Abstract
Purpose
Reversible ischaemia at radionuclide myocardial perfusion imaging (MPI) accurately predicts risk of cardiac death and nonfatal myocardial infarction (major adverse cardiac events, MACE). This prognostic penetrance might be empowered by accounting for exercise tolerance as an indirect index of ischaemia severity. The present study aimed to verify this hypothesis integrating imaging assessment of ischaemia severity with exercise maximal rate pressure product (RPP) in a large cohort of patients with suspected or known coronary artery disease (CAD).
Methods and results
We analysed 1,502 consecutive patients (1,014 men aged 59 ± 10 years) submitted to exercise stress/rest MPI. To account for exercise tolerance, the summed difference score (SDS) was divided by RPP at tracer injection providing a clinical prognostic index (CPI). Reversible ischaemia was documented in 357 patients (24 %) and was classified by SDS as mild (SDS 2–4) in 180, moderate (SDS 5–7) in 118 and severe (SDS >7) in 59. CPI values of ischaemic patients were clustered into tertiles with lowest and highest values indicating low and high risk, respectively. CPI modified SDS risk prediction in 119/357 (33 %) patients. During a 60-month follow-up, MACE occurred in 68 patients. Kaplan-Meier analysis revealed that CPI significantly improved predictive power for MACE incidence with respect to SDS alone. Multivariate Cox analysis confirmed the additive independent value of CPI-derived information.
Conclusion
Integration of ischaemic threshold and ischaemia extension and severity can improve accuracy of exercise MPI in predicting long-term outcome in a large cohort of patients with suspected or known CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radionuclide myocardial perfusion imaging (MPI) is routinely applied for risk assessment in patients with known or suspected coronary artery disease (CAD) (1, 2). According to its well-validated pathophysiological background, MPI not only detects ischaemia and scar tissue, but it also permits one to estimate their location and extension, providing prognostic information with an intrinsically additive value with respect to clinical data, coronary anatomy and exercise stress score (3–6). Similarly, the development of standardized methods for image interpretation permitted extending its use in multicentre studies evaluating the prognostic impact of integrated indexes representing extension and severity of total hypoperfused myocardium and reversible ischaemia. This approach confirmed the predictive accuracy of MPI in populations with different disease prevalence submitted to either physical or pharmacological stress (1–6).
Due to the kinetic features of the tracers used, MPI is the best-suited technique to noninvasively characterize coronary blood flow (CBF) response to physical effort and thus to the most common trigger of myocardial ischaemia in daily life. Nevertheless, despite a plethora of analyses comparing predictive accuracy of stress ECG and MPI, no study has tried so far to verify whether combining imaging-derived indexes with clinical markers of ischaemic threshold and exercise tolerance can eventually improve risk stratification.
This hypothesis seems theoretically sound since the direct evaluation of presence, severity and extension of exercise-induced ischaemia intrinsically overcomes the relatively low accuracy of ST segment depression and symptoms. On the other hand, accounting for exercise tolerance complements the scintigraphic indexes as the lower the exercise intensity not met by an adequate CBF response, the higher the incidence of ischaemia and its mechanical or arrhythmic complications.
To verify this hypothesis, this study combined imaging indexes of ischaemia severity with maximal achieved workload (WL) and maximal rate pressure product (RPP) as widely used indicators of exercise tolerance and myocardial oxygen consumption, respectively (7, 8). The data obtained indicate that this integration does indeed improve the prognostic penetrance of MPI in a large cohort of patients with known or suspected CAD.
Materials and methods
Our database included 2,270 patients with available rest and exercise gated single photon emission computed tomography (SPECT) data, referred for MPI between June 2001 and March 2007 at the Nuclear Cardiology Laboratory of the University of Naples Federico II, Italy. Overall, 742 patients were excluded because of: (1) recent (3 months) acute coronary syndrome, (2) previous episode of congestive heart failure, (3) valvular heart disease, (4) myocardial hypertrophy, (5) atrial fibrillation, (6) concomitant severe non-cardiac illness, or (7) missing follow-up or acceptance of our surveillance program. Of the remaining 1,528 patients, 26 were submitted to revascularization within 60 days after MPI and were excluded assuming a direct role of the test in treatment strategy (9). Accordingly, the total study population included 1,502 patients (1,014 men aged 59 ± 9 years). The Ethics Committee for the Biomedical Activities of the University Federico II approved the study and all patients gave informed consent.
Stress myocardial perfusion imaging
All patients underwent same-day 99mTc-sestamibi or tetrofosmin exercise and rest gated MPI according to the European Association of Nuclear Medicine/European Society of Cardiology (EANM/ESC) procedural guidelines (10). QPS software (Cedars-Sinai Cardiac Suite, Los Angeles, CA, USA) was used to classify segmental radioactivity according to the standardized 5-point scale (from 0 normal to 4 absent) (11). Segmental values in rest and stress scans were summed to generate summed stress (SSS), rest (SRS) and difference (SDS) scores, using the conventional 17-segment model (11). Left ventricular volumes and ejection fraction (LVEF) were computed using QGS software.
Definition of risk predictors
Cardiovascular risk was stratified according to the Framingham 10-year global CAD risk score (12). Clinical and ECG response to exercise was categorized into three risk classes according to the Duke treadmill score and thus considering exercise duration, ST segment depression as well as presence and severity of angina (13). WL was expressed in metabolic equivalents (METs). Similarly, LVEF was categorized as normal (>50 %), moderately impaired (30–50 %) or severely compromised (<30 %) according to previously published criteria (14). According to the literature (3–5, 14, 15), SSS values were scored as normal (0–3), mild (4–8), moderate (9–13) or severe (>13) defects. In the presence of SSS >3, ischaemia was categorized according to SDS as absent (<2), mild (2–4), moderate (5–7) or severe (>7). Conversely, to integrate SDS with a clinical estimation of ischaemic threshold, we developed a “clinical” prognostic index (CPI) normalizing SDS for RPP and a “physical” prognostic index (PPI) normalizing SDS for maximal WL at the time of tracer injection, according to the formulas:
where the multiplication terms represent simple scaling factors. Obviously, due to their nature, these indexes were only computed for patients with evident ischaemia at MPI.
Outcome determination
Follow-up data were obtained using a questionnaire that was administered by a phone call and by review of hospital records by individuals blinded to the patient’s test results. Subjects were prospectively monitored for the following events: death, cardiac death, nonfatal myocardial infarction (MI) or coronary revascularization. The date of the event or of the last contact with the patient was used to determine the length of follow-up. MI events were defined by clinical determination of the treating cardiologist. Cardiac death was defined as sudden death or death due to heart failure. Fatal MI was considered cardiac death if death occurred within the same hospitalization. The primary endpoint was the occurrence of major adverse cardiac events (MACE) (cardiac death or nonfatal MI), and the secondary endpoint was the composite occurrence of MACE or late (>60 days) revascularization.
Statistical analysis
Follow-up data on the first 5 years after accrual were used. In the primary analysis, only MACE was considered, whereas in the secondary analyses, MACE or revascularization, whichever was first, were considered as events.
First, for descriptive purposes, time to event distributions were estimated for all 1,502 patients using the Kaplan-Meier method and compared with the log-rank test. Then, analyses were focused on patients with reversible ischaemia in whom the divergent classification systems can provide different results. In these patients, a set of univariate and multivariate Cox models were fitted to the data: in univariate analyses, the incidence of MACE was modelled as a function of each of the following variables: age, Duke treadmill score, Framingham score, SDS, PPI and CPI. Then, all variables were tentatively included in a multivariate Cox model by means of a step-up (forward) procedure, based on the likelihood ratio test: a p value <0.1 was required for the inclusion of a variable in the model. The proportionality assumptions were assessed graphically according to the Grambsch and Therneau method (16).
Continuous variables are described as mean ± standard deviation and categorical data as percentages. Groups were compared using the t test, Fisher’s exact test or χ2 test, as appropriate. A p value < 0.05 was considered statistically significant. The statistical software used was SPSS Inc., Advanced Models 15.0 (Chicago, IL, USA).
Results
Patient and myocardial perfusion imaging characteristics
Patient demographics, cardiovascular history, medications and clinical response to exercise are shown in Table 1. Of the 1,502 patients, 1,017 (67 %) displayed “negative” exercise stress/rest MPI, 128 (9 %) showed “fixed” perfusion defects, while reversible ischaemia occurred in 357 patients (24 %). The time interval from tracer injection to acquisition was largely variable. Accordingly, post-stress function was not considered. Yet, baseline LVEF was significantly different in the three groups which was highest in patients with negative MPI (60 ± 11 %, p < 0.001 vs both fixed and ischaemic, respectively), intermediate in those with reversible ischaemia (50 ± 13 %, p < 0.001 vs fixed) and lowest in patients with fixed perfusion defects without ischaemia (45 ± 12 %).
Overall prognostic power of conventional MPI indexes in the whole study cohort
During follow-up, 28 patients died from non-cardiac causes. Cardiac death and nonfatal MI occurred in 32 and 36 patients, respectively, accounting for a total of 68 MACEs. Finally, late revascularization was performed in 119 patients accounting for a total of 187 secondary endpoints.
MACE incidence was significantly associated with baseline LV dysfunction (Fig. 1a) that, however, did not significantly predict composite events (Fig. 1b). On the contrary, severity of stress perfusion abnormality, scored by SSS, retained a powerful prognostic penetrance for both primary and secondary endpoints (Fig. 1c, d, respectively). Finally, the predictive value of MPI-detected ischaemia was also confirmed with the incidence of both MACE (Fig. 1e) and composite endpoints (Fig. 1f) being lowest in patients with negative exercise MPI, intermediate in patients with fixed, nonischaemic, perfusion defects and highest in ischaemic ones.
Accounting for ischaemic threshold modifies SDS-based risk stratification
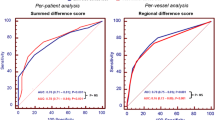
Among the 357 patients with reversible perfusion defects, SDS classified ischaemia severity as mild, moderate or severe in 180, 118 and 59 patients, respectively. Both CPI and PPI showed largely asymmetrical distributions with an average value of 24.9 ± 15.9 and 64.3 ± 47.9, respectively (Fig. 2a, b). Accordingly, the 357 patients were subdivided into tertiles with risk class increasing from lowest to highest tertile for each index tested. As shown in Fig. 2c, CPI was significantly correlated (Pearson coefficient R = 0.80; p < 0.001) with PPI. Nevertheless, the loose nature of this correlation resulted in substantial differences in risk classification (Fig. 2d). Similarly, CPI and PPI altered Duke risk class in 190 (53 %) and 244 (68 %) patients, respectively. Finally, and more importantly, accounting for ischaemic threshold also modified SDS-based risk prediction, as CPI and PPI increased risk class in 117 (33 %) and in 123 (34 %) patients (Fig. 2e, f), respectively.
CPI and PPI risk stratification and agreement with SDS. a, b Largely asymmetrical distribution and tertile classification of both CPI and PPI values in the 357 patients with SDS ≥2. c Scatter plot of correlating PPI index (x-axis) with corresponding CPI value (y-axis). Despite a significant correlation a high number of patients were differently classified by the two indexes whose tertile limits are represented by vertical and horizontal lines, respectively. d Overall agreement in patient classification. e, f Similar discordance in patient classification provided by SDS with respect to CPI and PPI, respectively, that was characterized by an increase in risk class in subjects with mild or moderate ischaemia, represented by SDS value for both indexes
Grading of myocardial ischaemia and outcome prediction
As shown in Fig. 3a, SDS predictive value was limited in the 357 ischaemic patients, with a cumulative 5-year MACE incidence of 15, 12 and 21 % in mild, moderate and severe ischaemia, respectively (log-rank p = 0.455). However, when composite endpoints were considered, the prognostic power of SDS became evident with a cumulative incidence of 23, 41 and 45 % in the same classes, respectively (log-rank p < 0.001) (Fig. 3b).
Improved risk stratification of CPI and PPI. a, b Cumulative hazard curves of patients with mild (green), moderate (blue) and severe (red) ischaemia as classified by SDS value. In this population, SDS scarcely predicted MACE, while it significantly identified the risk for composite endpoints. c, d The same hazard functions according to CPI classification in low (green), medium (blue) and high (red) risk. Accounting for maximal RPP improved MPI risk stratification and significantly predicted risk for both MACE and secondary endpoint. e, f Prognostic predictive value of PPI, with the same classification in low (green), medium (blue) and high (red) risk. PPI only predicts significantly the risk of composite endpoints
By contrast, integrating SDS and RPP significantly predicted both risk types. In fact, MACE cumulative incidence was 9, 14 and 22 % in subjects at low, medium or high risk, respectively (log-rank p < 0.01, Fig. 3c). Similarly, CPI also powerfully predicted a divergent occurrence of composite endpoints in the three risk classes (17, 36 and 45 %, respectively, log-rank p < 0.001, Fig. 3d). On the other hand, normalization for maximal WL achieved a relatively minor prognostic penetrance: it did not significantly predict cumulative incidence of MACE (log-rank p = 0.323, Fig. 3e), although it correctly stratified the risk for the composite endpoint (log-rank p = 0.01, Fig. 3f). Accordingly, due to its low predictive value, PPI index was no longer considered.
The independent prognostic value of CPI and SDS was corroborated by multivariate Cox analysis to discriminate the contribution of each index in the 357 ischaemic patients. As shown in Table 2, SDS showed a weak and nonsignificant predictive value for MACE both in univariate and multivariate analysis. On the other hand, it strongly predicted composite endpoints in univariate analysis (Table 3). However, this association disappeared (p = 0.714) in multivariate analysis, after adjustment for CPI, Framingham risk score and Duke treadmill score (Table 3).
By contrast, normalization for ischaemic threshold improved SDS risk stratification. In fact, CPI correctly predicted the incidence of MACE both in univariate and multivariate, analysis although in the latter approach statistical significance was reached for trend description while it did not reach the formal value for heterogeneity (Table 2). By contrast, CPI prognostic value for the composite endpoint was documented by both analyses (Table 3).
Interestingly, a linear relationship was observed between CPI-derived index and observed cumulative incidence of events. In fact, moderate risk class was associated with a more than twofold increase in the incidence of the composite endpoint and with a 50 % increase in the incidence of MACE. High risk class was associated with a more than threefold increase in the risk of all events and with a two- to threefold increase in the incidence of MACE.
Discussion
The present study confirms the hypothesis that normalizing the imaging score of ischaemia severity and extension by clinical indexes of ischaemic threshold significantly and independently improves risk stratification for cardiac death and nonfatal MI as well as the need for late revascularization.
Pathophysiological considerations
As a first observation, normalizing SDS for exercise tolerance—estimated by either maximal RPP or WL—profoundly modified risk class provided by the Duke treadmill score. This finding was somewhat expected as sensitivity of clinical symptoms and ST segment depression is relatively low in the general population (3). This limitation is further enhanced by the selection bias of our registry study that included a large group of patients submitted to stress imaging because of equivocal findings at exercise stress test. More importantly, angina, dyspnoea and ECG changes are relatively independent from ischaemia severity and thus from the main determinant of outcome directly interrogated by SDS (1–6, 14, 15). Accordingly, the relative disagreement between Duke treadmill and either CPI or PPI score reflects, on the one hand, the contribution of positive MPI despite a negative exercise stress test, on the other hand, the larger SDS variability with respect to clinical markers.
Though less evident, accounting for ischaemic threshold also modified risk prediction offered by SDS alone in ischaemic patients. According to current models (8), the progressive increase in oxygen consumption during exercise is parallelled by an adequate CBF response in control myocardium. By contrast, demand–supply match is lost in jeopardized areas once maximal flow capacity is reached. Severity of perfusion defect is thus correlated inversely with CBF in ischaemic areas and directly with perfusion in control regions. Accordingly, low SDS alone cannot differentiate between two largely different conditions: severe stenoses able to induce symptoms or ECG changes triggering tracer injection in the early exercise phases as opposed to moderate obstructions inducing an only mild perfusion defect and postponing tracer administration at high RPP and WL.
This theoretical limitation is well recognized in daily practice and procedural guidelines warrant description of exercise variables in MPI reports to better define severity of the clinical condition (10). Nevertheless, to the best of our knowledge, the present data represent the first attempt to estimate whether and how the prognostic information provided by SDS and its accurate description of ischaemia severity can be complemented by a clinical evaluation of ischaemic threshold as a surrogate index of its incidence during daily life.
Among the many clinical markers, we adopted maximal WL as a physical measure of exercise intensity and maximal RPP as an index of myocardial oxygen consumption (8). Due to their direct relationship with exercise tolerance, both of them were used as denominators to compute PPI and CPI, respectively. Using this approach, CPI appeared more accurate than PPI despite an obvious correlation between the two indexes. This difference most likely reflects the retrospective nature of our study that allowed different exercise protocols and included patients under active pharmacological treatment. Actually, most antianginal drugs exert their action by reducing heart rate and arterial pressure response to exercise rather than increasing maximal flow capacity (17). The consequent flattening in cardiovascular reaction to exercise increases the WL needed to elicit RPP threshold for ischaemia. In other words, drug treatment can improve maximal tolerated WL without significantly affecting maximal tolerated RPP. Under these circumstances, CPI might probably fit better with daily clinical practice in which drugs, and mostly beta-blockers, are often used at the time of MPI scan. On the contrary, PPI (and its adherence to the daily triggers of ischaemia) might be better suited for untreated patients although its performance cannot be elucidated on the basis of the present data.
Methodological considerations
In clinical practice, QPS software is widely used due to its capability to simultaneously score severity and extension of perfusion defects. Obviously, both variables might have been more precisely described using truly quantitative analyses of flow distribution (4). However, this approach would have increased interobserver variability, reducing analysis robustness and adherence of diagnostic interpretation to routine clinical practice. On the contrary, we already documented the high repeatability of MPI evaluation with this approach whose accuracy in cardiovascular risk stratification was largely confirmed in this cohort of unselected patients with suspected or known CAD. In fact, the incidence of both MACE and late revascularization was extremely low in patients with negative perfusion scans, while reversible ischaemia actually predicted significant risk excess. Similarly, the relevance of stress perfusion abnormality—measured by SSS—documented a relevant prognostic power confirming the well-validated model predicting a direct relationship between maximal severity of hypoperfusion (due to either irreversibly damaged or reversibly ischaemic myocardium) and cardiovascular risk.
On the other hand, the additive prognostic value of ischaemia in risk stratification is particularly relevant since it directly reflects the expected benefit offered by revascularization. The present data indicate that prognostic penetrance of reversible perfusion defects can be improved beyond the SDS value by its normalization for exercise tolerance due to the peculiar physiological nature of exercise and its gradual effect on CBF (8, 17).
In the clinical setting, MPI is often combined with pharmacological stressors even in patients able to exercise. Nevertheless, both adenosine (18) and alpha 2 receptor agonists (19) intrinsically exert an all-or-none maximal vasodilation; similarly, the progressive vasodilator action of dipyridamole is too fast to allow any modulation (18). Under these conditions, SDS analysis most likely provides a more complete definition of jeopardized myocardium.
The present data do not permit one to define whether the physiological nature of CPI or PPI and their close proximity to daily triggers of ischaemia actually make physical exercise a preferable stressor with respect to pharmacological vasodilation. This point is crucial in the modern era in which the best approach to interrogate extension of jeopardized myocardium is often a difficult choice (20). Actually, an extensive literature documented that techniques alternative to radionuclide MPI offer peculiar advantages: the lack of radiation exposure offered by echocardiography and magnetic resonance imaging (21, 22) allows a greater repeatability, the impressive increase in spatial resolution offered by magnetic resonance imaging markedly increases the diagnostic accuracy of stress MPI (23), while the possibility to match flow distribution and coronary anatomy, offered by computed tomography, will surely provide a more complete window on CAD severity (24). On the other hand, the peculiar nature of perfusion tracers and their optimal conjugation with physical exercise represent an almost exclusive feature of radionuclide MPI that might improve accuracy of risk prediction with respect to alternative ischaemia imaging strategies. This potential advantage couples the well-documented prognostic penetrance of ischaemic threshold evaluated by the Duke treadmill score (13) with an accurate definition of extension and site of jeopardized myocardium as prerequisite for revascularization.
Obviously, further studies are needed to define clinical conditions that are the best targets for this approach considering the possible interference of microvascular dysfunction on its prognostic penetrance. Actually, this disorder occurs in most patients with diabetes (25), dyslipidaemia, hypertension (26) or coronary atherosclerosis itself (27). Obviously, the prognostic impact of these conditions—that were largely represented in our study cohort—was accounted for in the Framingham risk score. Nevertheless, their interference with coronary microcirculatory function can affect diagnostic performance of SDS. In this line, normalizing for ischaemic threshold might at least partially reduce the impact of false-positive findings.
Conclusion
The present study indicates that accounting for RPP at tracer injection significantly improves the prognostic impact of SDS analysis in exercise MPI. Under many aspects, it confirms the common-sense approach considering ischaemic threshold as a main descriptor of clinical status whose prognostic value is nicely complemented by the description of ischaemia site, severity and extension offered by SDS. These data do not elucidate, in any way, whether accounting for this added value of exercise justifies the selection of this stress type. Nevertheless, the independent prognostic value of our analysis, its easy applicability and its adherence to the daily triggers of ischaemia have the potential to improve the clinical utilization of MPI.
References
Shaw LJ, Hage FG, Berman DS, Hachamovitch R, Iskandrian A. Prognosis in the era of comparative effectiveness research: where is nuclear cardiology now and where should it be? J Nucl Cardiol 2012;19:1026–43.
Gibbons RJ. Noninvasive diagnosis and prognosis assessment in chronic coronary artery disease: stress testing with and without imaging perspective. Circ Cardiovasc Imaging 2008;1:257–69.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Cabico JA, Friedman J, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: incremental prognostic value and use in risk stratification. Circulation 1996;93:905–14.
Berman DS, Kang X, Van Train KF, Lewin HC, Cohen I, Areeda J, et al. Comparative prognostic value of automatic quantitative analysis versus semiquantitative visual analysis of exercise myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1998;32:1987–95.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535–43.
Vanzetto G, Ormezzano O, Fagret D, Comet M, Denis B, Machecourt J. Long-term additive prognostic value of thallium-201 myocardial perfusion imaging over clinical and exercise stress test in low to intermediate risk patients: study in 1137 patients with 6-year follow-up. Circulation 1999;100:1521–7.
Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J 1973;85:546–62.
Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev 2008;88:1009–86.
Acampa W, Petretta M, Florimonte L, Mattera A, Cuocolo A. Prognostic value of exercise cardiac tomography performed late after percutaneous coronary intervention in symptomatic and symptom-free patients. Am J Cardiol 2003;91:259–63.
Hesse B, Tägil K, Cuocolo A, Anagnostopoulos C, Bardiés M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855–97.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539–42.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–47.
Mark DB, Shaw L, Harrell FE, Hlatky MA, Lee KL, Bengtson JR, et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med 1991;325:849–53.
Sharir T, Germano G, Kang X, Lewin HC, Miranda R, Cohen I, et al. Prediction of myocardial infarction versus cardiac death by gated myocardial perfusion SPECT: risk stratification by the amount of stress-induced ischemia and the poststress ejection fraction. J Nucl Med 2001;42:831–7.
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation 2013;128:1634–43.
Grambsch P, Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515–26.
Heusch G. Heart rate in the pathophysiology of coronary blood flow and myocardial ischaemia: benefit from selective bradycardic agents. Br J Pharmacol 2008;153:1589–601.
Rossen JD, Quillen JE, Lopez AG, Stenberg RG, Talman CL, Winniford MD. Comparison of coronary vasodilation with intravenous dipyridamole and adenosine. J Am Coll Cardiol 1991;18:485–91.
Mekkaoui C, Jadbabaie F, Dione DP, Meoli DF, Purushothaman K, Belardinelli L, et al. Effects of adenosine and a selective A2A adenosine receptor agonist on hemodynamic and thallium-201 and technetium-99m-sestaMIBI biodistribution and kinetics. JACC Cardiovasc Imaging 2009;2:1198–208.
Bonow RO. Sixth Annual Mario S. Verani, MD Memorial Lecture: Cardiovascular imaging—added value or added cost? J Nucl Cardiol 2008;15:170–7.
Cortigiani L, Bigi R, Landi P, Bovenzi F, Picano E, Sicari R. Prognostic implication of stress echocardiography in 6214 hypertensive and 5328 normotensive patients. Eur Heart J 2011;32:1509–18.
Heitner JF, Klem I, Rasheed D, Chandra A, Kim HW, Van Assche LM, et al. Stress cardiac MR imaging compared with stress echocardiography in the early evaluation of patients who present to the emergency department with intermediate-risk chest pain. Radiology 2014;271:56–64.
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 2012;379:453–60.
Wong DTL, Ko BS, Cameron JD, Leong DP, Leung MCH, Malaiapan Y, et al. Comparison of diagnostic accuracy of combined assessment using adenosine stress computed tomography perfusion + computed tomography angiography with transluminal attenuation gradient + computed tomography angiography against invasive fractional flow reserve. J Am Coll Cardiol 2014;63:1904–12.
Marini C, Bezante G, Gandolfo P, Modonesi E, Morbelli SD, Depascale A, et al. Optimization of flow reserve measurement using SPECT technology to evaluate the determinants of coronary microvascular dysfunction in diabetes. Eur J Nucl Med Mol Imaging 2010;37:357–67.
Sambuceti G, Parodi O. Role of coronary microvascular abnormalities in coronary artery disease—implications for perfusion imaging. J Nucl Cardiol 1995;2:78–84.
Sambuceti G, Marzullo P, Giorgetti A, Neglia D, Marzilli M, Salvadori P, et al. Global alteration in perfusion response to increasing oxygen consumption in patients with single-vessel coronary artery disease. Circulation 1994;90:1696–705.
Acknowledgments
The study has been supported by CARIGE Foundation within the program: “Studio Medico Nucleare di Variabili fisiologiche di interesse oncologico”.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marini, C., Acampa, W., Bauckneht, M. et al. Added prognostic value of ischaemic threshold in radionuclide myocardial perfusion imaging: a common-sense integration of exercise tolerance and ischaemia severity. Eur J Nucl Med Mol Imaging 42, 750–760 (2015). https://doi.org/10.1007/s00259-014-2963-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2963-8