Abstract
Purpose
To determine whether 18F-FDG uptake in breast cancer correlates with immunohistochemically defined subtype and is able to predict molecular subtypes.
Methods
This retrospective study involved 306 patients with 308 mass-type invasive breast cancers (mean size 2.65 cm, range 1.0–15.0 cm) who underwent 18F-FDG PET/CT before therapy. The correlations between primary tumour 18F-FDG uptake on PET/CT, expressed as SUVmax, and clinicopathological findings and molecular subtype, i.e. luminal A, luminal B (HER2-negative), luminal B (HER2-positive), HER2-positive and triple-negative, were analysed. The predictors of these subtypes were investigated.
Results
The mean SUVmax of the 308 tumours was 5.33 ± 3.63 (range 1.15–19.01). Among the subtypes of the 308 tumours, 87 (28.2 %) were luminal A, 111 (36.0 %) were luminal B (HER2-negative), 31 (10.1 %) were luminal B (HER2-positive), 26 (8.4 %) were HER2-positive and 53 (17.2 %) were triple-negative, and the corresponding mean SUVmax were 3.41 ± 2.07 (range 1.18–14.30), 5.17 ± 3.52 (range 1.35–19.01), 6.57 ± 3.84 (range 1.42–15.58), 7.55 ± 3.63 (range 2.30–13.60) and 6.97 ± 4.17 (range 1.15–16.06), respectively. A cut-off value of 3.60 yielded 70.1 % sensitivity and 66.1 % specificity with an area under the receiver operating characteristics curve (AUC) of 0.734 for predicting that a tumour was of the luminal A subtype. A cut-off value of 6.75 yielded 65.4 % sensitivity and 75.2 % specificity with an AUC of 0.704 for predicting a HER2-positive subtype.
Conclusion
SUVmax, a metabolic semiquantitative parameter, shows a significant correlation with the molecular subtype of breast cancer, and is useful for predicting the luminal A or HER2-positive subtype.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a heterogeneous disease. As a result of gene expression analysis, breast cancer is now classified into several different subtypes [1], and this information is useful for predicting response to treatment [2–4]. There is a correlation between prognosis and breast cancer subtype: luminal A, luminal B, human epidermal growth factor receptor 2-positive (HER2-positive), and triple-negative [5]. However, as gene expression profiling by microarray is not always feasible, immunohistochemical classification of the “intrinsic” subtypes of breast cancer according to the expression status of the oestrogen receptor (ER), progesterone receptor (PR), HER2 and Ki-67 has been suggested [6, 7]. In 2011, the St. Gallen expert panel identified breast cancer subtypes: luminal A (ER-positive and/or PR-positive, HER2-negative and Ki-67 <14 %), luminal B (ER-positive and/or PR-positive, HER2-negative and Ki-67 ≥14 %; or ER-positive and/or PR-positive, HER2-positive, irrespective of Ki-67 expression), HER2-positive (ER-negative, PR-negative and HER2-positive), and triple-negative (ER-negative, PR-negative and HER2-negative) [8], and systemic treatment recommendations were presented for these subtypes in the St. Gallen consensus recommendations. Several studies have since validated the clinical utility of these classifications [9, 10].
Many previous studies have demonstrated relationships between 18F-FDG uptake on PET/CT and clinicopathological characteristics, which are known to be important prognostic indicators of long-term survival in breast cancer patients [11–17]. Moreover, in recent years, several authors have demonstrated a good correlation between 18F-FDG uptake and the newly defined molecular subtypes [16–19]. However, the diagnostic performance of 18F-FDG uptake for prediction of these molecular subtypes based on the newly determined criteria has not been fully investigated. Only one group has evaluated this for prediction of the luminal A subtype, but the sample size was relatively small and no HER2-positive patients were included [19].
Therefore, the purpose of the present study was to determine (1) whether a correlation exists between 18F-FDG uptake on PET/CT, expressed as the maximum standardized uptake value (SUVmax), and the subtype of breast cancer defined by the St. Gallen International Expert Consensus, and (2) whether primary tumour SUVmax can predict the molecular subtype.
Materials and methods
Patient selection
The institutional review board of our hospital approved this retrospective study; the requirement for informed consent was waived. Between October 2008 and December 2014, 433 female patients with newly diagnosed invasive breast cancer underwent whole-body 18F-FDG PET/CT for initial staging. Of these patients, 60 with no focal uptake on PET, 34 with an apparent tumour size of less than 1 cm because of partial volume effects, and 33 in whom data pertaining to the immunohistochemical profiles of their tumour were lacking, were excluded. Finally, 308 index breast cancers in 306 patients were included in our study. Two patients had bilateral breast cancer. In patients with multifocal or multicentric cancer, the largest tumour was selected. The mean interval between PET/CT and surgery in 141 patients who underwent PET/CT and subsequent mastectomy or breast-conserving surgery without neoadjuvant chemotherapy or endocrine therapy was 26.3 days (range 5–49 days).
18F-FDG PET/CT
All 18F-FDG PET/CT examinations were performed using a PET/CT scanner incorporating a 16 multislice detector (Gemini GXL16; Philips Medical Systems, Eindhoven, The Netherlands) using gadolinium oxyorthosilicate detectors. Patients were instructed to fast for 5 h before the scan, and blood glucose was measured immediately before injection of 4.0 MBq/kg body weight of 18F-FDG. No patients showed a blood glucose level of more than 160 mg/dL. Static emission images were obtained approximately 60 min after injection. For attenuation correction and anatomic localization, helical CT scans from the top of the head to the bottom of the feet were obtained using the following parameters: tube voltage 120 kV, effective tube current auto-mA (up to 120 mA s), gantry rotation speed 0.5 s, detector configuration 16 × 1.5 mm, slice thickness 2 mm, and transverse field of view 600 mm. Immediately after completion of the CT scan, PET images of the region from the head to the mid-thigh were acquired for 90 s per bed position, and the region from the mid-thigh to the toes for 30 s per bed position employing the variable sampling method. Images at 13–14 bed positions each of 90 s and 6 bed positions each of 30 s were then acquired in three-dimensional mode, thus requiring between 22 and 24 min of emission scanning per patient. The patients were allowed to breathe normally during PET acquisitions.
Imaging analysis
All 18F-FDG PET/CT images were retrospectively reviewed in consensus by two experienced nuclear medicine physicians with 10 years of experience in PET/CT without any knowledge of other imaging results or clinicopathological findings other than the presence of breast cancer. For quantitative analysis of 18F-FDG uptake, a region of interest (ROI) was placed over the most intense area of 18F-FDG accumulation by the primary breast tumour in each patient. The SUV was calculated as: SUV = radioactivity concentration of the region (Bq/mL)/[injected dose (Bq)/patient weight (g)]. The SUVmax, defined as the peak SUV in the pixel with the highest count within the ROI, was measured and recorded for the focal areas of uptake.
Histological evaluation
Histopathological analysis was performed on specimens obtained by gross needle aspiration biopsy and surgical procedures. The histological type of the tumour, tumour size, and nuclear grade (1 well differentiated, 2 moderately differentiated, 3 poorly differentiated) were determined from formalin-fixed paraffin-embedded tumour tissue sections cut at a thickness of 5 μm and stained with haematoxylin and eosin. Immunohistochemistry was performed on paraffin-embedded material using primary antibodies against ER, PR and HER2, and the proliferation index was determined using Ki-67 antibody [20]. Expression levels of ER (1D5; Dako, Glostrup, Denmark), PR (PgR636; Dako), HER2 (Hercep Test; Dako), and Ki67 (MIB1; Dako) were determined immunohistochemically in terms of the percentages of cancer cells positive for ER, PR and Ki67 in the nuclei, and membrane staining for HER2 used automated immunostaining systems (BOND-MAX for ER and PR; Leica Microsystems, Tokyo, Japan; Autostainer for HER2 and Ki67; Dako).
ER and PR expression was scored as positive or negative with a nuclear immunostaining cut-off of 10 %. HER2 expression was evaluated as positive when membrane immunostaining was complete in more than 30 % of the tumour cells (3+) or, when less than 30 % (2+), fluorescence in situ hybridization analysis demonstrated HER2 gene amplification. The Ki-67 proliferation index was determined as the percentage of nuclei that were immunostained. The final axillary lymph node status (positive or negative) was established by the clinician performing the pathological confirmation, employing axillary lymph node dissection, sentinel lymph node biopsy or fine-needle aspiration cytology, or by imaging techniques.
Molecular classification of groups
According to the different combinations of ER, PR and HER2 status, and in line with the recommendations of the 12th International Breast Conference [8], the patients were categorized into five subgroups:
-
1.
Luminal A: ER-positive and/or PR-positive, HER2-negative, Ki-67 low (<14 %)
-
2.
Luminal B (HER2-negative): ER-positive and/or PR-positive, HER2-negative and Ki-67 high (≥14 %)
-
3.
Luminal B (HER2-positive): ER-positive and/or PR-positive, HER2-positive and any Ki-67 index
-
4.
HER2-positive: ER-negative, PR-negative and HER2-positive
-
5.
Triple-negative: ER-negative, PR-negative and HER2-negative
Statistical analysis
The correlations between the SUVmax of the breast cancer and the clinicopathological and immunohistochemical data were evaluated using the Wilcoxon rank sum test (two variables), the Kruskal-Wallis test (three or more nominal variables) and linear-by-linear association test (three or more ordered variables). Variables for which p was <0.05 in univariate analysis were subjected to multiple linear regression analysis to determine those that were independently associated with SUVmax. We examined whether there was a significant difference in mean SUV among the five groups, Luminal A, Luminal B (HER2-negative), Luminal B (HER2-positive), HER2-positive and triple-negative, using single-factor analysis of variance and a multiple comparison test for parametric data with Bonferroni correction. Receiver operating characteristic (ROC) curve analysis was performed to examine which subgroups could be differentiated from the others on the basis of SUVmax. The diagnostic accuracy of the optimal cut-off value for differentiating one subgroup from the others was also determined by ROC analysis. The data were analysed using the SAS version 9.3 statistical software package (SAS Institute, Cary, NC). Statistical significance was defined as p < 0.05.
Results
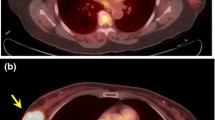
The mean ± standard deviation age of the 306 patients was 58.9 ± 13.5 years (range 30–95 years). The mean ± standard deviation size of the invasive tumours was 2.65 ± 1.83 cm (range 1.0–15.0 cm). The histological classifications of the cancers were: invasive ductal carcinoma (282 patients, 91.6 %), invasive lobular carcinoma (13 patients, 4.2 %), and other specified cancers (13 patients, 4.2 %; ten mucinous carcinomas, two apocrine carcinomas and one medullary carcinoma). The subtypes of the 308 tumours were luminal A in 87 patients (28.2 %), luminal B (HER2-negative) in 111 patients (36.0 %), luminal B (HER2-positive) in 31 patients (10.1 %), HER2-positive in 26 patients (8.4 %), and triple-negative in 53 patients (17.2 %). The clinicopathological findings and results of univariate regression analysis for the 308 breast cancers are summarized in Table 1. PET/CT imaging in representative patients is shown in Figs. 1 and 2.
A higher nuclear grade, a larger tumour size, a positive axillary lymph node status and higher TNM stage were all significantly associated with a higher SUVmax (Table 1). In terms of immunohistochemical profile, univariate analysis showed that ER negativity, PR negativity, HER2 positivity and high Ki-67 expression were also significantly associated with a higher SUVmax (Table 1).
Multiple regression analysis was performed to select independent clinicopathological variables associated with SUVmax in all patients with primary breast cancer. The variables entered into the multivariate models included tumour size (categorized as ≤2 cm versus >2 cm), nuclear grade (categorized as grade 1 versus grade 2 or 3), ER, PR, HER2 and Ki-67 expression, axillary nodal status, and TNM stage (categorized as stage I or II versus stage III or IV). Tumour size, ER status, nuclear grade, and TNM stage were all shown to independently influence SUVmax (Table 2).
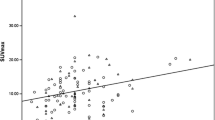
The mean SUVmax were 3.41 ± 2.07 (range 1.18–14.30), 5.17 ± 3.52 (range 1.35–19.01), 6.57 ± 3.84 (range 1.42–15.58), 7.55 ± 3.63 (range 2.30–13.60) and 6.97 ± 4.17 (range 1.15 – 16.06) for the luminal A, luminal B (HER2-negative), luminal B (HER2-positive), HER2-positive and triple-negative subgroups, respectively (Table 3 and Fig 3). SUVmax differed significantly among the five subgroups (p < 0.0001). Moreover, Bonferroni correction revealed significant differences in SUVmax between the luminal A and luminal B (HER2-negative) subgroups (p < 0.0001), the luminal A and luminal B (HER2-positive) subgroups (p < 0.0001), the luminal A and HER2-positive subgroups (p < 0.0001), the luminal A and triple-negative subgroups (p < 0.0001), the luminal B (HER2-negative) and HER2-positive subgroups (p = 0.00021), and the luminal B (HER2-negative) and triple negative subgroups (p = 0.00038).
The mean SUVmax was 3.41 ± 2.07 (range 1.18 – 14.30) for luminal A tumours and 6.08 ± 3.83 (range 1.15 – 19.01) for non-luminal A tumours (p < 0.0001). In the ROC analysis the optimal area under the ROC curve (AUC) was 0.734. A cut-off SUVmax of 3.60 yielded a sensitivity of 70.1 % (95 % confidence interval, CI, 60.5 – 79.7 %), a specificity of 66.1 % (95 % CI 59.8 – 72.3 %), and an accuracy of 67.2 % (95 % CI 62.0 – 72.5 %) for differentiation of luminal A from non-luminal A subtypes. The mean SUVmax was 7.55 ± 3.63 (range 2.30 – 13.60) for HER2-positive tumours and 5.12 ± 3.57 (range 1.15 – 19.01) for non-HER2-positive tumours (p < 0.0001). A cut-off SUVmax of 6.75 yielded a sensitivity of 65.4 % (95 % CI 47.1 – 83.7 %), a specificity of 75.2 % (95 % CI 70.1 – 80.2 %), an accuracy of 74.4 % (95 % CI 69.5 – 79.2 %), and an AUC of 0.704 for differentiation of HER2-positive from non-HER2-positive subtypes. The mean SUVmax was 6.97 ± 4.17 (range 1.15 – 16.06) for triple-negative tumours and 4.98 ± 3.42 (range 1.18 – 19.01) for non-triple-negative tumours (p < 0.0001). A cut-off SUVmax of 5.45 yielded a sensitivity of 64.1 % (95 % CI 51.2 – 72.8 %), a specificity of 67.1 % (95 % CI 61.3 – 72.8 %), an accuracy of 66.6 % (95 % CI 61.3 – 71.8 %), and an AUC of 0.649 for prediction of triple-negative tumours.
Discussion
The major findings of the present study were: (1) 18F-FDG uptake by breast cancer, expressed as SUVmax, was significantly correlated with many clinicopathological features, and (2) SUVmax of the primary tumour was significantly correlated with the molecular subtype of breast cancer, and was of value in predicting the luminal A or HER2-positive subtype.
Many previous studies have demonstrated relationships between 18F-FDG uptake on PET/CT and clinicopathological characteristics (including tumour size, histological grade, ER status, PR status, HER2 status, Ki-67 index, axillary lymph node status, and stage) that are known to be important predictors of long-term survival in breast cancer patients [11–17]. In our present series, the primary tumour SUVmax was significantly correlated with all immunohistochemical parameters (ER, PR, HER2 and Ki-67). All previous studies have shown that SUVmax is positively correlated with the Ki-67 index and negatively correlated with ER status [11–17]. Many studies have shown that SUVmax is negatively correlated with PR status, except one: in a study of 36 patients, Osborne et al. [12] found no significant association between SUV and PR status. The existence of a relationship between 18F-FDG uptake and HER status is a matter of controversy. Some groups have found a significant relationship between 18F-FDG uptake and HER2 oncogene expression [11, 15, 17], whereas others have not found a significant correlation [12–14, 16], suggesting that HER2 has no major influence on oncogene pathways.
The St. Gallen expert panel has identified five breast cancer subtypes [8]. Luminal A is the most common subtype, showing low expression of genes related to cellular proliferation. Patients with this subtype have a higher survival rate and lower relapse rate than those with other subtypes because of the good response to hormone treatment. The luminal B subtype has a more aggressive phenotype, a higher histological grade, a higher proliferative index and worse prognosis than the luminal A subtype. HER2-positive breast cancers are characterized by high expression of the HER2 gene, which promotes tumour growth and progression. They tend to be more aggressive than other subtypes: 75 % have a high histological grade, more than 40 % have p53 mutations, and they are less responsive to hormone treatment. The HER2-positive subtype is clinically associated with a higher rate of recurrence and mortality due to tumour aggressiveness, although the advent of antibody treatment with trastuzumab targeting this receptor has improved survival outcomes in the last decade [21]. Triple-negative breast cancer, especially the intrinsic basal type, accounting for 80 % of such tumours, has a more aggressive biology than other subtypes; it is associated with a poorer outcome than luminal subtypes, and no form of targeted therapy has yet been developed [22].
To our knowledge, only four groups have evaluated the relationship between primary tumour 18F-FDG uptake and molecular subtype of breast cancer [16–19]. Similar to our series, all four groups found a significant correlation between SUVmax and molecular subtype, the former being higher in more biologically aggressive tumours. Four groups have demonstrated that triple-negative cancers have the highest SUVmax among five or four subgroups, whereas HER2-positive cancers had the highest SUVmax among five subgroups in our series. We considered that differences among the subjects included in these studies may account for the differences in the results. Similar to our present study, Miyake et al. [19] demonstrated that SUVmax is of value for differentiating between luminal A and non-luminal A subtypes of invasive breast cancer (AUC 0.751). Our present results suggest that SUVmax has the potential for use in the diagnosis of breast cancer subtype and may be useful as a diagnostic adjunct to histopathological diagnosis. However, further analysis in a larger patient population and a multicentre study is necessary to confirm this speculation.
Our study had several limitations. First, it had a retrospective design and was conducted at a single institution, which would have unavoidably introduced selection bias. Second, the immunohistochemical results in 165 of the 306 patients (54 %) who had undergone neoadjuvant chemotherapy or endocrine therapy after 18F-FDG PET/CT examinations were obtained by sonographically assisted core needle biopsy. Therefore, the entire tumour might not have been evaluated in these patients, resulting in degradation of the reliability of the histopathological results. Third, we did not analyse actual survival data.
In conclusion, SUVmax, a semiquantitative metabolic parameter obtained by 18F-FDG PET/CT, was found to be significantly correlated with the molecular subtype of breast cancer, higher values being evident in more biologically aggressive tumours. This index may contribute to the prediction of the luminal A or HER2-positive subtype of invasive breast cancer, and thus the selection of an appropriate therapeutic strategy.
References
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
van ’t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–6.
van’t Veer LJ, Paik S, Hayes DF. Gene expression profiling of breast cancer: a new tumor marker. J Clin Oncol. 2005;23:1631–5.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001;98:10869–74.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
Hugh J, Hanson J, Cheang MC, Nielsen TO, Perou CM, Dumontet C, et al. Breast cancer subtypes and response to docetaxel in node-positive breast cancer: use of an immunohistochemical definition in the BCIRG 001 trial. J Clin Oncol. 2009;27:1168–76.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ. Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen international expert consensus on the primary therapy of early breast cancer 2011. Ann Oncol. 2011;22:1736–47.
Dubsky P, Filipits M, Jakesz R, Rudas M, Singer CF, Greil R, et al. EndoPredict improves the prognostic classification derived from common clinical guidelines in ER-positive, HER2-negative early breast cancer. Ann Oncol. 2013;24:640–7.
Niemiec J, Adamczyk A, Malecki K, Ambicka A, Rys J. Tumor grade and matrix metalloproteinase 2 expression in stromal fibroblasts help to stratify the high-risk group of patients with early breast cancer identified on the basis of St Gallen recommendations. Clin Breast Cancer. 2013;13:119–28.
Ueda S, Tsuda H, Asakawa H, Shigekawa T, Fukatsu K, Kondo N, et al. Clinicopathological and prognostic relevance of uptake level using 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in primary breast cancer. Jpn J Clin Oncol. 2008;38:250–8.
Osborne JR, Port E, Gonen M, Doane A, Yeung H, Gerald W, et al. 18F-FDG PET of locally invasive breast cancer and association of estrogen receptor status with standardized uptake value: microarray and immunohistochemical analysis. J Nucl Med. 2010;51:543–50.
Heudel P, Cimarelli S, Montella A, Bouteille C, Mognetti T. Value of PET-FDG in primary breast cancer based on histopathological and immunohistochemical prognostic factors. Int J Clin Oncol. 2010;15:588–93.
Groheux D, Giacchetti S, Moretti JL, Porcher R, Espié M, Lehmann-Che J, et al. Correlation of high 18F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging. 2011;38:426–35.
Wang CL, MacDonald LR, Rogers JV, Aravkin A, Haseley DR, Beatty JD. Positron emission mammography: correlation of estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 status and 18F-FDG. AJR Am J Roentgenol. 2011;197:W247–55.
Koolen BB, Vrancken Peeters MJ, Wesseling J, Lips EH, Vogel WV, Aukema TS, et al. Association of primary tumour FDG uptake with clinical, histopathological and molecular characteristics in breast cancer patients scheduled for neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2012;39:1830–8.
Koo HR, Park JS, Kang KW, Cho N, Chang JM, Bae MS, et al. 18F-FDG uptake in breast cancer correlates with immunohistochemically defined subtypes. Eur Radiol. 2014;24:610–8.
García Vicente AM, Soriano Castrejón Á, León Martín A, Chacón López-Muñiz I, Muñoz Madero V, Muñoz Sánchez Mdel M, et al. Molecular subtypes of breast cancer: metabolic correlation with 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2013;40:1304–11.
Miyake KK, Nakamoto Y, Kanao S, Tanaka S, Sugie T, Mikami Y, et al. Diagnostic value of 18F-FDG PET/CT and MRI in predicting the clinicopathologic subtypes of invasive breast cancer. AJR Am J Roentgenol. 2014;203:272–9.
Murase K, Yanai A, Saito M, Imamura M, Miyagawa Y, Takatsuka Y, et al. Biological characteristics of luminal subtypes in pre- and postmenopausal estrogen receptor-positive and HER2-negative breast cancers. Breast Cancer. 2014;21:52–7.
Gianni L, Dafni U, Gelber RD, Azambuja E, Muehlbauer S, Goldhirsch A, et al. Treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: a 4-year follow-up of a randomised controlled trial. Lancet Oncol. 2011;12:236–44.
Caudle AS, Yu TK, Tucker SL, Bedrosian I, Bedrosian I, Litton JK, et al. Local-regional control according to surrogate markers of breast cancer subtypes and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast conserving therapy. Breast Cancer Res. 2012;14:R83.
Compliance with ethical standards
Conflicts of interest
None.
Human and animal rights and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This was a retrospective study, for which formal consent is not required. This article does not describe any studies with animals performed by any of the authors. This retrospective study was approved by the institutional review board, and the need for patient informed consent was waived.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kitajima, K., Fukushima, K., Miyoshi, Y. et al. Association between 18F-FDG uptake and molecular subtype of breast cancer. Eur J Nucl Med Mol Imaging 42, 1371–1377 (2015). https://doi.org/10.1007/s00259-015-3070-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3070-1