Abstract
Available literature on the differences in circulation and microcirculation of normal liver and liver metastases as well as in rheology of the different radiolabelled microspheres [99mTc-labelled macroaggregates of albumin (MAA), 90Y-TheraSpheres and 90Y-SIR-spheres] used in selective internal radiation therapy (SIRT) are reviewed and implications thereof on the practice of SIRT discussed. As a result of axial accumulation and skimming, large microspheres are preferentially deposited in regions of high flow, whereas smaller microspheres are preferentially diverted to regions of low flow. As flow to normal liver tissue is considerably variable between segments and also within one segment, microspheres will be delivered heterogeneously within the microvasculature of normal liver tissue. This non-uniformity in microsphere distribution in normal liver tissue has a significant “liver-sparing” effect on the dose distribution of 90Y-labelled microspheres. Arterial flow to liver metastases is most pronounced in the hypervascular rim of metastases, followed by the smaller metastases and finally by the central hypoperfused region of the larger metastases. Because of the wide variability in size of labelled MAAs and because of the skimming effect, existing differences in flow between metastatic lesions of variable size are likely exaggerated on 99mTc-MAA scintigraphy when compared to 90Y-TheraSpheres and 90Y-SIR-spheres (smaller variability in size and probably also in specific activity). Ideally, labelled MAAs would contain a size range similar to that of 90Y-SIR-spheres or 90Y-TheraSpheres. Furthermore, the optimal number of MAA particles to inject for the pretreatment planning scintigraphy warrants further exploration as it was shown that concentrated suspensions of microspheres produce more optimal tumour to normal liver distribution ratios. Finally, available data suggest that the flow-based heterogeneous distribution of microspheres to metastatic lesions of variable size might be optimized, that is rendered more homogeneous, through the combined use of angiotensin II and degradable starch microspheres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is the most common site of visceral metastases for a variety of human malignancies; up to 25 % of cancer patients will develop hepatic metastases during the course of their disease and the majority of patients dying from cancers originating in structures whose venous drainage is through the portal circulation will show evidence of metastatic liver disease at the time of death [1, 2]. Less than 25 % of the patients presenting with liver metastases are amenable to surgery [3]. In the remaining patients chemotherapy and external beam radiotherapy will only provide palliation [4, 5]. In spite of the availability of various treatment options, due to their late discovery, liver metastases prove difficult to eradicate. Selective internal radiation therapy (SIRT) or transarterial radioembolization using 90Y-labelled microspheres is a promising treatment modality for the treatment of metastatic liver cancer [6, 7]. The technique involves the intra-arterial injection of commercially available 90Y-labelled microspheres via the hepatic artery or a side branch thereof; liver metastases are primarily fed via the hepatic artery, whereas normal liver tissue is fed primarily via the portal vein and up to three times more hepatic arterial vessels surround tumourous liver lesion when compared to normal liver tissue [9, 10]. 90Y is a pure β emitter with maximum β energy of 2.28 MeV and average β energy of 934 keV per disintegration. It has a half-life of 64.2 h and it decays into the stable element 90Zr. The range of tissue penetration of the emissions is 2.5–11 mm. Two types of 90Y-labelled microspheres are commercially available: SIR-spheres and TheraSpheres. SIR-spheres are non-biodegradable 90Y-labelled resin microspheres with a diameter of 20–40 μm [8, 9]. A typical administration involves 20–40 million microspheres each of which carries approximately 40–70 Bq of 90Y; maximal available activity is 3 GBq. TheraSpheres® (MDS Nordion, Ottawa, Canada) are non-biodegradable glass microspheres with diameters ranging between 20 and 30 μm. At the time of calibration, each microsphere has an activity of 2,500 Bq. Six different vials are available; maximal available activity is 20 GBq. More recently, customized TheraSphere vials were also made available. The difference in the vials is the number of spheres, e.g. 1.2 million microspheres are present in a vial with an activity of 3 GBq. Based on their size, both types of microspheres are believed to gain entry into tumour nodules but will not pass through the end capillary bed into the venous circulation and thus will become trapped in the tumour capillary bed, selectively delivering radiation to the tumour tissue whilst relatively sparing normal tissue.
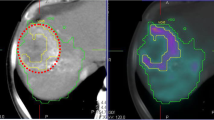
In order to confirm access to areas of the liver that need to be treated with 90Y-labelled microspheres and in order to isolate liver from other foregut structures, prior to SIRT, a 99mTc-macroaggregated albumin (MAA) scan is performed; MAA particles are deemed to have a comparable size to 90Y-labelled microspheres and their biodistribution is assumed to be similar provided they are injected under comparable conditions [10, 11]. Furthermore, as 99mTc-MAA particles are believed to have a biodistribution comparable to 90Y-labelled microspheres, 99mTc-MAA tumour to normal tissue ratios might be predictive of therapy response; the selective delivery of a high dose of radiation to malignant liver lesions following infusion of 90Y-labelled microspheres while sparing non-tumourous liver lesions depends on their tumour to non-tumourous liver parenchyma uptake ratio. In this regard, three recent publications showed that in SIRT of hepatocellular carcinoma using 90Y-TheraSpheres, 99mTc-MAA single photon emission computed tomography (SPECT)/CT is accurately predictive of tumoural response and even of survival in one paper. Similar results may be expected for treatment of liver metastases as the therapeutic effect comes from radiation, at least with 90Y-TheraSpheres; 90Y-SIR-spheres will also embolize the metastases given the high number of microspheres injected [12–14].
In this paper, available literature on the differences in circulation and microcirculation of normal liver and liver metastases as well as in rheology of the different radiolabelled microspheres used in SIRT are reviewed and implications thereof on the practice of SIRT discussed. Additionally, potential options for modulation of SIRT using angiotensin II and degradable starch microspheres (DSM) are discussed.
Circulation and microcirculation of normal liver and liver metastases
Circulation and microcirculation in the normal liver
The adult human liver weighs approximately 1,500 g and obtains it blood via a dual supply; hepatic blood accounts for 10–15 % of the total blood volume [15]. Approximately 60–80 % of hepatic blood is derived from the gastrointestinal tract via the portal vein and 40–20 % from the systemic circulation via the hepatic artery [16–19]. Mean regional arterial blood flow in the lateral, medial, anterior and posterior liver segments approximates 37.6, 30.0, 28.2 and 31.6 ml/min per 100 g, respectively [20]. Mean regional portal hepatic blood flow in the same segments approximates 29.8, 43.4, 50.0 and 40.9 ml/min per 100 g, respectively [20]. Terminal branches of the hepatic portal vein and hepatic artery with a diameter of 15–35 μm and a length of 50–70 μm empty together and mix as they enter the liver sinusoids (average diameter 5 μm), distensible vascular channels lined with highly fenestrated endothelial cells (sinusoidal endothelial fenestrae, SEFs) and bounded circumferentially by hepatocytes, from which the blood is then conveyed to the inferior vena cava by the hepatic veins. In addition, hepatic arterioles wind themselves around the portal venules sending short branches to the portal venules (vasa vasorum) and to capillaries of the peribiliary plexus. They further drain into sinusoids via arteriosinus twigs. Finally, direct arterioportal anastomoses have been reported
The valveless portal vein is a low pressure (6–10 mmHg)/low resistance system that largely depends on the degree of constriction or dilatation of the mesenteric and splanchnic arterioles and to a lesser degree on atrial pressure [18]. Splanchnic resistance may increase linearly with increases in portal pressure. In contrast, the hepatic artery supplies the liver with arterial blood via a high pressure (mean pressure similar to that of the aorta)/high resistance system that depends on cardiac output and on the degree of arterial inflow resistance to other vascular beds [19]. Based on direct blood pressure measurements by micropuncture, the blood pressure in the terminal hepatic arteriole is at least 22–29 mmHg, which in the portal venule is 3.7 mmHg, while the sinusoidal pressure is estimated to be as low as 0.7–1.5 mmHg [20]. At the entry of the hepatic sinusoids two sphincter-like structures, one located at the junction between the terminal portal venule and the sinusoid characterized by large endothelial cells surrounded with Ito cells (hepatic stellate cells, HSCs) and one at the junction between the terminal hepatic arteriole and the sinusoid corresponding to the precapillary sphincter, help to regulate local control of hepatic sinusoidal blood flow [21, 22]. It is essential for the local control of hepatic sinusoidal blood flow that the dynamic contracting and relaxing changes not only in these inlet sphincter-like structures but also in the SEFs correspond with those of the HSCs, both of which are mediated by the sinusoidal endothelium-derived vasoconstrictor endothelins (ETs) and vasodilator nitric oxide (NO) [23].
Importantly, the hepatic arterial resistance may change so as to buffer the effect of portal or arterial flow alterations on total hepatic blood flow, a mechanism coined by Ezzat and Lautt as the “hepatic arterial buffer response” that is believed to be mediated predominantly via adenosine washout [15, 18, 24]. Adenosine is produced at a constant rate, independent of oxygen supply or demand, and secreted into a small fluid compartment, termed the space of Mall, that surrounds the hepatic arterial resistance vessels. If portal vein flow decreases, less adenosine is washed away into the portal blood and the accumulated adenosine leads to hepatic arterial dilation. Similarly, hepatic arterial autoregulation operates by the same mechanism, whereby a decrease in arterial pressure leads to a decrease in hepatic arterial flow, thus resulting in less adenosine washout into the hepatic artery blood. The accumulated adenosine leads to hepatic artery dilation [25, 26]. These intrinsic regulatory mechanisms tend to maintain total hepatic blood flow at a constant level, thus stabilizing hepatic clearance of hormones, venous return and cardiac output. The hepatic arterial buffer response is capable of buffering a decrease in portal flow of 25–60 %.
Circulation and microcirculation of liver metastases
Animal models
Haemodynamics of liver metastases differ significantly from that of normal liver tissue. Overall, available data suggest the lack of autoregulation at the level of the liver sinusoids in liver metastases and activation of the hepatic arterial buffer response.
Lack of autoregulation
As early as 1969, Krylova demonstrated that during tumour growth of liver metastases there is no development of smooth muscles in the neoplastic walls and that there is an absence of nervous elements and thus also of autoregulation [27]. Likewise, Mattsson et al. and Hafström et al. demonstrated the absence of adrenergic innervation of blood vessels of experimental tumours by means of histochemistry; quantitative estimations of noradrenaline contents proved to be close to zero [28, 29]. Wickersham et al. noticed that topical administration of adrenaline and noradrenaline caused a significant difference between normal and tumour tissue with no response in tumour vessels indicating a lack of smooth muscles and/or receptors [30].
Activation of the hepatic arterial buffer response
In a rat model of occult colorectal liver metastases, a decrease in hepatic arterial perfusion as well as in portal blood flow was evidenced, accompanied by a simultaneous increase in mean transit time suggesting a rise in intrahepatic resistance as underlying cause [31]. Similar findings were observed in a hypovascular HSN sarcoma liver metastases model [32]. Various factors may contribute to these findings [33, 34]. First, at the cellular level, tumour cell-driven activation of Kupffer cells in the space of Disse was shown to result in cytokine release and endothelial cell activation. Circulating leucocytes were shown to bind to these endothelial activated cells resulting in increased leucocyte rolling and flow stasis with metastases development. Flow stasis occurred prior to identification of visible tumours. Of interest, inhibition of receptors expressed on activated endothelial surfaces abrogated metastases formation. Second, because of size restriction, “microthrombotic” metastatic cells introduced via the portal vein will be arrested at the inflow side of the microvascular bed increasing intrahepatic pressure. Also, micrometastases may encircle portal venules and compress sinusoidal capillaries leading to an increase of portal pressure. Third, a circulating vasoactive agent inducing splanchnic vasoconstriction has been implicated; increased vascular resistance developed in rats in which small bowel segments were cross-perfused with arterial blood from rats bearing liver metastases [35]. Finally, as metastases grow larger and become macroscopic, portal hepatic blood flow further decreases due to an increase in intratumoural pressure as well as in the surrounding vasculature due to compression: tumour nodules are surrounded by compressed sinusoidal capillaries that resist portal flow [36–38]. Because of the reduction in portal flow an adaptive increase of liver perfusion via the hepatic artery is seen, resulting in an increase in the hepatic perfusion index. Importantly, arterial blood appears to enter tumours via the portal venules suggesting arterioportal communications play an important role in tumour blood supply; interruption of either the hepatic artery or the portal vein does not arrest blood circulation in liver metastases. Of interest, while the hepatic perfusion index increases, total hepatic blood flow is reduced.
Human data
Up to the size of 200 μm, liver metastases receive their main blood supply via sinusoids. Beyond this size neovascularization is induced by surrounding arterial and portal vessels [39]. Macroscopic liver metastases exhibit an irregular tortuous vascular network bordered by a vascular ring composed of compressed sinusoids. Similar to preclinical models, arterial blood appears to enter the metastases via the portal venules (through anastomoses) and drains out into the hepatic venules through the microvasculature [40–44]. Both the absolute and relative contribution of hepatic arterial blood flow to total hepatic flow are significantly increased in patients presenting with liver metastases. Conversely, portal vein blood flow is significantly reduced. While in non-malignant disease, arterial and hepatic flow are reciprocal due to the buffer effect, such a straightforward relationship is lacking in the presence of liver metastases. In fact in a study by Miles et al., arterial perfusion proved to be weakly, yet significantly correlated to portal perfusion, a reversal of the normal situation implying that neovascularization in liver metastases is disordered with admixture of arterial and portal blood in sinusoids no longer being present [45]. The lower portal values when compared to arterial values also imply that there is some hepatic venous drainage, albeit reduced. As shown by Haugeberg et al. following gelatin perfusion of the hepatic vein on human cadaver livers with metastases, the hepatic vein demonstrated venous drainage from peripheral areas of tumour in less than 30 % of metastases and from central tumour areas in only 9 % of liver metastases [39]. Larger branches of the hepatic vein were not detected within metastases. Of interest, in the same study, injection of the portal vein showed that more than 50 % of liver metastases had a distinct portal blood supply to the tumour periphery which in approximately one third of cases extended centrally. Likewise, using clearance and dynamic blood flow analysis by means of gamma camera imaging following injection of 133Xe into both hepatic arterial and portal venous catheters in patients undergoing surgery for colorectal cancer, Taylor et al. showed that while initial distribution images indicated a predominant arterial perfusion to the metastases, after manual hepatic artery ligation, portal vein perfusion to the metastases was significantly increased [41]. Similar results were obtained by Flowerdew et al. using dynamic first-pass imaging of 99mTc-sulphur colloid through the liver of 44 patients presenting with liver tumours [46]. The latter authors determined the relative arterial and portal components of regional hepatic blood flow following arterial embolization. Observations made were compared with those of 33 control subjects. Overall, these findings suggest the existence of a pressure-dependent flow system for liver metastasis. As arterial blood shunts into the portal venules at the tumour border, the high arterial pressure created within those vessels impedes the portal flow from entering the tumour. As soon as the arterial flow is interrupted, the high pressure is relieved and the portal flow increases to supply the tumour.
On the rheology of MAA and microspheres
In the mid-1960s Ueda et al. and Taplin et al. developed MAA spheres labelled with 131I, as markers for the multi-organ distribution of cardiac output [47, 48]. Later, MAA was labelled with 99mTc, in view of the advantages both in terms of radiation dosimetry and of imaging properties [49, 50]. Shortly after the introduction of MAA, radiolabelled microspheres were introduced by Rudolph and Heymann for examining regional blood flow in sheep fetuses in utero [51]. Some 10 years later, McDevitt and Nies demonstrated the potential of radiolabelled microspheres for measuring cardiac output in rodents and for estimating hepatic arterial flow [52]. Several authors have studied the impact of size, number and density on the distribution of radiolabelled spheres.
Sphere size
When flowing through arteries, radiolabelled microspheres of 15–80 μm diameter will concentrate centripetally [53–55]. This centripetal tendency becomes more pronounced as the ratio of microsphere diameter to vessel diameter increases and is largely due to the wall exclusion effect. Between a suspension that flows through a vessel, e.g. blood and artery, there is a zone which is relatively deficient in suspended material. This zone extends into the suspension for a distance comparable with the dimensions of the particles which it contains [56, 57]. The axial concentration of microspheres causes a skimming effect; the concentration of microspheres entering a side branch will be lower than that in the main channel [58]. Furthermore, as smaller spheres will tend to flow more peripherally when compared to larger ones, there will be a tendency for larger microspheres to be separated from the smaller microspheres by variations in arterial size and branching. At each branch point, microspheres will tend to enter the branch with the higher velocity and thus the fraction entering this branch will be larger than the fraction of flow which enters. In dog hearts, using microspheres of 15, 35 and 50 μm, the larger microspheres were preferentially deposited in regions of high flow [59, 60]. Similarly, the deposition of 35- and 50-μm microspheres in the outer renal cortex was greater than that of 15-μm microspheres, and deposition in the juxtamedullary region was relatively less for the larger microspheres when compared to small spheres [61]. Of interest, in the dog heart model, it was also suggested that the form of vessel branching had a negligible effect on microsphere distribution. The extent of embolization of differently sized radioactive microspheres in experimental tumours and the homogeneity of their distribution in normal liver was examined in 25 rats by Meade et al. [62]. The ratio of arterially introduced microspheres lodging in tumour tissue compared to the surrounding normal hepatic parenchyma was measured for 15-, 32.5- and 50-μm diameter tracer microspheres. The mean tumour to liver arterial perfusion ratio (T/L) for 15- and 32.5-μm spheres was approximately 3:1 in both cases and there was no significant difference between these values. However, 50-μm microspheres did not preferentially lodge in malignant tissue (mean T/L ratio 1:1). As microsphere diameter increased from 15 to 50 μm, microspheres lodged more evenly throughout the liver substance. For 15-μm microspheres the coefficient of variation was 55.5 ± 8.3 % and 32.5-μm microspheres distributed with a coefficient of 35 ± 16.8 %, while 50-μm spheres distributed most evenly with a coefficient of 19.7 ± 6.8 %.
Radioactivity versus sphere size
Whereas 90Y-TheraSpheres and 90Y-SIR-spheres have a relatively stable amount of radioactivity/sphere, this is probably not the case for MAA spheres when labelled with 99mTc. Provided that radiolabelling of MAA spheres occurs through interaction with thiolate groups and imidazole-containing groups on their surface, doubling sphere size will increase the average radioactivity of a sphere by a factor of 4 given the surface area of the sphere is directly proportional to the square of its radius [50]. As such a sphere of 40-μm diameter will contain 16 times more radioactivity when compared to a sphere with a diameter of 10 μm. If on the other hand MAA spheres are penetrable and 99mTc labelling can also occur on the inner side of the spheres, the amount of activity per sphere would be proportional to its radius to the third power. Accordingly, the greater the variation in size of 99mTc- labelled MAA, the less proportional the number of microspheres trapped in a region will be to flow.
Sphere number
Discrete tumours were induced by Anderson et al. in rats through subcapsular hepatic inoculations of HSN cells [63]. At 20 days, 12.5-, 25- or 40-μm diameter, radiolabelled albumin microspheres were administered, in various concentrations, via the gastroduodenal artery. Tumour to normal liver microsphere distribution ratios were determined and median values ranged from 0.1 (0.2 mg/ml 12.5-μm microspheres) to 1.8 (20 mg/ml 40-μm microspheres). Concentrated suspensions (20 mg/ml) of large microspheres (40 μm; ratio 1.8 versus 1.4 and 0.5 for 20 mg/ml of 25- and 12.5-μm microspheres, respectively) produced the most favourable tumour to normal liver distribution ratios. There were 2.7 × 106, 1.2 × 107 and 9.2 × 107 microspheres/ml in the 20 mg/ml suspensions of the 40, 25 and 12.5 μm diameter microspheres. With regard to the T/N ratios for small dilute microspheres, plasma skimming may have resulted in lower tumour uptake. On the other hand, a flow dislocation effect described previously for DSM may be responsible for the higher T/N ratios found with increasing number of microspheres injected. Following injection of 45–90 × 106 of 40-μm DSMs in a volume of 50 ml, flow dislocation from areas with high resting flow to areas with low resting flow was documented in liver tumours by Civalleri et al. [64, 65]. Thus, concentrated microspheres may lead to embolization following their injection which leads to distribution of the latter portion of microspheres to relatively hypovascular areas. Also, microsphere chain formation, a phenomenon first identified by Yipintsoi et al., may have contributed to the larger T/N ratios identified with increasing concentration of spheres injected [59]. Chain formation results from the impact and protrusion of microspheres into an arterial wall whose diameter is larger than the diameter of the microsphere with the impacted microsphere not significantly altering red blood cell flow in the vessel. Further microsphere-rich blood flows into the arterial vessel and these microspheres collect behind the impacted microsphere forming a chain resulting in an non-uniform distribution. As shown by Harell et al. chain formation is directly related to the number of microspheres injected [66]. Of interest, in this series, a weak yet significant inverse correlation was found between T/N ratios and tumour weight. Higher T/N ratios are associated with smaller tumours and larger tumours tend to become avascular in their core. As in the latter study carbonized particles were used (density 1.4 g/ml, major chemical components: 67 % of carbon and 25 % of oxygen); these findings warrant confirmation using resin and glass microspheres.
Density
In studies on myocardial blood flow, the use of radioactive (density 1.3 g/ml) or non-radioactive microspheres (density 1.02–1.05 g/ml) did not result in differences between endo/epicardial blood flow ratios suggesting that buoyancy does not significantly influence the in vivo behaviour of microspheres; average blood density is approximately 1.06 g/ml [67]. Furthermore, in a study by Reed and Wood, on the effect of body position on vertical distribution of pulmonary flow in dogs, no differences in distribution of microspheres were found between microspheres with densities of 0.2, 1.4 and 3.0 g/ml [68].
Modulation of microsphere uptake by liver metastases and of lung shunting
Various studies have shown that the amount of therapeutic microspheres targeting liver metastases may be improved by manipulating the tumour to normal liver blood flow.
Vasoactive drugs
As described previously, the vasculature of liver metastases is immature, possessing neither smooth muscle cells nor an adrenergic nerve supply and is therefore unable to respond to arterial constriction or dilation in the same way as normal vasculature [28, 29]. Accordingly, selective hepatic arterial injection of vasoconstricting agents, by causing a temporary arterial constriction in normal blood vessels, may enhance the delivery of arterially administered substances such as 90Y-labelled microspheres to liver metastases. Inversely, following hepatic arterial injection of vasodilating agents, a reduction of substance delivery to liver metastases may be anticipated. In this regard, Hafström et al. studied the effects of glucagon, histamine, vasopressin, adrenaline and noradrenaline on blood flow in anaesthetized rats with intrahepatic tumours using microspheres labelled with 99mTc and 51Cr [29]. Relative tumour blood flow was defined as the ratio between tumour flow and arterial hepatic flow. A relative decrease of tumour blood flow in relation to surrounding liver tissue blood flow was registered after infusion of vasopressin. No effects were seen after glucagon, histamine or adrenaline infusion. Contrariwise, in noradrenaline-infused rats an increase in tumour to liver ratio was found indicating a preferential blood flow to tumours induced by this drug. In sheep squamous cell carcinoma transplanted to the liver, intrahepatic arterial injection of angiotensin II produced a significant increase in the embolization rate of arterially introduced radioactive microspheres from 2.8 to 4.1 [69].
In a series of human hepatic cancer, using 81mKr, short duration hepatic intra-arterial injection of angiotensin II (3–4 min) resulted in a twofold increase in radioactivity in the tumour and a reduction to about one half of the baseline level in normal liver tissue [70]. Likewise, using angiotensin II, Hemingway et al. were able to increase the delivery of radiolabelled albumin microspheres in an experimental model of liver tumours as well as in patients suffering from colorectal cancer metastasized to the liver [71]. Using intraoperative laser Doppler flowmetry the latter authors assessed the impact of angiotensin II infusion on tumour blood flow in ten patients with colorectal liver metastases. Flow increased in eight of ten patients, but there were striking qualitative and quantitative differences in blood flow response between patients with isolated small metastases and those with large tumour deposits. In patients with small metastases, perfusion increased to a peak of up to ten times its baseline value over a period of 130–240 s from the start of angiotensin II infusion retuning to baseline over a similar period. The change in arterial pressure was parallelled with that of flow over time, although the flow changes proved to be several folds larger implying a significant reduction in tumour vasculature. In contrast, of the four patients with large tumours, two showed no blood flow response to angiotensin II infusion, whereas two showed a relatively low and short-lived peak which occurred only 30 s after the start of the angiotensin II infusion. Of interest, angiotensin II did not seem to impact baseline lung shunting in patients suffering from colorectal liver metastases suggesting a neoplastic nature of the blood vessels responsible for the shunt; percentages of lung shunting of 99mTc-labelled MAA ranging from 0.4 to 32 % have been reported in patients suffering from metastatic colorectal cancer (mCRC) [72]. Available data further suggest the degree of lung shunting is directly related to the size of the liver metastases and to their grade of vascularity [72]. Similar results were reported by Ho et al. [73].
Degradable starch microspheres
Starch microspheres have a mean diameter of 40 μm and consist of starch polymers cross-linked with epichlorohydrin. They are degraded by endogenous serum alpha-amylases and have a half-life in human serum of 25 min at 37 °C in vivo. In a hypovascular HSN liver tumour model, regional injection of 16.5 μm 57Co-microspheres resulted in a normal liver to tumour ratio of 2.25/1 for 99mTc-methylene diphosphonate (MDP) retention [74]. Concomitant injection of 40 μm DSM with 57Co-microspheres reversed this ratio to 1:2 corresponding to a fourfold increase in arterial blood flow, indicating that DSM selectively enhanced retention of 99mTc-MDP not by causing intra-tumour stasis but by directing a greater arterial flow to hypovascular areas. Similar findings were reported in patients using high flow dynamic CT scanning. Using 99mTc-MAA, Ziessman et al. sought to determine the optimal quantity of starch microspheres that would lead to a hold-up of a drug solution in the microcirculation of liver metastases in 20 patients suffering from mCRC [75]. The authors showed that the amount of lung shunting was related to the dose of starch microspheres injected; using a baseline hepatic arterial scintigraphy (500 μCi of 99mTc-MAA) as a reference and subsequent injections of 1.2 mCi/18 × 106 DSM per min with a maximum of five subsequent doses injected (total of 90 × 106 DSM injected), mean percentage lung shunting slightly decreased following the first injection of 18 × 106 DSM and progressively increased thereafter to 26.8 % after five doses of 18 × 106 DSM. While this phenomenon is as yet incompletely understood, various potential explanations for the increased arterial blood flow to liver tumours following DSM injection have been put forward: a DSM-induced arteriolar capillary blockade resulting in increased arterial backflow with blood flow redistribution, opening of arteriovenous shunts hitherto temporarily closed but opened following DSM embolization, a DSM-induced hypoxia-driven blood shunting or a reduction in the local washout of adenosine.
Temporary balloon occlusion
If the degree of lung shunting is too large (dose to the lungs exceeding 30 Gy), it may preclude patients from being treated. In this setting, temporary balloon occlusion using compliant or non-compliant balloons of the hepatic veins (right, middle or left hepatic vein depending upon the relevant drainage territory) may result in the reduction of pulmonary shunting to a level that permits SIRT with 90Y-labelled microspheres. Of interest, limited available data suggest that on repeated scans performed to evaluate a second treatment course, pulmonary shunting rests uninflated [76]. It is postulated that occlusion of the hepatic veins while infusing 90Y-microspheres results from the pressure placed on the vascular bed by the sedimentation of the microspheres during the implantation procedure which would endure beyond the immediacy of the implantation.
Implications of the rheology of labelled microspheres on the practice of SIRT and potential options for SIRT modulation
Following their intra-arterial injection, microspheres accumulate axially and show a disparate local flow as a result of size-dependent skimming; the concentration of microspheres entering a side branch will be lower than that in the main vessel. Both axial accumulation and skimming are believed to be largely due to the wall exclusion effect as described by Bayliss, not to inertial or gravitational forces. As a result of axial accumulation and skimming, large microspheres will be preferentially deposited in regions of high flow, whereas smaller microspheres will be preferentially diverted to regions of low flow. Flow to normal liver tissue is considerably variable between segments and also within one segment. As a consequence, at the microscopic level, in normal liver tissue, microspheres will be delivered heterogeneously within the microvasculature. Due to the broad range in size of radiolabelled 99mTc-MAA particles, ranging from 10 to 120 μm, it may be anticipated that the distribution heterogeneity within the normal microvasculature of 99mTc-MAA spheres will be more pronounced when compared to that of 90Y-SIR-spheres (20–60 μm) and 90Y-TheraSpheres (20–30 μm). Importantly, the non-uniformity in microsphere distribution in normal liver tissue in general has a significant “liver-sparing” effect on dose distribution [77]. The dosimetry for normal liver tissue was determined on autopsy material from a patient treated for a large hepatic liver metastasis with 90Y-SIR-spheres; two tissue samples of approximately 1 cm3 were prelevated, away from major blood vessels. In the normal liver sample, the average dose was 8.9 Gy with a minimum dose of 5 Gy. Less than 1 % of the normal tissue volume received a dose of 30 Gy, the level above which complications have resulted for whole liver exposure using external beam radiotherapy [78].
The fraction of arterial blood that flows to liver metastases differs between patients and also between different metastases of the same patient. Up to the size of 200 μm, metastases receive their blood supply via sinusoids. Beyond the size of 200 μm, peripheral neovascularization is induced. As lesions grow beyond the size of 1–1.5 cm, they outgrow their peripheral blood supply and the interior part of the metastases become largely devoid of arterial blood perfusion which may eventually result in central necrosis. In about 40 % of macrometastases, micrometastases are present in close proximity (1–1.5 cm), most likely resulting from local hepatic retrograde tumour spread. Accordingly, in decreasing order of magnitude, arterial flow to liver metastases is most pronounced in the hypervascular rim of metastases larger than 1.5 cm, followed by the smaller metastases and finally by the central hypoperfused region of the larger metastases. Arterioles feeding liver metastases in humans are on average 30–40 μm in diameter and none of the arterioles were shown to be larger than 100 μm in diameter. As such, on 99mTc-MAA scintigraphy, a proportion of spheres (the largest ones) are likely to be trapped outside, in front of the metastatic tissue. Furthermore, because of the wide variability in size of 99mTc-labelled MAA spheres and the potential size-related difference in specific activity (larger 99mTc-labelled MAA spheres are likely more active than smaller ones) and because of the skimming effect (larger spheres will follow the highest flow), existing differences in flow between metastatic lesions of variable size are likely to be exaggerated on 99mTc-MAA scintigraphy when compared to TheraSpheres and SIR-spheres (smaller variability in size and probably also in specific activity). Ideally, MAA kits would contain spheres within a size range similar to that of 90Y-SIR-spheres or 90Y-TheraSpheres. Furthermore, the optimal number of MAA particles to inject for the pretreatment planning scintigraphy warrants further exploration as it was shown that concentrated suspensions of microspheres produce more optimal tumour to normal liver distribution ratios; for a typical 99mTc-MAA pretreatment scintigraphy, on average 0.5 × 106 MAA spheres are injected versus >2 × 106 90Y-labelled microspheres. Of interest, available data suggest that the flow-based heterogeneous distribution of microspheres to metastatic lesions of variable size might be optimized, that is rendered more homogeneous, through the combined use of angiotensin II and DSM. In small liver metastases in humans, perfusion was shown to increase to a peak of up to ten times its baseline value over a period of 130–240 s from the start of angiotensin II infusion in the hepatic artery, returning to baseline over a similar period. In contrast, in large metastases, no blood flow or either a relatively low and short-lived peak response to angiotensin II infusion was found. The latter finding might explain why the isolated use of angiotensin II when using SIRT did not prove useful in human trials performed in the early 1990s. On the other hand, a number of studies have shown that injection of concentrated DSMs directs a greater arterial flow to hypovascular areas while at the same time increasing lung shunting (injection of more than 20 × 106 DSMs). Based on these data, a split-dose injection of 90Y-microspheres might be considered: the slow injection (over 1 min) of half a dose starting approximately 130 s after angiotensin II injection in the hepatic artery or the clinically relevant side branch thereof, followed by the injection of up to 40 × 106 DSM subsequently followed by injection of the second half a dose of 90Y-microspheres. The first half a dose, administered following angiotensin II injection, will target the hypervascular rim of larger lesions as well as significantly improve the perfusion of the smaller lesion (up to 10 times). The second half a dose, administered after DSM injection, will mainly target the hypovascular areas of the larger lesions. Adopting such a paradigm, temporary balloon occlusion of the draining hepatic vein(s) might be necessary whilst injecting DSMs and thereafter, in order to control the fraction of 90Y-microspheres shunted to the lungs. For direct comparative as well as for dosimetric purposes, evaluation of the lung shunt fraction and uptake by liver metastases of 99mTc-MAA adopting this paradigm should be evaluated using the same split-dose and ballooning approach. A potential drawback of the split-dose paradigm as suggested is a dose reduction to the hypervascular rim of the larger lesions which could theoretically compromise treatment outcome. On the other hand, adopting the currently used routine strategy for SIRT and considering the short range of the β emission of 90Y (mean tissue penetration of 2.5 mm, with a maximum penetration of 10 mm), the hypoxic, underperfused areas of larger metastases are now most likely undertreated. While the great majority of tumour cells suffer adverse consequences under hypoxic conditions, a small cell fraction is favoured through genomic changes and clonal selection [79, 80]. The aggressive phenotype of these tumour cells that can be considered as a desperate attempt of cancer cells to survive their hostile and nutrient-deprived microenvironment will lead to faster tumour progression that will further enhance hypoxia perpetuating a vicious circle and ultimately determining the fate of the patient. The split-dose paradigm as suggested will increase the deposit of 90Y-microspheres to hypoxic areas in metastases whilst at the same time provide oxygen to fix the radiation-induced damage to the more aggressive tumour cells induced by the β-rays emitted by 90Y. Future studies will need to resolve which one of both strategies, either conventional or split-dose, yields the best results in terms of treatment outcome.
References
Kasper HU, Drebber U, Dries V, Dienes HP. Liver metastases: incidence and histogenesis. Z Gastroenterol 2005;43(10):1149–57.
Wellner UF, Keck T, Brabletz T. Liver metastases: pathogenesis and oncogenesis. Chirurg 2010;81:551–6.
Kuvshinoff B, Fong Y. Surgical therapy of liver metastases. Semin Oncol 2007;34:177–85.
Hoffmann RT, Paprottka P, Jakobs TF, Trumm CG, Reiser MF. Arterial therapies of non-colorectal cancer metastases to the liver (from chemoembolization to radioembolization). Abdom Imaging 2011;36:671–6.
Malik U, Mohiuddin M. External-beam radiotherapy in the management of liver metastases. Semin Oncol 2002;29:196–201.
Van de Wiele C, Defreyne L, Peeters M, Lambert B. Yttrium-90 labelled resin microspheres for treatment of primary and secondary malignant liver tumors. Q J Nucl Med Mol Imaging 2009;53:317–24.
Memon K, Lewandowski RJ, Kulik L, Riaz A, Mulcahy MF, Salem R. Radioembolization for primary and metastatic liver cancer. Semin Radiat Oncol 2011;21:294–302.
Welsh JS, Kennedy AS, Thomadsen B. Selective internal radiation therapy (SIRT) for liver metastases secondary to colorectal adenocarcinoma. Int J Radiat Oncol Biol Phys 2006;66:S62–73.
Wong CY, Savin M, Sherpa KM, Qing F, Campbell J, Gates VL, et al. Regional yttrium-90 microsphere treatment of surgically unresectable and chemotherapy-refractory metastatic liver carcinoma. Cancer Biother Radiopharm 2006;21:305–13.
Salem R, Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Ibrahim S, et al. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol 2007;10:12–29.
Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Nemcek Jr AA, Kulik L, et al. Radioembolization with 90Y microspheres: angiographic and technical considerations. Cardiovasc Intervent Radiol 2007;30:571–92.
Chiesa C, Maccauro M, Romito R, Spreafico C, Pellizzari S, Negri A, et al. Need, feasibility and convenience of dosimetric treatment planning in liver selective internal radiation therapy with (90)Y microspheres: the experience of the National Tumor Institute of Milan. Q J Nucl Med Mol Imaging 2011;55:168–97.
Kao YH, Hock Tan AE, Burgmans MC, Irani FG, Khoo LS, Gong Lo RH, et al. Image-guided personalized predictive dosimetry by artery-specific SPECT/CT partition modeling for safe and effective 90Y radioembolization. J Nucl Med 2012;53:559–66.
Garin E, Lenoir L, Rolland Y, Edeline J, Mesbah H, Laffont S, et al. Dosimetry based on 99mTc-macroaggregated albumin SPECT/CT accurately predicts tumor response and survival in hepatocellular carcinoma patients treated with 90Y-loaded glass microspheres: preliminary results. J Nucl Med 2012;53:255–63.
Lautt WW. Role and control of the hepatic artery. In: Lautt WW, editor. Hepatic circulation in health and disease. New York: Raven; 1981. p. 203–26.
Vollmar B, Menger MD. The hepatic microcirculation: mechanistic contributions and therapeutic targets in liver injury and repair. Physiol Rev 2009;89:1269–339.
Rappaport AM. Hepatic blood flow: morphologic aspects and physiologic regulation. Int Rev Physiol 1980;21:1–63.
Greenway CV, Stark RD. Hepatic vascular bed. Physiol Rev 1971;51:23–65.
Eipel C, Abshagen K, Vollmar B. Regulation of hepatic blood flow: the hepatic arterial buffer response revisited. World J Gastroenterol 2010;16:6046–57.
Taniguchi H, Oguro A, Takeuchi K, Miyata K, Takahashi T, Inaba T, et al. Difference in regional hepatic blood flow in liver segments—non-invasive measurement of regional hepatic arterial and portal blood flow in human by positron emission tomography with H2(15)O. Ann Nucl Med 1993;7:141–5.
Oda M, Yokomori H, Han JY. Regulatory mechanisms of hepatic microcirculatory hemodynamics: hepatic arterial system. Clin Hemorheol Microcirc 2006;34:11–26.
Pannen BH. New insights into the regulation of hepatic blood flow after ischemia and reperfusion. Anesth Analg 2002;94:1448–57.
Ueno T, Bioulac-Sage P, Balabaud C, Rosenbaum J. Innervation of the sinusoidal wall: regulation of the sinusoidal diameter. Anat Rec A Discov Mol Cell Evol Biol 2004;280:868–73.
Ezzat WR, Lautt WW. Hepatic arterial pressure-flow autoregulation is adenosine mediated. Am J Physiol 1987;252:H836–45.
Lautt WW. The 1995 Ciba-Geigy Award Lecture. Intrinsic regulation of hepatic blood flow. Can J Physiol Pharmacol 1996;74:223–33.
Lautt WW. Hepatic vasculature: a conceptual review. Gastroenterology 1977;73:1163–9.
Krylova NV. Characteristics of microcirculation in experimental tumours. Bibl Anat 1969;10:301–3.
Mattsson J, Appelgren L, Hamberger B, Peterson HI. Adrenergic innervation of tumour blood vessels. Cancer Lett 1977;3:347–51.
Hafström L, Nobin A, Persson B, Sundqvist K. Effects of catecholamines on cardiovascular response and blood flow distribution to normal tissue and liver tumors in rats. Cancer Res 1980;40:481–5.
Wickersham JK, Barrett WP, Furukawa SB, Puffer HW, Warner NE. An evaluation of the response of the microvasculature in tumors in C3H mice to vasoactive drugs. Bibl Anat 1977;(15 Pt 1):291–3.
Cuenod C, Leconte I, Siauve N, Resten A, Dromain C, Poulet B, et al. Early changes in liver perfusion caused by occult metastases in rats: detection with quantitative CT. Radiology 2001;218:556–61.
Hemingway DM, Cooke TG, Grime SJ, Nott DM, Jenkins SA. Changes in hepatic haemodynamics and hepatic perfusion index during the growth and development of hypovascular HSN sarcoma in rats. Br J Surg 1991;78:326–30.
Fukumura D, Yuan F, Monsky WL, Chen Y, Jain RK. Effect of host microenvironment on the microcirculation of human colon adenocarcinoma. Am J Pathol 1997;151:679–88.
Kruskal JB, Thomas P, Kane RA, Goldberg SN. Hepatic perfusion changes in mice livers with developing colorectal cancer metastases. Radiology 2004;231:482–90.
Carter R, Anderson JH, Cooke TG, Baxter JN, Angerson WJ. Splanchnic blood flow changes in the presence of hepatic tumour: evidence of a humoral mediator. Br J Cancer 1994;69:1025–6.
Sjövall S, Ahrén B, Bengmark S. Intermittent hepatic arterial or portal occlusion reduces liver tumor growth. J Surg Res 1991;50:146–9.
Kan Z, Ivancev K, Lunderquist A, McCuskey PA, Wright KC, Wallace S, et al. In vivo microscopy of hepatic tumors in animal models: a dynamic investigation of blood supply to hepatic metastases. Radiology 1993;187:621–62.
Archer SG, Gray BN. Vascularization of small liver metastases. Br J Surg 1989;76:545–8.
Haugeberg G, Strohmeyer T, Lierse W, Böcker W. The vascularization of liver metastases. Histological investigation of gelatine-injected liver specimens with special regard to the vascularization of micrometastases. J Cancer Res Clin Oncol 1988;114:415–9.
Lin G, Lunderquist A, Hägerstrand I, Boijsen E. Postmortem examination of the blood supply and vascular pattern of small liver metastases in man. Surgery 1984;96:517–26.
Taylor I, Bennett R, Sherriff S. The blood supply of colorectal liver metastases. Br J Cancer 1978;38:749–56.
Paris AL, Meissner WA, McDermott Jr WV. Histologic changes seen in the hepatic parenchyma and in metastatic nodules following hepatic dearterialization. J Surg Oncol 1982;19:114–8.
Oktar SO, Yücel C, Demirogullari T, Uner A, Benekli M, Erbas G, et al. Doppler sonographic evaluation of hemodynamic changes in colorectal liver metastases relative to liver size. J Ultrasound Med 2006;25:575–82.
Shuman WP. Liver metastases from colorectal carcinoma: detection with Doppler US-guided measurements of liver blood flow—past, present, future. Radiology 1995;195:9–10.
Miles KA, Leggett DA, Kelley BB, Hayball MP, Sinnatamby R, Bunce I. In vivo assessment of neovascularization of liver metastases using perfusion CT. Br J Radiol 1998;71:276–81.
Flowerdew ADS, McLaren MI, Fleming JS, Britten AJ, Ackery DM, Birch SJ, et al. Liver tumour blood flow and responses to arterial embolization measured by dynamic hepatic scintigraphy. Br J Cancer 1987;55:269–73.
Ueda H, Lio M, Kaihara S. Determination of regional pulmonary blood flow in various cardiopulmonary disorders. Study and application of macroaggregated albumin (MAA) labelled with I-131 (I). Jpn Heart J 1964;190:431–44.
Taplin GV, Johnson DE, Dore EK, Kaplan HS. Suspensions of radioalbumin aggregates for photoscanning the liver, spleen, lung and other organs. J Nucl Med 1964;5:259–75.
Chandra R, Shamoun J, Braunstein P, DuHov OL. Clinical evaluation of an instant kit for preparation of 99mTc-MAA for lung scanning. J Nucl Med 1973;14:702–5.
Zamora PO, Rhodes BA. Imidazoles as well as thiolates in proteins bind technetium-99m. Bioconjug Chem 1992;3:493–8.
Rudolph AM, Heymann MA. The circulation of the fetus in utero. Methods for studying distribution of blood flow, cardiac output and organ blood flow. Circ Res 1967;21:163–84.
McDevitt DG, Nies AS. Simultaneous measurement of cardiac output and its distribution with microspheres in the rat. Cardiovasc Res 1976;10:494–8.
Fähraeus R. Die Strömungsverhältnisse und die Verteilung der Blutzellen im Gefäßsystem. Klin Wochenschr 1928;7:100–6.
Segré G, Silberberg A. Radial particle displacements in Poiseuille flow of suspensions. Nature 1961;189:209–10.
Segré G, Silberberg A. Behaviour of macroscopic rigid spheres in Poiseuille flow. Parts 1 and 2. J Fluid Mech 1962;14:115–57.
Fung Y. Stochastic flow in capillary blood vessels. Microvasc Res 1973;5:34–48.
Bayliss LE. The axial drift of the red cells when blood flows in a narrow tube. J Physiol 1959;149:593–613.
Ofjord ES, Clausen G, Aukland K. Skimming of microspheres in vitro: implications for measurement of intrarenal blood flow. Am J Physiol 1981;241:H342–7.
Yipintsoi T, Dobbs Jr WA, Scanlon PD, Knopp TJ, Bassingthwaighte JB. Regional distribution of diffusible tracers and carbonized microspheres in the left ventricle of isolated dog hearts. Circ Res 1973;33:573–87.
Domenech RJ, Hoffman JI, Noble MI, Saunders KB, Henson JR, Subijanto S. Total and regional coronary blood flow measured by radioactive microspheres in conscious and anesthetized dogs. Circ Res 1969;25:581–96.
Katz MA, Blantz RC, Rector FC, Seldin DW. Measurement of intrarenal blood flow. I. Analysis of microsphere method. Am J Physiol 1971;220:1903–13.
Meade VM, Burton MA, Gray BN, Self GW. Distribution of different sized microspheres in experimental hepatic tumours. Eur J Cancer Clin Oncol 1987;23:37–41.
Anderson JH, Angerson WJ, Willmott N, Kerr DJ, McArdle CS, Cooke TG. Regional delivery of microspheres to liver metastases: the effects of particle size and concentration on intrahepatic distribution. Br J Cancer 1991;64:1031–4.
Civalleri D, Rollandi G, Simoni G, Mallarini G, Repetto M, Bonalumi U. Redistribution of arterial blood flow in metastases-bearing livers after infusion of degradable starch microspheres. Acta Chir Scand 1985;151:613–7.
Civalleri D, Scopinaro G, Simoni G, Claudiani F, Repetto M, DeCian F, et al. Starch microsphere-induced arterial flow redistribution after occlusion of replaced hepatic arteries in patients with liver metastases. Cancer 1986;58:2151–5.
Harell GS, Corbet AB, Dickhoner WH, Bradley BR. The intraluminal distribution of 15-micrometer-diameter carbonized microspheres within arterial microvessels as determined by vital microscopy of the golden hamster cheek pouch. Microvasc Res 1979;18:384–402.
da-Luz PL, Leite JJ, Barros LF, Dias-Neto A, Zanarco EL, Pileggi FJ. Experimental myocardial infarction: effect of methylprednisolone on myocardial blood flow after reperfusion. Braz J Med Biol Res 1982;15:355–60.
Reed Jr JH, Wood EH. Effect of body position on vertical distribution of pulmonary blood flow. J Appl Physiol 1970;28:303–11.
Burton M, Gray B, Coletti A. Effect of angiotensin II on blood flow in the transplanted sheep squamous cell carcinoma. Eur J Cancer Clin Oncol 1988;24:1373–6.
Sasaki Y, Imaoka S, Hasegawa Y, Nakano S, Ishikawa O, Ohigashi H, et al. Changes in distribution of hepatic blood flow induced by intra-arterial infusion of angiotensin II in human hepatic cancer. Cancer 1985;55:311–6.
Hemingway DM, Angerson WJ, Anderson JH, Goldberg JA, McArdle CS, Cooke TG. Monitoring blood flow to colorectal liver metastases using laser Doppler flowmetry: the effect of angiotensin II. Br J Cancer 1992;66:958–60.
Goldberg JA, Bradnam MS, Kerr DJ, Haughton DM, McKillop JH, Bessent RG, et al. Arteriovenous shunting of microspheres in patients with colorectal liver metastases: errors in assessment due to free pertechnetate, and the effect of angiotensin II. Nucl Med Commun 1987;8:1033–46.
Ho S, Lau WY, Leung WT, Chan M, Chan KW, Johnson PJ, et al. Arteriovenous shunts in patients with hepatic tumors. J Nucl Med 1997;38:1201–5.
Chang D, Jenkins SA, Grime SJ, Nott DM, Cooke T. Increasing hepatic arterial flow to hypovascular hepatic tumors using degradable starch microspheres. Br J Cancer 1996;73:961–5.
Ziessman HA, Thrall JH, Gyves W, Ensminger WD, Niederhuber JE, Tuscan M, et al. Quantitative hepatic arterial perfusion scintigraphy and starch microspheres in cancer chemotherapy. J Nucl Med 1983;24:871–5.
Bester L, Salem R. Reduction of arteriohepatovenous shunting by temporary balloon occlusion in patients undergoing radioembolization. J Vasc Interv Radiol 2007;18:1310–4.
Roberson PL, Ten Haken RK, McShan DL, McKeever PE, Ensminger WD. Three-dimensional tumor dosimetry for hepatic yttrium-90-microsphere therapy. J Nucl Med 1992;33:735–8.
Campbell AM, Bailey IH, Burton MA. Tumour dosimetry in human liver following hepatic yttrium-90 microsphere therapy. Phys Med Biol 2001;46:487–98.
Vaupel P. Hypoxia and aggressive tumor phenotype: implications for therapy and prognosis. Oncologist 2008;13:21–6.
Kunz M, Ibrahim S. Molecular responses to hypoxia in tumor cells. Mol Cancer 2003;2:23.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van de Wiele, C., Maes, A., Brugman, E. et al. SIRT of liver metastases: physiological and pathophysiological considerations. Eur J Nucl Med Mol Imaging 39, 1646–1655 (2012). https://doi.org/10.1007/s00259-012-2189-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2189-6