et al. Complete metabolic response after definitive radiation therapy for cervical cancer: patterns and factors predicting for recurrence. Gynecol Oncol. 2012;127:303–6. doi:10.1016/j.ygyno.2012.08.006.
De Villiers E-M, Fauquet C, Broker TR, Bernard H-U, zur Hausen H. Classification of papillomaviruses. Virology. 2004;324:17–27.
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907.
Rautava J, Kuuskoski J, Syrjänen K, Grenman R, Syrjänen S. HPV genotypes and their prognostic significance in head and neck squamous cell carcinomas. J Clin Virol. 2012;53:116–20.
Nichols AC, Dhaliwal SS, Palma DA, Basmaji J, Chapeskie C, Dowthwaite S, et al. Does HPV type affect outcome in oropharyngeal cancer? J Otolaryngol Head Neck Surg. 2013;42:9.
Mirghani H, Amen F, Blanchard P, Moreau F, Guigay J, Hartl D, et al. Treatment de‐escalation in HPV-positive oropharyngeal carcinoma: ongoing trials, critical issues and perspectives. Int J Cancer. 2015;136:1494–503.
Bachtiary B, Obermair A, Dreier B, Birner P, Breitenecker G, Knocke TH, et al. Impact of multiple HPV infection on response to treatment and survival in patients receiving radical radiotherapy for cervical cancer. Int J Cancer. 2002;102:237–43.
Harima Y, Sawada S, Nagata K, Sougawa M, Ohnishi T. Human papilloma virus (HPV) DNA associated with prognosis of cervical cancer after radiotherapy. Int J Radiat Oncol Biol Phys. 2002;52:1345–51.
Huang LW, Chao SL, Hwang JL. Human papillomavirus 31 related types predict better survival in cervical carcinoma. Cancer. 2004;100:327–34.
Werness BA, Levine AJ, Howley PM. Association of human papillomavirus types 16 and 18 E6 proteins with p53. Science. 1990;248:76–9.
Lina Villa L, Schlegel R. Differences in transformation activity between HPV-18 and HPV-16 map to the viral LCR-E6-E7 region. Virology. 1991;181:374–7.
Arends M, Wyllie A, Bird C. Human papillomavirus type 18 is associated with less apoptosis in fibroblast tumours than human papillomavirus type 16. Br J Cancer. 1995;72:646–9.
Wang CC, Lai CH, Huang HJ, Chao A, Chang CJ, Chang TC, et al. Clinical effect of human papillomavirus genotypes in patients with cervical cancer undergoing primary radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78:1111–20. doi:10.1016/j.ijrobp.2009.09.021.
Acknowledgment
The authors acknowledge Prof. Stephen B. Fox for his support in this work.
Compliance with ethical standards
ᅟ
Funding
This research was supported by a grant from the Peter MacCallum Cancer Centre Foundation.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siva, S., Deb, S., Young, R.J. et al. 18F-FDG PET/CT following chemoradiation of uterine cervix cancer provides powerful prognostic stratification independent of HPV status: a prospective cohort of 105 women with mature survival data. Eur J Nucl Med Mol Imaging 42, 1825–1832 (2015). https://doi.org/10.1007/s00259-015-3112-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3112-8