Abstract
Purpose
Despite recent advances in clinical imaging modalities, differentiation of pancreatic masses remains difficult. Here, we tested the diagnostic accuracy of molecular-based imaging including 3′-deoxy-3′-[18F]fluorothymidine (FLT) positron emission tomography (PET) and [18F]fluorodeoxyglucose (FDG) PET/CT in patients with suspected pancreatic masses scheduled to undergo surgery.
Methods
A total of 46 patients with pancreatic tumours suspicious for malignancy and scheduled for resective surgery were recruited prospectively. In 41 patients, FLT PET and FDG PET/CT scans were performed. A diagnostic CT performed on a routine basis was available in 31 patients. FLT PET and FDG PET/CT emission images were acquired according to standard protocols. Tracer uptake in the tumour [FDG and FLT standardized uptake value (SUV)] was quantified by the region of interest (ROI) technique. For FDG PET/CT analysis, correct ROI placement was ensured via side-by-side reading of corresponding CT images.
Results
Of 41 patients, 33 had malignancy, whereas 8 patients had benign disease. Visual analysis of FDG and FLT PET resulted in sensitivity values of 91% (30/33) and 70% (23/33), respectively. Corresponding specificities were 50% (4/8) for FDG PET and 75% (6/8) for FLT PET. In the subgroup of patients with contrast-enhanced CT (n = 31), sensitivities were 96% (PET/CT), 88% (CT alone), 92% (FDG PET) and 72% (FLT PET), respectively. Mean FLT uptake in all malignant tumours was 3.0 (range SUVmax 1.1–6.5; mean FDG SUVmax 7.9, range 3.3–17.8; p < 0.001).
Conclusion
For differentiation of pancreatic tumours, FDG PET and FDG PET/CT showed a higher sensitivity but lower specificity than FLT PET. Interestingly, visual analysis of FLT PET led to two false-positive findings by misinterpreting physiological bowel uptake as pathological FLT uptake in the pancreas. Due to the limited number of patients, the clinical value of adding FLT PET to the diagnostic workup of pancreatic tumours remains to be determined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite recent advances in clinical imaging and biomarker identification, differential diagnosis of pancreatic masses remains challenging. Chronic pancreatitis (CP) is considered as one of the risk factors for the development of pancreatic cancer. Due to several overlapping morphological features, differentiation of pseudotumoral masses as a consequence of CP and benign/malignant tumours is frequently impossible [1]. To date, standard diagnostic workup includes computed tomography (CT), endoscopic ultrasound (EUS), and EUS-guided fine-needle aspiration (EUS FNA) as well as magnetic resonance imaging (MRI) and positron emission tomography (PET). Yet, the most accurate diagnostic algorithm remains to be determined. As compared to diagnostic imaging tests, invasive procedures such as EUS FNA also have an unsatisfying sensitivity of 73% for detection of pancreatic cancer [2]. Moreover, a negative biopsy in the case of a radiologically and/or clinically suspicious lesion cannot exclude pancreatic cancer.
A number of studies investigated the role of PET with the glucose analogue 18F-fluorodeoxyglucose (FDG) for better discrimination of benign from malignant tumours [3–5]. Despite an encouragingly high sensitivity, FDG has been reported to accumulate also in inflammatory lesions, thereby reducing the specificity of PET [6]. New, potentially more specific radiopharmaceuticals for clinical PET imaging have been recently introduced. The thymidine analogue 3′-deoxy-3′-[18F]fluorothymidine (FLT) [7] allows the non-invasive visualization of proliferating tissues. In a previously published pilot study, we have shown that focal FLT uptake was exclusively detected in malignant tumours of the pancreas [8]. In the present study, we aimed to assess FLT PET in a larger cohort. Moreover, this prospective trial was designed to test the diagnostic accuracy of FLT PET in comparison to the more established hybrid imaging of FDG PET in combination with contrast-enhanced CT (CECT) in patients with suspected pancreatic masses.
Materials and methods
Inclusion criteria
Between September 2008 and April 2009, patients referred to the Department of Surgery of the Klinikum rechts der Isar, Technische Universität München with a pancreatic mass suspicious for malignancy or CP were clinically evaluated. Surgical therapy was indicated where malignancy could not be excluded. The indications for surgery for CP patients were medically intractable pain or secondary complications of CP-like gastric outlet or biliary obstruction. Patients older than 18 years were invited to participate in this prospective study. If patients were willing to participate, informed consent was obtained. The study protocol was approved by the local Ethics Committee of the Technische Universität München.
Patient characteristics
Forty-six patients fulfilling the inclusion criteria were included in the study. One patient withdrew consent before undergoing FLT PET, and another patient was censored since the final histological report revealed leiomyosarcoma. In the remaining 44 patients, 28 were male and 16 were female (median age 65 ± 12 years, range 34–86 years).
Diagnostic workup
Imaging procedures included abdominal ultrasound, endoscopic retrograde cholangiopancreatography (ERCP), endosonography (EUS ± FNA biopsy or cytology), MRI and CT of the chest and abdomen, as clinically indicated. FLT PET imaging was performed in 42 patients, whereas in 2 patients an FLT scan was not performed due to logistic reasons; 43 patients underwent an FDG PET/CT scan. The median time interval between FLT and FDG PET scans was 1 day (range 1–6 days). A diagnostic CT with arterial and portal venous phase as well as appropriate transaxial, coronal and sagittal reconstruction was available in 32 patients. In the remaining patients, preoperative diagnostic workup was performed on an outpatient basis and the corresponding CT studies were either not performed in arterial and portal venous phase or did not meet the quality requirements for diagnostic CT evaluation. In a subgroup of 31 patients a diagnostic CT scan, FLT PET and FDG PET/CT were available. Twelve patients were referred with a recent CECT; therefore, FDG PET/CT was performed without CECT. Instead, a “low-dose” CT was performed to ensure proper localization of PET lesions. For further details, see Table 1.
3′-Deoxy-3′-[18F]fluorothymidine PET imaging
3′-Deoxy-3′-[18F]fluorothymidine was synthesized as previously described [8]. Imaging was performed on a whole-body high-resolution PET scanner (ECAT HR+, Siemens/CTI, Knoxville, TN, USA). This scanner simultaneously acquires 47 contiguous slices with a slice thickness of 3.4 mm. The in-plane image resolution of transaxial images was approximately 8 mm full-width at half-maximum (FWHM), with an axial resolution of approximately 5 mm FWHM. Static emission images were acquired 45 min after injection of approximately 300 MBq FLT. Correction of emission data was performed as previously reported [8].
[18F]Fluorodeoxyglucose PET/CT imaging
FDG PET/CT scans were performed on a Sensation 16 Biograph PET/CT scanner (Siemens Medical Solutions, Erlangen, Germany) as part of the diagnostic workup. Patients fasted 6 h before the PET scan and blood glucose levels were measured before each PET examination. All measured values were less than 150 mg/dl and showed no significant alterations. The CT acquisition protocol included a low-dose CT (26 mAs, 120 kV, 0.5 s per rotation, 5 mm slice thickness) from the base of the skull to mid-thigh for attenuation correction with diluted oral contrast (Telebrix, 300 mg) followed by the PET scan. All PET scans were acquired 90 min after intravenous injection of 300–400 MBq of FDG in 3-D mode with an acquisition time of 3 min per bed position. Images were reconstructed by an attenuation-weighted ordered subsets expectation maximization algorithm (4 iterations, 8 subsets) followed by a post-reconstruction smoothing Gaussian filter (5 mm FWHM).
Image interpretation
FLT PET, FDG PET/CT and CT scans were individually read by blinded interpreters comprising two board certified nuclear medicine physicians and a board certified radiologist without knowledge of the clinical history other than the study inclusion criteria. Visual assessment was done by using a five-point scale for interpretation of FDG PET, FDG PET/CT and CT scans. The five-point scale was defined by the following criteria: 1 = definitely malignant, 2 = probably malignant, 3 = equivocal, 4 = probably benign and 5 = definitely benign. Regarding FLT PET studies, in which no anatomical information was available, studies were either interpreted as positive (definitely malignant) or negative (definitely benign). FLT PET, CT, FDG PET and FDG PET/CT were interpreted separately. Equivocal findings were interpreted as both false-positive and false-negative. Semi-quantitative evaluation of the PET and PET/CT studies was done by drawing a circular region of interest (ROI) (diameter 1.5 cm) with the TrueD software (Siemens Medical Solutions). Mean standardized uptake values (SUV) were calculated from each ROI using the formula: SUV = measured activity concentration (Bq/g) × body weight (g)/injected activity (Bq).
Reference methods for assessment of pancreatic tumours
Of the included patients, 75% (33/44) underwent surgery. In 11 patients, surgery was not performed due to the following reasons: liver metastasis (LM) 3, peritoneal carcinosis + LM 2, lung metastasis 2, non-resectable tumour 1, non-resectable tumour + LM 1, clinically unfit 1, peritonitis 1. Histopathology or cytology served as reference for malignancy and was available in all 44 patients. In the subgroup of 31 patients with diagnostic CT, FLT PET and FDG PET/CT, surgery was performed in 24 (77%) patients. The median time interval between FLT PET and surgery was 4 days (range 1–99 days). One patient with a cystic adenocarcinoma presented during diagnostic workup clinically suspicious, but histologically unverified lung lesions and consecutively underwent 3 months of chemotherapy prior to surgery (99 days between FLT PET scan and surgery). The next longest time intervals between FLT PET and surgery were 21, 13, 12, 9 and 8 days, respectively.
Statistical analysis
Statistical analyses were performed using PASW Statistics software (version 18.0; SPSS, Inc., Chicago, IL, USA). Quantitative values were expressed as mean ± standard deviation, median and range. Exact 95% confidence intervals (CI) were reported for estimates of sensitivity and specificity indicating statistically significant predictive capability if the critical value of 0.5 is not included. All analyses were performed two-sided at a 5% level of significance.
Results
Histopathology and clinical stage
Malignant disease was proven in 34 patients, including all 11 patients not undergoing surgery. In ten patients, histopathology revealed benign disease. In the subgroup of 31 patients, pathological workup proved a malignant pancreatic tumour in 25 patients and benign disease in 6 patients.
The tumour stages of the 34 patients presenting malignancy were T1 in 1, T2 in 6, T3 in 15 and T4 in 12 patients, respectively. However, in six patients, T staging was only clinically available (cT2 in three, cT3 in one and cT4 in two patients, respectively). Corresponding tumour sizes ranged from 1.2 to 8.5 cm (mean 4.0 cm, median 4.0 cm) with the second smallest tumour measuring 2.2 cm.
Surgical procedures
Operations performed were as follows: pylorus-preserving pancreatoduodenectomy (15), classic Whipple (1), pancreas tail resection (12), total pancreatectomy (4), duodenum-preserving pancreatic head resection (1), double bypass (5), laparotomy and exploration (4) and thoracoscopy (1).
FLT PET and FDG PET
FLT PET was performed in 42 patients with a mean SUVmax of the pancreatic lesion of 2.9 (median 2.7, range 1.1–6.5). Visual analysis rated FLT scans positive in 26 patients, whereas 16 scans were rated as negative. FDG PET was available in 43 patients and a mean SUVmax of 7.2 (median 6.5, range 2.1–17.8) was calculated in pancreatic lesions being significantly higher than the FLT uptake (p < 0.001). Of the FDG PET/CT scans, 7 were interpreted as benign and 36 were reported to be positive. Correlation of FLT and FDG scans with histopathology was performed in the subgroup of 41 patients imaged with both tracers. Of 33 patients rated malignant at histopathology, 23 presented a positive FLT scan, resulting in a sensitivity of 70%. For FDG PET, sensitivity was calculated to be 91% (30/33). Corresponding specificity and accuracy values were 75% (6/8) and 71% (29/41) for FLT PET and 50% (4/8) and 83% (34/41) for FDG PET/CT, respectively (see also Table 2 and Fig. 1).
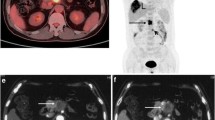
A 61-year-old male patient with a mass in the pancreatic head. The patient underwent FLT PET scan indicating an intense focal FLT uptake in transaxial (a), coronal (b) and sagittal (c) sections of FLT PET (black arrows). In the corresponding FDG PET/CT (fused images are displayed in d, venous phase transaxial CT in e) there is also an intense uptake in the pancreatic head. Histology revealed a pT2 pN1 adenocarcinoma of the pancreatic head
Receiver-operating characteristic analysis for discrimination of benign and malignant lesions resulted in a cut-off value of SUVmax = 2.0 for FLT (AUC 0.594) and a cut-off value of SUVmax = 3.5 for FDG (AUC 0.836). The corresponding sensitivities and specificities were 70 and 67% for FLT, and 97 and 63% for FDG, respectively. Correlation of FLT and FDG uptake with tumour stage (T1/T2 vs T3/T4) in all patients presenting malignancy resulted in significantly higher FDG uptake values in T3/T4 patients (p = 0.048), whereas for FLT statistical significance was not reached (p = 0.699).
FLT PET, FDG PET, CECT and FDG PET/CT
In the subgroup of 31 patients, all three modalities were performed. Of the 25 patients with malignant disease, FLT PET was positive in 18 patients (sensitivity 72%). Corresponding sensitivities for FDG PET, CECT and FDG PET/CT were 92% (23/25), 88% (22/25) and 96% (24/25); see also Table 3. FLT scan was true-negative in four of six patients. Numbers of true-negative scans were 2, 0 and 1 for FDG PET, CECT and FDG PET/CT; because of the low number of histopathologically benign findings, specificities were not calculated.
Discussion
To the best of our knowledge this is the largest clinical study comparing FLT PET and FDG PET/CT with CECT in patients with suspected pancreatic masses scheduled to undergo resective surgery. On the basis of prior studies this trial was designed to investigate the potential of in vivo proliferation imaging in a clinical highly relevant setting using histopathology as reference. For assessment of relevance of FLT PET we used the clinically widely accepted imaging modalities CECT and FDG PET/CT. The primary aim of this study was to assess whether molecular imaging of proliferation in vivo adds relevant additional information to the diagnostic algorithm in pancreatic tumours.
In this study, FDG PET, CECT and FDG PET/CT detected malignant pancreatic disease with high sensitivities (92, 88 and 96%, respectively). This observation is in line with previously published sensitivity values [3, 4, 9, 10]. Sensitivity of FLT PET was 72% in the subgroup of 31 patients with all imaging modalities available and 70% in all 41 patients. This value is comparable to the sensitivity value of 74% reported in our previous trial [8]. Interestingly, there was no significant decrease in sensitivity between the two study cohorts although the inclusion criteria of the present trial comprised patients scheduled to undergo surgery, translating into a study cohort with smaller tumours and less extensive disease. However, the strongest reasons for false-negative FLT PET scans comprise small tumour size due to partial volume effects, low tumour grade and a low tumour proliferation [8, 11].
The reported drawbacks of FDG PET, CECT and FDG PET/CT have always been the limited specificity with false-positive findings in FDG PET due to tracer uptake in inflammatory lesions or false-positive reports at CT caused by pseudotumoral masses due to CP. In contrast, FLT PET is deemed to be a very specific tracer. In our previous study we reported a specificity of 100% underlining its adequacy for differentiation of undefined lesions, especially if CP cannot be excluded [8]. Even though this trial was not designed to assess the specificity of any of the investigated imaging modalities (only patients scheduled to undergo surgery and therefore having strong suggestive signs of malignancy in prior workup), FLT PET turned out to be more specific than FDG PET, CECT and FDG PET/CT by presenting the lowest number of false-positive findings. However, in contrast to our previous trial we observed two false-positive findings at FLT PET. As FLT PET was interpreted independently without concomitant CT, no anatomical information was available for interpretation of focal FLT uptake. Re-evaluation/assessment of these false-positive findings revealed misinterpretation of physiological bowel uptake as pathological FLT uptake in the pancreas. Nevertheless, non-specific uptake in reactive cervical lymph nodes in patients with head and neck cancer has recently been described [12]. Therefore, an increased proliferation rate is not specific for malignant tumours and, thus, unspecific uptake of FLT in reactive nodes or inflammatory pancreatic lesions cannot be excluded in future trials. Furthermore, our observation of false-positive findings due to lack of anatomical information underlines the need for combined functional and morphological imaging. Future studies will therefore be performed on PET/CT scanners, reducing the probability of false-positive findings due to misinterpretation because of missing anatomical information. This set-up would also overcome another limitation of our study comparing FLT PET scans and FDG PET/CT scans performed on the same scanner and guaranteeing a better comparability. The particular design of this study including patients with pancreatic masses scheduled to undergo surgery resulted in a selection bias towards a lower rate of benign lesions and therefore a limited validity regarding the specificity of the investigated modalities. Another important limitation of FLT PET is the previously reported limited sensitivity in N and M staging, especially in liver metastases due to the high physiological liver uptake [8, 13, 14]. However, introduction of combined MRI and PET scanners bears a great potential for differentiation of pancreatic tumours and tumour staging and warrants further investigation.
In conclusion, for differentiation of pancreatic tumours, FDG PET and FDG PET/CT showed a higher sensitivity than FLT PET. FLT PET presented fewer false-positive findings than FDG PET, CECT or FDG PET/CT, and the rate of false-positive findings might be further reduced by hybrid FLT PET/CT imaging. Due to the limited number of patients included, the clinical value of adding FLT PET to the diagnostic workup of pancreatic tumours remains to be determined.
References
Balthazar EJ. Pancreatitis associated with pancreatic carcinoma. Preoperative diagnosis: role of CT imaging in detection and evaluation. Pancreatology 2005;5:330–44.
Ardengh JC, Lopes CV, Campos AD, Pereira de Lima LF, Venco F, Módena JL. Endoscopic ultrasound and fine needle aspiration in chronic pancreatitis: differential diagnosis between pseudotumoral masses and pancreatic cancer. JOP 2007;8:413–21.
Diederichs CG, Staib L, Glatting G, Beger HG, Reske SN. FDG PET: elevated plasma glucose reduces both uptake and detection rate of pancreatic malignancies. J Nucl Med 1998;39:1030–3.
Friess H, Langhans J, Ebert M, Beger HG, Stollfuss J, Reske SN, et al. Diagnosis of pancreatic cancer by 2[18F]-fluoro-2-deoxy-D-glucose positron emission tomography. Gut 1995;36:771–7.
Heinrich S, Goerres GW, Schäfer M, Sagmeister M, Bauerfeind P, Pestalozzi BC, et al. Positron emission tomography/computed tomography influences on the management of resectable pancreatic cancer and its cost-effectiveness. Ann Surg 2005;242:235–43.
Buck AC, Schirrmeister HH, Guhlmann CA, Diederichs CG, Shen C, Buchmann I, et al. Ki-67 immunostaining in pancreatic cancer and chronic active pancreatitis: does in vivo FDG uptake correlate with proliferative activity? J Nucl Med 2001;42:721–5.
Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med 1998;4:1334–6.
Herrmann K, Eckel F, Schmidt S, Scheidhauer K, Krause BJ, Kleeff J, et al. In vivo characterization of proliferation for discriminating cancer from pancreatic pseudotumors. J Nucl Med 2008;49:1437–44. doi:10.2967/jnumed.108.052027.
Buchs NC, Bühler L, Bucher P, Willi JP, Frossard JL, Roth AD, et al. Value of contrast-enhanced 18F-fluorodeoxyglucose positron emission tomography/computed tomography in detection and presurgical assessment of pancreatic cancer: a prospective study. J Gastroenterol Hepatol 2011;26:657–62. doi:10.1111/j.1440-1746.2010.06525.x.
Tang S, Huang G, Liu J, Liu T, Treven L, Song S, et al. Usefulness of 18F-FDG PET, combined FDG-PET/CT and EUS in diagnosing primary pancreatic carcinoma: a meta-analysis. Eur J Radiol 2011;78:142–50. doi:10.1016/j.ejrad.2009.09.026.
Quon A, Chang ST, Chin F, Kamaya A, Dick DW, Loo BW Jr., et al. Initial evaluation of (18)F-fluorothymidine (FLT) PET/CT scanning for primary pancreatic cancer. Eur J Nucl Med Mol Imaging 2008;35:527–31.
Troost EG, Vogel WV, Merkx MA, Slootweg PJ, Marres HA, Peeters WJ, et al. 18F-FLT PET does not discriminate between reactive and metastatic lymph nodes in primary head and neck cancer patients. J Nucl Med 2007;48:726–35.
Buck AK, Hetzel M, Schirrmeister H, Halter G, Möller P, Kratochwil C, et al. Clinical relevance of imaging proliferative activity in lung nodules. Eur J Nucl Med Mol Imaging 2005;32:525–33.
Francis DL, Freeman A, Visvikis D, Costa DC, Luthra SK, Novelli M, et al. In vivo imaging of cellular proliferation in colorectal cancer using positron emission tomography. Gut 2003;52:1602–6.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Herrmann and M. Erkan contributed equally to this work.
Rights and permissions
About this article
Cite this article
Herrmann, K., Erkan, M., Dobritz, M. et al. Comparison of 3′-deoxy-3′-[18F]fluorothymidine positron emission tomography (FLT PET) and FDG PET/CT for the detection and characterization of pancreatic tumours. Eur J Nucl Med Mol Imaging 39, 846–851 (2012). https://doi.org/10.1007/s00259-012-2061-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2061-8