Abstract
Background
Some specifics of cardiac stress protocols, i.e., stressor used or exercise level achieved, may impact myocardial perfusion imaging (MPI) accuracy.
Methods
Four-hundred and seventy-five patients were submitted to MPI and coronary angiography. MPI was performed after exercise (303 patients) or dipyridamole stress (172 patients). A coronary stenosis ≥70% was considered significant. In case of exercise test, a peak heart rate (HR) <85% of the maximal age predicted was considered submaximal and categorized as follows: >75% and <85% (“Group 1”); <75% (“Group 2”).
Results
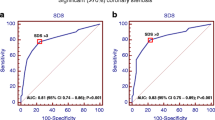
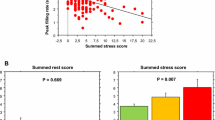
At coronary angiography, 312/475 (66%) patients showed significant stenosis. In the overall population, MPI showed a high accuracy in unmasking significant coronary stenosis, independently of the stress protocol adopted (AUC .76 for exercise vs .78 for vasodilator; P = NS). However, in case of an exercise stress test, a significant interaction between peak %HR and MPI diagnostic power was evident. While an elevated accuracy was still maintained in “Group 1” patients (AUC .79; P vs maximal exercise = NS), a significant drop was demonstrated in “Group 2” patients (AUC .66; P vs maximal exercise = .012, and P vs “Group 1” = .042).
Conclusions
The accuracy of MPI is not influenced by the stress protocol adopted. Exercise MPI maintains an elevated accuracy as long as the %HR remains >75%.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion imaging (MPI) on single-photon emission computed tomography (SPECT) is considered as a reference method for the evaluation of patients with suspected or known coronary artery disease (CAD),1 offering the opportunity to combine a semi-quantitative assessment of regional myocardial perfusion and to derive measures of the hemodynamic relevance of a coronary stenosis.2 When performed in association with an exercise stress test, SPECT-MPI allows integrating left ventricular (LV) perfusion and functional information with the assessment of relevant measures of patients global cardio-respiratory fitness and effort tolerance, which in turn may predict adverse outcome.3,4
Nevertheless, despite the theoretical superiority of an exercise stress test, a relevant proportion of MPI evaluations is performed under a pharmacological stressor, i.e., a vasodilator, that gives the chance to perform a standardized stress protocol also in patients with contraindication to exercise testing, i.e., non-interpretable ECG, or unable to exercise sufficiently.5
To this respect, it is classically believed that in the case of a submaximal exercise protocol, i.e., with <85% of the predicted maximal heart rate (HR), the accuracy of SPECT-MPI would fall significantly, due to a higher incidence of false-negative results.6,7 Specifically, in these cases, a pharmacological stressor is generally considered as a more reliable test for the evaluation of ischemic susceptibility.5,8
However, although a similar accuracy in unmasking the presence of relevant CAD has been reported, the two stress test modalities are characterized by a significantly different prognostic impact, since an exercise SPECT appears to better predict patients’ long-term outcome.9
Moreover, some studies have also suggested how SPECT-MPI may still hold an acceptable diagnostic accuracy also when performed after a submaximal exercise stress test.10–12
To this respect, despite some previous evidences,11,12 a consistent evaluation of the effects of cardiac stress protocol parameters, i.e., exercise tolerance, on MPI diagnostic accuracy in a large population of patients with suspected ischemic heart disease (IHD) is still warranted.
We sought to assess the relationships between cardiac stress protocols and MPI diagnostic accuracy in patients with suspected or known CAD and to determine the interaction among exercise tolerance and MPI-related diagnostic power.
Materials and Methods
Patient Population
Among the patients referred to our institution between 2011 and 2014 for myocardial scintigraphy on a cadmium-zinc-telluride (CZT) camera followed by coronary angiography, we retrospectively selected all the subjects (475 patients) with anginal chest pain and known (160 patients, 34%) or suspected CAD (315 patients, 66%). Specifically, 85 patients (all with normal ejection fraction (EF) and a summed stress score <5) were submitted to computed tomography (CT) coronary angiography, while the remaining 390 underwent invasive coronary angiography, according to our routine clinical protocol and/or as indicated by the referring physicians. A coronary stenosis ≥70% was considered significant. The time interval between coronary angiography and CZT study was ≤3 months. Exclusion criteria were hemodynamic instability, severely symptomatic heart failure, myocardial inflammatory disease, and more than moderate valvular disease. The study was approved by the Local Ethical Committee and conformed to the Declaration of Helsinki on human research. Written informed consent was obtained from every patient after explanation of the protocol, its aims, and potential risks.
Stress Protocols
Patients discontinued beta-blockers, calcium-antagonists, and nitrates from 24 to 48 hour before testing. Three-hundred and three patients (64%) underwent symptom-limited bicycle exercise test (stepwise increments of 25 W every 2 minute) while 172 patients (36%) dipyridamole stress testing (.56 mg/kg IV over 4 minute). Of the patients undergoing exercise stress test, 95 reached >85% of the age-predicted maximum HR, while 208 did not. Among those, in 129 (62%) patients, exercise test was ended because of stress-induced severe chest pain and/or significant ST segment depression. The stress protocol was completed in each patient without adverse events. In each patient, the rate pressure product at peak stress (HR × systolic blood pressure) was computed and considered maximal if ≥30,000.13
Acquisition Protocol
Patients underwent stress/rest CZT (Discovery NM 530c; GE Healthcare, Haifa, Israel) imaging according to a single-days protocol with the administration of 185-222 MBq of 99mTc-tetrofosmin during stress and 370-444 MBq at rest. Patients with known prior myocardial infarction were injected at rest after sublingual administration of nitrates.14,15
Stress-CZT imaging was performed 10-15 minute after injection of the radiopharmaceutical with an acquisition time of 7 minute. Patients were injected at rest 30 minute after the end of the first acquisition and then after an interval of 30-45 minute, a second acquisition was carried out for 6 minute. Image acquisition times were calculated in order to obtain a number of counts generally acquired by the same CZT camera after a standard tracer injection.14 Patients were imaged in the supine position with arms placed over their head without any detector or collimator motion. All images were acquired with a 32 × 32 matrix and a 20% energy window centered at the 140 keV photopeak of 99mTc (pixels width 4 mm).
List mode files were acquired, and images were reconstructed on a standard workstation (Xeleris II; GE Healthcare, Haifa, Israel) using a dedicated iterative algorithm with 50 iterations.15 A Butterworth post-processing filter (frequency .37, order 7) was applied to the reconstructed slices. The tomographic studies were also re-projected into 60 planar projections to emulate a standard SPECT layout. Images were reconstructed without scatter or attenuation correction.
Analysis of Perfusion Images
Perfusion images were semi-quantitatively scored according to the 17-segment LV model and a five-point scale (0-normal, 1-equivocal, 2-moderate, 3-severe reduction in radioisotope uptake, and 4 absence of detectable tracer uptake) and the summed stress score and summed rest score were calculated. Accordingly, the summed difference score (SDS), a measure of stress-induced reversible myocardial ischemia, was computed in every patient and considered pathological if >3.16 The same analysis was performed on a per-vessel basis and the difference score of each coronary territory calculated. Two experienced nuclear cardiologists performed the semi-quantitative analysis independently, and consensus was reached on all analyses.
Analysis of Gated Images
LV functional analysis was performed on 16-frame reformatted images using commercially available software (Corridor4DM, Invia, Ann Arbor, MI). End-diastolic volume (EDV), end-systolic volume, EF, and peak filling rate (PFR, EDV second−1) were calculated in every patient15,17,18 both at rest and during stress. In order to quantitate the magnitude of stress-induced LV functional impairment, the “% Stress-to-Rest” ratios of EF and PFR were calculated.
Invasive and CT Coronary Angiography
Invasive coronary angiography was performed using standard techniques and multiple projections. Coronary angiograms were quantified with a dedicated computer software (Advanced Vessel Analysis, Innova 3DXR for Advanced Workstations; GE Healthcare) using an automatic edge-contour detection algorithm to compute stenosis severity. CT coronary angiography was performed on a 64-slice scanner (GE Discovery VCT; GE Healthcare) or on a 320-slice scanner (Aquilon one, Toshiba). The data were then transferred to dedicated workstations for post-processing. Stenosis severity was measured on Multiplanar Reformatting Images using an automatic interactive program to quantify coronary luminal narrowing and expressed with intervals of 5%.19 In vessels showing multiple stenosis in series, only the most severe was considered.
Statistical Analysis
Continuous variables were expressed as mean ± SD and categorical variables as percentages. Groups were compared for categorical data using Fisher’s exact test and for continuous variables using analysis of variance followed by Fisher’s protected least significant difference for multiple comparisons. All tests were 2-sided; a P < .05 was considered significant. The accuracy of CZT-derived SDS in unmasking the presence of significant coronary stenosis was assessed at receiving operating characteristic (ROC) analysis and the area under the curve (AUC) and the relative 95% CI were determined. Specifically, the interaction between specific stress protocols, exercise vs vasodilator test, and CZT accuracy was determined. Moreover, in patients submitted to an exercise stress test, the impact of exercise level and diagnostic accuracy was determined. Therefore, patients with a submaximal exercise (<85% of predicted maximal HR) were divided according to the median value of %HR distribution and categorized as follows: “Group 1” (<85% and >75% of predicted %HR), and “Group 2” (<75% of predicted %HR).
Statistical analyses were performed using JMP (SAS Institute Inc, version 4.0.0) and Stata (version 13, StataCorp, College Station, TX).
Results
Characterization of the Population
The characteristics of the overall study population are reported in Table 1. As expected, patients who underwent a vasodilator stress test were significantly older (P < .001) and relatively more obese (P = .003) than those submitted to an exercise test. At coronary angiography, 312/475 (66%) patients presented a significant coronary stenosis in one (129, 41%), two (106, 34%), or three (77, 25%) vessels with no significant difference between the two patients categories. Specifically, coronary findings at CT and invasive angiography, as considered separately, are reported in Table 2.
Association Between Stress Protocol and MPI Accuracy: Exercise Vs Vasodilator
In the overall population, a significant association between increasing CAD extent and more impaired measures of myocardial perfusion and function was evident (Table 3). Accordingly, the interaction among the different MPI stress protocols and patients clinical and functional variables was further investigated. There was not any significant difference regarding resting LV functional parameters between patients who underwent an exercise or a vasodilator stress test (Table 4). However, patients submitted to an exercise test more frequently showed signs of myocardial ischemia on stress ECG (P = .008) as well as significantly higher values of SDS and stress-induced LV functional impairment (Table 4). Interestingly, the difference in terms of ischemic burden on MPI between exercise and vasodilator stress was limited to patients with multi-vessel disease (SDS: 7 ± 4 in vasodilator vs 8 ± 4 in exercise stress, P = .05) while disappeared in those with single-vessel CAD.
Nevertheless, at ROC analysis (Figure 1), the two stress modalities showed a similar accuracy in unmasking the presence of significant coronary stenosis.
Interaction Among Exercise Level and MPI Accuracy
Of the 208 patients who performed a submaximal exercise level, 103 attained a %HR >75% (“Group 1”), while 105 were injected despite a %HR <75% (“Group 2”). The latter patients were significantly older (69 ± 9 years and 66 ± 9 years for “Group 2” and “Group 1,” respectively) and more frequently obese (31% and 35%, for “Group 1” and “Group 2,” respectively) than subjects that performed a maximal exercise (66 ± 10 years and 20% obese; P < .05 for both). No significant difference in the incidence of stress-induced clinical or ECG-graphical signs of ischemia was evident between the groups. Similarly, no significant difference in the extent of significant CAD was evident between “Group 2” patients and those who performed a maximal exercise. As expected patients, individual RPP at peak stress was strictly related to the attained exercise level (25,777 ± 4405 bpm·mmHg in patients with a maximal exercise, 21,178 ± 4849 bpm·mmHg in “Group 1”, and 117,543 ± 4388 bpm·mmHg in “Group 2”; P < .001), with only 2/103 (2%) and 0/105 (0%) patients reaching a RPP ≥ 30,000 in “Group 1” and “Group 2,” respectively.
The interaction among exercise level and CZT accuracy in unmasking significant CAD was assessed (Figure 2). While “Group 1” patients showed a similar diagnostic accuracy as those with a maximal exercise, in patients with significantly impaired HR response (“Group 2”), MPI diagnostic power was considerably diminished because of a significantly lower sensitivity (71% in “Group 2” vs 85% in “Group 1” and 84% in “maximal exercise”; P = .023 vs “Group 1” and P = .044 vs “maximal exercise”). To this respect, in “Group 2” patients, the underestimation of the ischemic burden was particularly evident in the presence of multi-vessel CAD (Figure 3).
Interestingly, as the analysis was limited to the patients with submaximal exercise but clinical evidence of stress-induced myocardial ischemia (angina and/or ST segment depression), CZT-MPI presented a similar accuracy in unmasking significant CAD in both “Group 1” (AUC .84, 95% CI .73-.92) and “Group 2” (AUC .76, 95% CI .63-.85; P = NS) subjects. On the other hand, in patients in whom exercise was ended because of fatigue the accuracy of CZT-MPI was significantly higher in “Group 1” (AUC .74, 95% CI .62-.83) than in “Group 2” (AUC .54, 95% CI .41-.67, P = .04) patients.
Discussion
Our study shows that MPI performed on a dedicated CZT camera has an elevated accuracy in unmasking the presence of significant CAD, independently from the stress protocol employed. Specifically, the present results suggest that an excellent diagnostic power is maintained also in the case of a moderately submaximal exercise stress test, as long as the 75% of the maximal predicted HR is reached.
MPI and CAD: The Value of the Stress Test Protocol
MPI on SPECT has become a reference for the non-invasive estimation of the presence of significant CAD,5 allowing an accurate evaluation of regional myocardial blood flow regulation together with quantitative measures of LV function.1,15,17 To this respect, when combined with an exercise stress test, MPI offers the chance to acquire information on both individual ischemic threshold and on key parameters of patients’ effort tolerance, allowing deriving prognostically relevant measures of patients’ cardio-respiratory fitness.3,4
Nevertheless, in a relevant proportion of patients (as high as 26%), an exercise stress test is not clinically feasible9; in this case, a pharmacological stress test, generally through a coronary vasodilator, may offer a similar accuracy in unmasking significant CAD.5
Our study sought to compare the relative accuracy of the two main MPI stress test protocols in the detection of significant CAD with the use of a novel dedicated camera equipped with stationary CZT detectors. As a matter of fact, those cameras are characterized by a significantly higher photon sensitivity and spatial resolution than standard SPECT devices, theoretically offering a more accurate evaluation of regional myocardial perfusion, despite a rapid acquisition time and a significantly reduced radiation burden.14,20
The present results confirmed the elevated accuracy of MPI in unmasking significant CAD, independently from the stress protocol used. Interestingly, the accuracy of CZT-MPI was maintained also in patients with a moderately reduced exercise tolerance (75% < %HR < 85%) even in the absence of clinical evidences of myocardial ischemia, suggesting its possible clinical role also in patients with a submaximal exercise stress test.
Cardiac Workload and MPI Accuracy
It is generally believed that a submaximal exercise stress MPI has a limited accuracy in detecting significant CAD,6,7 although this concept has been questioned by some.11 Accordingly, in these patients, a pharmacological stress test is generally warranted, either alone or in conjunction with low-level exercise.7,21 On the other hand, the significant inferiority of vasodilator MPI with respect to exercise stress SPECT in terms of patients’ risk stratification has been repeatedly highlighted, and the clinical value of different accessorial information that an exercise stress test allows to obtain demonstrated.3,4,12,22
As previously reported, despite the theoretical diagnostic limitations of a submaximal exercise stress test, in a relevant proportion of patients (as high as 1 every 4), the widely accepted boundary of the 85% of the predicted maximal HR is not reached due to symptoms or physical exhaustion,8–10 making the trade-off between reduced diagnostic power and enhanced patients risk stratification, a clinically relevant question. Interestingly, it could be possible that the relatively superior accuracy and photon sensitivity of the recently introduced CZT-dedicated cardiac cameras14,18 could help to partially overcome these limitations, allowing a “diagnostic” MPI also in case of a relatively submaximal exercise level.
As a matter of fact, our data indicate that in a relevant proportion of patients with a nominally submaximal exercise level, the diagnostic accuracy of a state-of-the-art MPI with a novel CZT camera is maintained. On the other hand, in case of a significantly reduced cardiac workload, such as when <75% of the maximal HR is reached, a significant drop in accuracy is demonstrated because of a significantly lower diagnostic sensitivity. Specifically, our results indicate that, in the presence of clinical evidences of myocardial ischemia, the accuracy of exercise MPI remains elevated independently from the attained exercise level. On the other hand, in patients in whom exercise is terminated because of fatigue an acceptable accuracy is maintained as soon as the 75% of the predicted maximal HR is reached.
These results suggest that the conversion to a pharmacological stress test might be omitted in the case of a moderately submaximal exercise tolerance, allowing obtaining this exercise-related accessorial information on cardio-respiratory fitness also in patients usually submitted to a pharmacological stress test. This consideration might hold particularly true when a dedicated cardiac CZT camera is used for MPI since its increased sensitivity might allow a better assessment of myocardial ischemic burden also in patients with relatively submaximal exercise stress test. On the other hand, in patients who reach less than the 75% of the target HR without clinical signs of ischemia, the administration of low doses of atropine might increase MPI accuracy7 even though the predicted maximal HR is not reached, allowing to improve the diagnostic power in detecting CAD.
Interestingly, in the present study, CZT-MPI showed a relatively lower accuracy than previously reported.14 This result may be related to the fact that in our study, MPI was considered positive only in the presence of reversible myocardial ischemia. In fact, while the inclusion of myocardial scar as a diagnostic criterion would have increased the diagnostic power of MPI, ischemia represents by far a more clinically indicated measure of abnormal myocardial perfusion.
Limitations
The retrospective nature of the study may introduce the problem of a possible selection bias of the patients. However, as all the consecutive anginal patients submitted to CZT-MPI and coronary angiography were selected, the impact of this limitation should be considered low. Moreover, due to the consistent number of patients studied, the present data represent a close picture of the actual population of subjects submitted to MPI. The evaluation of post-stress measures of LV systolic and diastolic function is performed 10-15 minute after stress completion, probably underestimating the real magnitude of stress-induced LV functional impairment. However, considering the intrinsic timing of the present imaging protocol, a more precocious assessment of LV function seems unrealistic.
Moreover, in patients with preserved LV systolic function and limited myocardial ischemia (18% of the population), coronary anatomy was evaluated only at CT coronary angiography and some coronary stenoses could have been overlooked. Since this study was performed on a dedicated cardiac camera equipped with a relatively new technology of stationary CZT detectors, the present results might not be directly transferred to tradition SPECT devices. For instance, the specifics of the acquisition protocol employed and the radionuclide doses injected in the present study have been already validated in CZT cameras14,15,17,18 but cannot be adopted when traditional SPECT devices are adoperated.5 Finally, in the present study, the gold-standard used for the assessment of MPI accuracy was entirely anatomical. To this respect, we recognize that the use of a functional reference standard, such as invasive fractional flow reserve, would have better depicted the hemodynamic severity of a given coronary lesion. Accordingly, a relatively conservative positivity criterion for coronary angiography (≥70% stenosis) was selected in order to better identify only the clinically relevant coronary lesions.23
Conclusions
In patients with suspected IHD, MPI offers an elevated accuracy in unmasking the presence of significant CAD independently of the stress test protocol employed, i.e., exercise or vasodilator. A significant diagnostic power is maintained also in the case of a mildly submaximal exercise stress test as soon as a >75% of the predicted maximal HR is reached. These results might lead to a better protocol selection in patients submitted to MPI, expanding the indications of exercise test.
New Knowledge Gained
In patients with suspected or known coronary artery disease, myocardial perfusion imaging showed an elevated accuracy in unmasking the presence of significant coronary stenosis, independently of the stress protocol employed, i.e., exercise vs pharmacological, and also in the case of a moderately submaximal exercise test.
References
Parker MW, Iskandar A, Limone B, Perugini A, Kim H, Jones C, et al. Diagnostic accuracy of cardiac positron emission tomography versus single photon emission computed tomography for coronary artery disease: A bivariate meta-analysis. Circ Cardiovasc Imaging 2012;5:700-7.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900-7.
Rozanski A, Gransar H, Min JK, Hayes SW, Friedman JD, Thomson LE, et al. Long-term mortality following normal exercise myocardial perfusion SPECT according to coronary disease risk factors. J Nucl Cardiol 2014;21:341-50.
Bourque JM, Holland BH, Watson DD, Beller GA. Achieving an exercise workload of > or = 10 metabolic equivalents predicts a very low risk of inducible ischemia: Does myocardial perfusion imaging have a role? J Am Coll Cardiol 2009;54:538-45.
Hesse B, Tägil K, Cuocolo A, Anagnostopoulos C, Bardiés M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855-97.
Iskandrian AS, Heo J, Kong B, Lyons E. Effect of exercise level on the ability of thallium-201 tomographic imaging in detecting coronary artery disease: Analysis of 461 patients. J Am Coll Cardiol 1989;14:1477-86.
Manganelli F, Spadafora M, Varrella P, Peluso G, Sauro R, Di Lorenzo E, et al. Addition of atropine to submaximal exercise stress testing in patients evaluated for suspected ischaemia with SPECT imaging: A randomized, placebo-controlled trial. Eur J Nucl Med Mol Imaging 2011;38:245-51.
Verzijlbergen JF, Vermeersch PH, Laarman GJ, Ascoop CA. Inadequate exercise leads to suboptimal imaging. Thallium-201 myocardial perfusion imaging after dipyridamole combined with low-level exercise unmasks ischemia in symptomatic patients with non-diagnostic thallium-201 scans who exercise submaximally. J Nucl Med 1991;32:2071-8.
Navare SM, Mather JF, Shaw LJ, Fowler MS, Heller GV. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: A meta-analysis. J Nucl Cardiol 2004;11:551-61.
Schinkel AF, Boiten HJ, van der Sijde JN, Ruitinga PR, Sijbrands EJ, Valkema R, et al. 15-Year outcome after normal exercise 99mTc-sestamibi myocardial perfusion imaging: What is the duration of low risk after a normal scan? J Nucl Cardiol 2012;19:901-6.
Brown KA, Rowen M. Impact of antianginal medications, peak heart rate and stress level on the prognostic value of a normal exercise myocardial perfusion imaging study. J Nucl Med 1993;34:1467-71.
Esquivel L, Pollock SG, Beller GA, Gibson RS, Watson DD, Kaul S. Effect of the degree of effort on the sensitivity of the exercise thallium-201 stress test in symptomatic coronary artery disease. Am J Cardiol 1989;63:160-5.
Berman JL, Wynne J, Cohn PF. A multivariate approach for interpreting treadmill exercise tests in coronary artery disease. Circulation 1978;58:505-12.
Gimelli A, Bottai M, Giorgetti A, Genovesi D, Kusch A, Ripoli A, et al. Comparison between ultrafast and standard single-photon emission CT in patients with coronary artery disease: A pilot study. Circ Cardiovasc Imaging 2011;4:51-8.
Gimelli A, Liga R, Pasanisi EM, Giorgetti A, Marras G, Favilli B, et al. Evaluation of left ventricular diastolic function with a dedicated cadmium-zinc-telluride cardiac camera: Comparison with Doppler echocardiography. Eur Heart J Cardiovasc Imaging 2014;15:972-9.
Gutstein A, Navzorov R, Solodky A, Mats I, Kornowski R, Zafrir N. Angiographic correlation of myocardial perfusion imaging with half the radiation dose using ordered-subset expectation maximization with resolution recovery software. J Nucl Cardiol 2013;20:539-44.
Giorgetti A, Masci PG, Marras G, Rustamova YK, Gimelli A, Genovesi D, et al. Gated SPECT evaluation of left ventricular function using a CZT camera and a fast low-dose clinical protocol: Comparison to cardiac magnetic resonance imaging. Eur J Nucl Med Mol Imaging 2013;40:1869-75.
Gimelli A, Liga R, Bottai M, Pasanisi EM, Giorgetti A, Fucci S, et al. Diastolic dysfunction assessed by ultra-fast cadmium-zinc-telluride cardiac imaging: Impact on the evaluation of ischaemia. Eur Heart J Cardiovasc Imaging 2015;16:68-73.
Liga R, Marini C, Coceani M, Filidei E, Schlueter M, Bianchi M, et al. Structural abnormalities of the coronary arterial wall—in addition to luminal narrowing—affect myocardial blood flow reserve. J Nucl Med 2011;52:1704-12.
Herzog BA, Buechel RR, Katz R, Brueckner M, Husmann L, Burger IA, et al. Nuclear myocardial perfusion imaging with a cadmium-zinc-telluride detector technique: Optimized protocol for scan time reduction. J Nucl Med 2010;51:46-51.
Parker MW, Morales DC, Slim HB, Ahlberg AW, Katten DM, Cyr G, et al. A strategy of symptom-limited exercise with regadenoson-as-needed for stress myocardial perfusion imaging: A randomized controlled trial. J Nucl Cardiol 2013;20:185-96.
He ZX, Dakik HA, Vaduganathan P, Qureshi U, Mahmarian JJ, Verani MS. Clinical and angiographic significance of a normal thallium-201 tomographic study in patients with a strongly positive exercise electrocardiogram. Am J Cardiol 1996;78:638-41.
Chen ML, Mo YH, Wang YC, Lo HS, Wang PC, Chao IM, et al. 64-slice CT angiography for the detection of functionally significant coronary stenoses: Comparison with stress myocardial perfusion imaging. Br J Radiol 2012;85:368-76.
Disclosure
Alessia Gimelli, Riccardo Liga, Emilio Maria Pasanisi, Mirta Casagranda, Michele Coceani, and Paolo Marzullo declare no relationships with industry or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alessia Gimelli and Riccardo Liga have contributed equally to this study as first co-authors.
See related editorial, doi:10.1007/s12350-015-0119-2.
Rights and permissions
About this article
Cite this article
Gimelli, A., Liga, R., Pasanisi, E.M. et al. Influence of cardiac stress protocol on myocardial perfusion imaging accuracy: The role of exercise level on the evaluation of ischemic burden. J. Nucl. Cardiol. 23, 1114–1122 (2016). https://doi.org/10.1007/s12350-015-0101-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0101-z