Abstract
Purpose
Several diagnostic trials have indicated that the combined use of 18F-fluoroethyl-l-tyrosine (FET) PET and MRI may be superior to MRI alone in selecting the biopsy site for the diagnosis of gliomas. We estimated the cost-effectiveness of the use of amino acid PET compared to MRI alone from the perspective of the German statutory health insurance.
Methods
To evaluate the incremental cost-effectiveness of the use of amino acid PET, a decision tree model was built. The effectiveness of FET PET was determined by the probability of a correct diagnosis. Costs were estimated for a baseline scenario and for a more expensive scenario in which disease severity was considered. The robustness of the results was tested using deterministic and probabilistic sensitivity analyses.
Results
The combined use of PET and MRI resulted in an increase of 18.5% in the likelihood of a correct diagnosis. The incremental cost-effectiveness ratio for one additional correct diagnosis using FET PET was €6,405 for the baseline scenario and €9,114 for the scenario based on higher disease severity. The probabilistic sensitivity analysis confirmed the robustness of the results.
Conclusion
The model indicates that the use of amino acid PET may be cost-effective in patients with glioma. As a result of several limitations in the data used for the model, further studies are needed to confirm the results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gliomas are primary brain tumours and are among the tumours with the worst prognosis. The treatment and the prognosis of gliomas are predominantly determined by histological grading. While low-grade gliomas may permit a watch and wait strategy [1], high-grade gliomas require aggressive treatment with surgical resection, radiation and chemotherapy [2–4]. In order to consider the appropriate treatment options, it is important to achieve an early and valid diagnosis. For the diagnosis of gliomas, guidelines recommend a histological diagnosis via brain biopsy in brain tumours [5–7]. When performing a brain biopsy, it is important to choose the target region which is most informative for a correct diagnosis. Brain biopsies are fatal in about 0.2% of patients and lead to severe morbidity in up to 2% [8, 9].
Due to its outstanding soft-tissue contrast and the vast opportunities of multiplanar reconstruction, MRI has become a standard tool in the diagnosis of gliomas [10, 11]. However, MRI has limited ability to differentiate tumour tissue from oedematous, necrotic or fibrotic tissue. This can lead to discrepancies between the real tumour size and signal abnormalities in MRI [12], resulting in selection of a wrong biopsy site [13].
PET is one of the most promising new diagnostic tools in clinical oncology because it permits the visualization of the tumour metabolism. In contrast to most other oncological indications, the diagnosis of gliomas is dominated by the use of amino acid PET tracers [12, 14]. Several studies have shown that the use of amino acid PET enables clinicians to select tumour tissue more accurately than with MRI [13, 15–20]. The current guidelines of the Neuroimaging Committee of the European Association of Nuclear Medicine as well as the guidelines of the German Society for Nuclear Medicine recommend the use of amino acid PET, including 18F-fluoroethyl-l-tyrosine (FET) PET for selecting the best biopsy site in gliomas [21, 22].
However, the use of amino acid PET remains a matter of debate, since high-quality randomized controlled trials are lacking. So far, there is no controlled study that allows a statement as to the patient-related benefits such as an increase in quality of life or an increase in survival. Therefore, in spite of the above-mentioned recommendations, the reimbursement for FET PET is still controversial, especially within the German health-care system. Presently, the use of FET PET is not reimbursed for the imaging of gliomas. To our knowledge, an economic analysis on the selection of the biopsy site in gliomas has not yet been published.
We report here an analysis of the cost-effectiveness of FET PET for selecting the best biopsy site in gliomas from the perspective of the statutory health insurance in Germany. We developed a decision tree model to analyse the effectiveness for this indication. By this means we compared the two alternatives, MRI alone (MRI) and the combined use of MRI and FET PET (MRI plus PET). The cost-effectiveness was calculated using the incremental cost-effectiveness ratio (ICER).
Methods
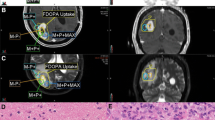
In order to analyse the effectiveness of MRI combined with FET PET when guiding the biopsy of gliomas, we built a decision tree model in which two alternative strategies were compared (Fig. 1). In the intervention group the biopsy of gliomas was guided by MRI plus PET, and in the control group the biopsy was guided by MRI alone.
Decision tree for modelling the effectiveness of FET PET in biopsy planning of patients with glioma. The model includes the two alternative strategies of the use of MRI alone (Biopsy based on MRI) to guide the biopsy of the glioma and of the combined use of MRI and PET (Additional PET). The probability of the right diagnosis is defined as the outcome (see text for more details) (green circles chance node, red triangles termination node)
The construction of the decision tree model and the sensitivity analyses were performed using TreeAge Pro 2009 (TreeAge Software, Williamstown, MA).
Calculation of the costs
We calculated the costs using a method similar to that used by Heinzel et al. [23], who provide a more detailed description. The costs of amino acid PET were obtained from the reimbursement scheme for medical procedures for privately insured patients (http://www.e-bis.de/goae/defaultFrame.htm) because they are currently not covered by the German statutory health insurance. We calculated a baseline scenario with the lowest reimbursement amount and a severity-adjusted scenario with a higher reimbursement. The latter scenario was calculated using a severity-based multiplying factor depending on the medical procedure according to the above-mentioned cost scale. This severity adjustment in calculating reimbursement for medical procedures allows adjustment for various factors such as the difficulty of the procedure or the qualification of the health personnel.
We included the following costs for the baseline scenario (severity-adjusted scenario): detailed consultation €8.74 (€20.10), report on diagnostic findings €7.58 (€17.43), intravenous injection €4.08 (€9.38), whole-body tumour scintigraphy €131.15 (€236.07), PET with quantitative analysis €417.15 (€786.89). These categories refer to the codes 3, 75, 253, 5431 and 5489 of the above-mentioned cost scale. Additionally, the costs for the radioactive tracer were taken into account. Some hospitals using amino acid PET have the capacity to produce the tracers on-site. Moreover, FET is available via commercial enterprises. In order to represent the range of costs, we calculated the mean of the price of two German enterprises and one on-site facility. Adding value-added tax of 19%, the cost for the tracer was €616.
We did not consider indirect costs because they are not relevant from the perspective of the health insurance.
The cost of the baseline scenario together with the additional tracer was €1,185, and the cost of the morbidity-adjusted reimbursement rate scenario was €1,686 for one PET scan.
Calculation of effectiveness of FET PET-guided biopsy of gliomas
Input data
Our analysis of the use of amino acid PET for biopsy guidance in patients with glioma was based on the longitudinal within-group comparison of Pauleit et al. [19] including 31 patients. In contrast to other studies, two important methodological features were considered in this analysis. First, it was the only analysis that compared MRI alone with the combined information from MRI and PET for the selection of the biopsy site. Second, in order to assess the diagnostic quality of amino acid PET the results of the biopsy should be related to its exact location within the PET scan. In case of brain biopsies, however, it is difficult for the neurosurgeon to verify the exact location of the biopsy in relation to a postoperative cavity. In the study of Pauleit et al. [19] the neurosurgeon placed intraoperative markers (e.g. titanium pellets) at the location from which the biopsy was taken. By means of these markers, it was possible to correlate exactly the imaging findings with the histological specimen.
Decision tree model
The decision tree model begins at the point where the diagnosis of a glioma is considered likely resulting in a confirmatory test with a biopsy. The diagnostic hypothesis is based on an MRI scan acquiring a T1-weighted 3-D image with and without contrast agent (Gd-DTPA) and a transverse FLAIR sequence. The outcome was defined as the correctness of the diagnosis (correct diagnosis = 1, wrong diagnosis = 0).
For the upper branch the first chance node contains the two likelihoods PET-positive and PET-negative. This describes the likelihood that the PET scan shows focally increased amino acid metabolism resulting in the suspicion of a PET-positive glioma. If the PET scan is positive, then the combined information from MRI plus PET is used to identify a target region for biopsy. The chance node following the PET-positive branch includes the likelihood that a target region based on the combined information from MRI plus PET will or will not result in identifying tumour tissue in a biopsy. Since gliomas are known to have a heterogeneous structure a biopsy should be taken at the most dedifferentiated part of the tumour, otherwise the biopsy will lead to a wrong diagnosis. Thus, if the biopsy specimen correctly indicates both the type of tumour (i.e. glioma) and the grade of the tumour (i.e. the degree of dedifferentiation, WHO I, II, III or IV) it is termed ‘Correct Diagnosis’, and if not ‘Incorrect Diagnosis’. The probabilities are calculated based on the comparison of the biopsy specimen and the final diagnosis obtained after surgical resection of the tumour. Of 23 positive biopsy specimens, 21 showed the correct grading, resulting in a probability of 0.91 for correct grading.
The branches following the chance node ‘No Tumour in Biopsy’ illustrate the likelihoods of glioma in spite of negative results from the biopsy. The branch ‘No Tumour in Biopsy’ includes the probabilities that a negative biopsy, given a positive PET and MRI scan, corresponds to the complete absence of tumour (Correct Diagnosis) or to a tumour in another region of the brain (Incorrect Diagnosis). Comparing the negative biopsies from regions defined by PET and MRI with the final diagnoses showed discrepant diagnoses in four of five patients. Thus, in 20% of patients a negative biopsy specimen correctly predicted the absence of tumour.
The lower part of the decision tree models the use of MRI alone for identifying a target region for biopsy. Basically, it has the same structure as the upper part. The likelihood of negative or positive MRI is not included since the decision tree starts with the presumption of a diagnosis of glioma based on MRI (i.e. positive MRI).
The probabilities of the chance nodes (i.e. ‘Additional PET’, ‘PET negative’, ‘Tumour in Biopsy’, and ‘No Tumour in Biopsy’) are based on the study by Pauleit et al. [19]. For the calculations, we defined the prevalence (i.e. the number of positive biopsies in the sample divided by the number of all biopsies in the sample), the sensitivity (i.e. the number of true positive biopsy targets in MRI plus PET divided by the number of all positive biopsy targets), the specificity (i.e. the number of true-negative biopsy targets in MRI plus PET divided by the number of all negative biopsy targets), and the positive predictive value (i.e. the number of biopsy targets identified by PET and MRI correctly predicting tumour in the biopsy specimen divided by all biopsy targets identified by MRI plus PET).
In the upper branch, the positive predictive value (i.e. the likelihood of the chance node following the branch ‘PET positive’) was estimated to be 93%. Thus, if a target region for biopsy is defined by using MRI plus PET there is a probability of 0.93 for acquiring tumour tissue in the biopsy specimen.
The first chance node of the lower part of the decision tree is calculated analogously to the chance node of the alternative ‘Additional PET’ (see above). Applying the reported data from Pauleit et al. [19] (sensitivity 96%, specificity 53% and prevalence 50%) we calculated a positive predictive value (PPV) of 67%.
The branch ‘No Tumour in Biopsy’ is the likelihood that a negative biopsy, given a positive MRI scan, corresponds to the complete absence of tumour (‘Correct Diagnosis’) or to the presence of tumour in another region of the brain (‘Incorrect Diagnosis’). Because there were no data available from a control group without the use of a PET scan, we included the negative biopsies from areas selected by MRI alone and from those selected by MRI plus PET. The rationale for this was the assumption that in the absence of a PET scan selected regions may or may not lie within areas of increased amino acid metabolism. Thus, all negative biopsies taken from MRI-positive regions are considered irrespective of whether they are or are not additionally positive in the PET scan. Of the 26 negative biopsy specimens, 8 showed an absence of tumour in the final diagnosis, resulting in a probability of 0.30 for a correct diagnosis.
The probability of a ‘Correct Diagnosis’ following the branch ‘Tumour in Biopsy’ was determined by comparing the results of the final diagnosis (i.e. after surgical resection of the tumour) with those from the biopsies. Again, we included the negative biopsies from areas selected by MRI alone and from those selected by MRI plus PET. Of 26 positive biopsy specimens, 23 had the correct grading, resulting in a probability of 0.88 for a correct grading.
The probabilities of a correct diagnosis using MRI alone and using MRI plus PET were calculated with the roll-back procedure for decision trees using TreeAge Pro 2009. To estimate expected values for each decision node, this method starts at the end-points of the decision tree and multiplies the pay-offs (i.e. the benefit to the patient) by the probabilities of their occurrence. For example, the expected value for the third decision node of the alternative ‘Additional PET’ following the branch ‘Tumour in Biopsy’ is calculated as: 1 × 0.91 + 0 × 0.09 = 0.91. These calculations are made for each decision node.
Sensitivity analyses
In order to test the robustness of the results, we performed deterministic and probabilistic sensitivity analyses. Deterministic one-way sensitivity analyses were performed for all values of the decision tree models to account for the impact of their uncertainty. For each variable three intervals were chosen. The low and high values of the intervals were determined by questioning an expert. The expert was asked to define a plausible range which would contain 95% of the values for each variable (see Table 1).
We also performed probabilistic sensitivity analyses using Monte Carlo simulation [24]. For the attribution of probability distributions to the variables of the decision tree, triangular distributions were used [25, 26]. Based on the initial definition of the intervals by the expert, we fitted the respective distributions for all variables (see Table 1). Afterwards the expert was questioned again in order to ensure the plausibility of the distributions. Based on these distributions, we performed a second-order Monte Carlo simulation with 10,000 samples.
Results
Base case
The decision tree showed that the combined use of MRI plus PET would result in an increased likelihood of a correct diagnosis when compared to MRI alone (p = 0.874 versus p = 0.689). Therefore, the incremental effectiveness of the combined use of PET and MRI compared to MRI alone is an increase of 18.5% in the likelihood of a correct diagnosis. This means that six patients have to be diagnosed with MRI plus PET in order to avoid one wrong diagnosis (number needed to diagnose = 1/0.185 = 5.4).
For the baseline scenario, this results in an ICER of 1,185/0.185 = €6,405 (morbidity-adjusted reimbursement rate scenario = €9,114).
Sensitivity analyses
The results of the one-way sensitivity analyses are shown in Table 2. The variation in node 6 (the first node of the lower branch in Fig. 1) may result in the lowest incremental effectiveness of the combined use of MRI plus PET versus MRI alone.
The statistics of the Monte Carlo simulations addressing the effectiveness of MRI plus PET-guided biopsy in gliomas are shown in Table 3 and Fig. 2. The mean incremental effectiveness of MRI plus PET-guided biopsy versus biopsy without PET was 0.179. Within the interval of 95% the values ranged from 0.084 to 0.274, i.e. the probability of a correct diagnosis using MRI plus PET is increased between 8% and 27%. This would result in an ICR between €14,813 and €4,389 for the baseline reimbursement rate, and between €21,075 and €6,244 for the morbidity-adjusted reimbursement rate.
Discussion
This study evaluated the cost-effectiveness of MRI plus PET for the target selection of biopsies in gliomas. Compared to MRI alone, MRI plus PET led to an increased likelihood of a correct diagnosis with an incremental effectiveness of 18.5% and additional costs ranging from €1,185 to €1,686. The ICER for one additional correct diagnosis using MRI plus PET was between €6,405 and €9,114. The probabilistic sensitivity analysis confirmed the robustness of the results.
Because there are no empirical data on patient-related benefits such as survival or changes in patient management, in this model we defined the probability of a correct diagnosis as the primary outcome. Although there was no direct benefit for the patient, the probability of a correct diagnosis appears to be an appropriate surrogate, as further therapy planning in patients with glioma is based on it. Because patients with high-grade glioma require radical surgical resection of the tumour followed by chemotherapy and radiation [7, 27], a wrong diagnosis may lead either to premature aggressive treatment with the risk of serious side effects or to delayed treatment with the risk of a decrease in survival time.
Based on the results of this analysis, the increase in costs for MRI plus PET lay between €1,185 for the baseline scenario and €1,686 for the morbidity-adjusted reimbursement rate scenario. Considering the costs of treatment for gliomas (including many false-positives), this increase in diagnostic cost appears to be acceptable. For example, in a recently published systematic review that evaluated the treatment costs of chemotherapy using temozolomide combined with radiotherapy, the treatment costs for newly diagnosed glioblastoma were between €27,365 and €39,092 [28]. When using MRI plus PET, in our analysis six patients needed to be diagnosed to obtain one additional correct diagnosis. Hence, considerable savings can be expected by avoiding unnecessary treatment.
It has been shown that the use of amino acid PET is of particular value in patients with a non-contrast-enhancing brain tumour on the MRI scan [29]. In these patients biopsy targeting without PET is particularly difficult because usually the area of maximum contrast enhancement is selected as the target. Additionally, it is important to note that non-enhancement of a brain lesion does not equate to low-grade malignancy [30]. Therefore, a biopsy-based diagnosis is important in order to choose the most appropriate treatment. The data underlying our analysis were not selected according to contrast enhancement on the MRI scan. Therefore, one may assume an even lower likelihood of a correct diagnosis with MRI alone compared to our input data. Thus, the most cost-effective use of amino acid PET may apply to such cases. Other reasons such as the heterogenic structure of the tumour tissue, may also complicate biopsy targeting with MRI alone. Thus, restricting the use of amino acid PET to lesions without contrast enhancement may not be justified.
Some limitations of this analysis have to be considered. First, clinical data could only be derived from a longitudinal within-group comparison including 31 patients. In that study, patients with a space-occupying intracerebral lesion that appeared as highly suspicious for cerebral glioma on the CT and MRI scans were consecutively included. As indicated by the one-way sensitivity analyses, among different variations of the parameters of the decision tree model, the variation of the probability of a positive biopsy diagnosis using MRI alone had the strongest impact on outcome. Second, in the decision tree model the branch ‘No Tumour in Biopsy’ represents the likelihood that a negative biopsy (assuming a positive PET and MRI scan) corresponds to complete absence of tumour tissue (Correct Diagnosis) or to the presence of tumour in another region of the brain (Incorrect Diagnosis). This chance node indicates the probability that in only 20% of the negative biopsies would the specimen correctly predict the absence of tumour. It has to be considered that this is related only to regions where a PET scan indicates the presence of tumour tissue. In such cases it seems that a negative biopsy would be unreliable.
In the near future, additional studies are needed to directly compare MRI-based and MRI/PET-based selection of the biopsy site, ideally performed as randomized controlled trials. This may also permit the reliability of a negative biopsy in a patient with a PET scan indicating tumour tissue to be verified. However, it has to be noted that such a trial would require withholding a PET scan from some patients. Because of an increased risk of a wrong diagnosis, one may argue that withholding an amino acid PET scan would be inappropriate from an ethical point of view since it violates the duty of the physician to provide optimal medical management (see, for example, references [31, 32] for a more detailed discussion on the ethical aspects of controlled trials).
Additionally, it has to be considered that the technical requirements for biopsy targeting using FET PET are high. It can only be done with close interdisciplinary cooperation between the department of radiology/nuclear medicine and the department of neurosurgery and the availability of a specific navigation system permitting fusion of the FET PET and MRI data. These requirements may only be fulfilled in some specialized centres treating a high number of patients with glioma. One may therefore consider that biopsies in patients with glioma should be performed exclusively in such specialized centres.
Third, it has to be noted that the costs of the tracers were only calculated approximately based on data from two German enterprises. The representativeness of this estimate is unclear since costs may vary from centre to centre and additional variables may affect the real costs. These are, for example, reduced costs due to sales discounts if more than one unit is purchased or additional costs due to long distance transportation. Moreover, an increasing demand may prospectively lead to an increase in production capacity and to a decrease in price. These factors depend on the individual needs of an institution and the future developments of the use of amino acid PET.
Summing up, the model indicates that FET PET may be a cost-effective tool in the planning of biopsies of gliomas. It has the potential to reduce ineffective treatment and corresponding costs as well as harm to the patient. However, additional studies are needed to confirm the results.
References
Floeth FW, Pauleit D, Sabel M, Stoffels G, Reifenberger G, Riemenschneider MJ, et al. Prognostic value of O-(2-18F-fluoroethyl)-L-tyrosine PET and MRI in low-grade glioma. J Nucl Med. 2007;48(4):519–27.
Deb P, Sharma MC, Mahapatra AK, Agarwal D, Sarkar C. Glioblastoma multiforme with long term survival. Neurol India. 2005;53(3):329–32.
Walid MS, Smisson III HF, Robinson Jr JS. Long-term survival after glioblastoma multiforme. South Med J. 2008;101(9):971–2.
Scoccianti S, Magrini SM, Ricardi U, Detti B, Buglione M, Sotti G, et al. Patterns of care and survival in a retrospective analysis of 1059 patients with glioblastoma multiforme treated between 2002 and 2007: a multicenter study by the Central Nervous System Study Group of Airo (Italian Association of Radiation Oncology). Neurosurgery. 2010;67(2):446–58.
Grant R. Overview: brain tumour diagnosis and management/Royal College of Physicians guidelines. J Neurol Neurosurg Psychiatry. 2004;75 Suppl 2:ii18–23.
Schneider T, Mawrin C, Scherlach C, Skalej M, Firsching R. Gliomas in adults. Dtsch Arztebl Int. 2010;107(45):799–808.
Stupp R, Roila F. Malignant glioma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2008;19 Suppl 2:ii83–5.
Kaufman HH, Catalano Jr LW. Diagnostic brain biopsy: a series of 50 cases and a review. Neurosurgery. 1979;4(2):129–36.
Sawyer J, Ellner J, Ransohoff DF. To biopsy or not to biopsy in suspected herpes simplex encephalitis: a quantitative analysis. Med Decis Mak. 1988;8(2):95–101.
DeAngelis LM. Brain tumors. N Engl J Med. 2001;344(2):114–23.
Chen W. Clinical applications of PET in brain tumors. J Nucl Med. 2007;48(9):1468–81.
Langen KJ, Hamacher K, Weckesser M, Floeth F, Stoffels G, Bauer D, et al. O-(2-[18F]fluoroethyl)-L-tyrosine: uptake mechanisms and clinical applications. Nucl Med Biol. 2006;33(3):287–94.
Pirotte B, Goldman S, Massager N, David P, Wikler D, Vandesteene A, et al. Comparison of 18F-FDG and 11C-methionine for PET-guided stereotactic brain biopsy of gliomas. J Nucl Med. 2004;45(8):1293–8.
Langen KJ, Floeth FW, Stoffels G, Hamacher K, Coenen HH, Pauleit D. Improved diagnostics of cerebral gliomas using FET PET. Z Med Phys. 2007;17(4):237–41.
Goldman S, Levivier M, Pirotte B, Brucher JM, Wikler D, Damhaut P, et al. Regional methionine and glucose uptake in high-grade gliomas: a comparative study on PET-guided stereotactic biopsy. J Nucl Med. 1997;38(9):1459–62.
Kracht LW, Miletic H, Busch S, Jacobs AH, Voges J, Hoevels M, et al. Delineation of brain tumor extent with [11C]L-methionine positron emission tomography: local comparison with stereotactic histopathology. Clin Cancer Res. 2004;10(21):7163–70.
Miwa K, Shinoda J, Yano H, Okumura A, Iwama T, Nakashima T, et al. Discrepancy between lesion distributions on methionine PET and MR images in patients with glioblastoma multiforme: insight from a PET and MR fusion image study. J Neurol Neurosurg Psychiatry. 2004;75(10):1457–62.
Muragaki Y, Chernov M, Maruyama T, Ochiai T, Taira T, Kubo O, et al. Low-grade glioma on stereotactic biopsy: how often is the diagnosis accurate? Minim Invasive Neurosurg. 2008;51(5):275–9.
Pauleit D, Floeth F, Hamacher K, Riemenschneider MJ, Reifenberger G, Müller HW, et al. O-(2-[18F]fluoroethyl)-L-tyrosine PET combined with MRI improves the diagnostic assessment of cerebral gliomas. Brain. 2005;128(Pt 3):678–87.
Pirotte B, Goldman S, Bidaut LM, Luxen A, Stanus E, Brucher JM, et al. Use of positron emission tomography (PET) in stereotactic conditions for brain biopsy. Acta Neurochir (Wien). 1995;134(1–2):79–82.
Langen KJ, Bartenstein P, Boecker H, Brust P, Coenen HH, Drzezga A, et al. German guidelines for brain tumour imaging by PET and SPECT using labelled amino acids. Nuklearmedizin. 2011;50(4):167–73.
Vander BT, Asenbaum S, Bartenstein P, Halldin C, Kapucu O, Van Laere K, et al. EANM procedure guidelines for brain tumour imaging using labelled amino acid analogues. Eur J Nucl Med Mol Imaging. 2006;33(11):1374–80.
Heinzel A, Stock S, Langen KJ, Müller D. Cost-effectiveness analysis of amino acid PET guided surgery for supratentorial high-grade gliomas. J Nucl Med. 2011; in Press.
Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach. Med Decis Mak. 1985;5(2):157–77.
Meltzer MI, Dennis DT, Orloski KA. The cost effectiveness of vaccinating against Lyme disease. Emerg Infect Dis. 1999;5(3):321–8.
Burgos JL, Gaebler JA, Strathdee SA, Lozada R, Staines H, Patterson TL. Cost-effectiveness of an intervention to reduce HIV/STI incidence and promote condom use among female sex workers in the Mexico-US border region. PLoS One. 2010;5(6):e11413.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96.
Uyl-de Groot CA, Stupp R, van der Bent M. Cost-effectiveness of temozolomide for the treatment of newly diagnosed glioblastoma multiforme. Expert Rev Pharmacoecon Outcomes Res. 2009;9(3):235–41.
Plotkin M, Blechschmidt C, Auf G, Nyuyki F, Geworski L, Denecke T, et al. Comparison of F-18 FET-PET with F-18 FDG-PET for biopsy planning of non-contrast-enhancing gliomas. Eur Radiol. 2010;20(10):2496–502.
Ginsberg LE, Fuller GN, Hashmi M, Leeds NE, Schomer DF. The significance of lack of MR contrast enhancement of supratentorial brain tumors in adults: histopathological evaluation of a series. Surg Neurol. 1998;49(4):436–40.
Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. Part 1: ethical and scientific issues. Ann Intern Med. 2000;133(6):455–63.
Miller FG, Brody H. What makes placebo-controlled trials unethical? Am J Bioeth. 2002;2(2):3–9.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heinzel, A., Stock, S., Langen, KJ. et al. Cost-effectiveness analysis of FET PET-guided target selection for the diagnosis of gliomas. Eur J Nucl Med Mol Imaging 39, 1089–1096 (2012). https://doi.org/10.1007/s00259-012-2093-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2093-0