Abstract
Purpose
We assessed the role of the maximum standardized uptake value (SUVmax) of bone marrow and the extramedullary lesion with the highest SUVmax in positron emission tomography/computed tomography (PET/CT) of newly diagnosed multiple myeloma (MM) patients in predicting overall survival (OS).
Methods
A total of 61 newly diagnosed patients (55 MM and 6 plasmacytoma) were enrolled in the study [37 men and 24 women with a median age of 57 years (range 28–80 years)]. The SUVmax of bone marrow and the extramedullary lesion in PET/CT was correlated with the levels of β2-microglobulin, C-reactive protein (CRP), albumin, creatinine, per cent of bone marrow plasma cells, serum free light chain (FLC) ratio, International Staging System (ISS) score and Durie-Salmon stage.
Results
The extramedullary lesion with the highest SUVmax showed significant correlation with bone marrow fluorodeoxyglucose (FDG) uptake (p = 0.027) and near significant correlation with ISS (p = 0.048). Bone marrow SUVmax correlated significantly with the per cent of bone marrow plasma cell count (p = 0.024), CRP (p = 0.012) and ISS (p = 0.013). In stage III MM the mean values of SUVmax in extramedullary lesions were significantly higher than stages I and II (6.23 ± 6.32 vs 2.85 ± 3.44, p = 0.023). The serum FLC ratio did not show any correlation with SUVmax of lesions and bone marrow (p > 0.05). Forty-four MM patients with FDG-positive lesions in PET/CT showed inferior 5-year estimated survival (61.73%) when compared to 11 patients without FDG-positive lesions, all of whom were alive (p = 0.01). In multivariate analysis an extramedullary lesion with the highest SUVmax was the only independent predictor of OS (p = 0.03).
Conclusion
PET/CT allows identification of high-risk myeloma patients, and extramedullary lesions with the highest SUVmax independently predict inferior OS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is a cancer of the plasma cells which accounts for more than 10% of all haematological malignancies [1]. MM is characterized by the proliferation of a single clone of plasma cells derived from B cells in the bone marrow and production of monoclonal immunoglobulins. The diagnosis and staging of MM is based on laboratory parameters, bone marrow biopsy and conventional radiographs showing lytic bone lesions, osteoporosis or pathological fractures [2, 3]. In MM patients imaging modalities should serve to verify the extent of skeletal and extraskeletal involvement, supply the information required by the staging system, and assess stability of involved bones and treatment response [4, 5]. As conventional radiographs can significantly underestimate the extent of bone and extramedullary involvement, more advanced imaging modalities including computed tomography (CT), whole-body scintigraphy and magnetic resonance imaging (MRI) have been used to improve the detection of tumour burden. However, these imaging methods may not be able to differentiate treated lesions and viable tumour tissue. In recent years, positron emission tomography (PET) has also been used in MM imaging. A marked accumulation of 18F-fluorodeoxyglucose (FDG) in the bone lesions of MM patients with FDG PET imaging has been shown in case reports [6–8]. Preliminary reports have shown that high uptake of 18F-FDG by tumour cells is associated with the metabolic activity of the tumour in MM [9–11].
The aim of this study was to investigate the role of the maximum standardized uptake value (SUVmax) of bone marrow and the extramedullary lesion with the highest metabolic activity on PET/CT in predicting survival of newly diagnosed myeloma patients.
Materials and methods
Patients
A total of 61 previously untreated, newly diagnosed patients (55 MM and 6 plasmacytoma) were enrolled in the study. The local Ethics Committee of our university approved the study. The study group consisted of 37 men and 24 women with a median age of 57 years (range 28–80 years). The median follow-up time was 26 months (range 1–211 months) starting from the date of diagnosis up to January 2010 or when death occurred.
All eligible patients underwent staging workup for MM consisting of whole blood count, routine biochemistry, serum levels of β2-microglobulin, C-reactive protein (CRP), serum and urinary immunofixation, complete immunoglobulin and serum free light chain (FLC) concentrations, 24-h proteinuria, bone marrow aspirate and biopsy. Conventional radiographic skeletal surveys of the skull, ribs, spine, pelvis, humerus, femur, MRI of the vertebral column and head to toe whole-body 18F-FDG PET/CT scans were examined in all patients.
Patients were diagnosed as having MM or plasmacytoma on the basis of the criteria defined by the International Myeloma Working Group (IMWG) [2]. According to the staging system of Durie and Salmon, 5 (9.1%) MM patients had stage I disease, 6 (10.9%) stage II disease and 44 (80%) stage III disease. Twelve of the patients had abnormal renal function with serum creatinine values ≥ 2.0 mg/dl. The light chain component was kappa in 31 (56.4%) MM patients and lambda in 24 (43.63%) MM patients. International Staging System (ISS) values available for 52 patients were I in 31 patients (50.8%), II in 11 (18%) and III in 10 (16.4%) patients. Patient characteristics are shown in Table 1. Thirty-six patients (59%) under 65 years of age who were candidates for autologous stem cell transplantation (ASCT) received an anthracycline-based VAD (vincristine, Adriamycin, dexamethasone) chemotherapy regimen according to the policy of the national health insurance at the time of diagnosis. Fifteen patients (24.6%) ≥ 65 years of age, who were not candidates for ASCT, received either melphalan-prednisone or melphalan-prednisone-thalidomide as initial treatment (ten with melphalan-prednisone and five with melphalan-prednisone-thalidomide). Three patients (4.9%) received bortezomib-dexamethasone, one patient (1.6%) received thalidomide-dexamethasone and two patients (3.3%) received radiotherapy as initial treatment according to the individual condition of the patient. A total of 26 patients (42.6%) underwent high-dose chemotherapy and haematopoietic stem cell transplantation (HSCT) during the follow-up period (22 patients autologous, 3 allogeneic and 1 tandem allogeneic after autologous HSCT). Treatment response was defined according to the European Group for Blood and Marrow Transplantation criteria, introduced by Bladé et al. [12]. After a median follow-up time of 26 months (range 1–211 months), disease status was complete remission in 19 (31.1%), partial remission in 12 (19.7%), refractory or relapse in 11 (18%), less than partial remission in 6 (9.8%) and death in 13 (21.3%) patients. Enhanced 18F-FDG uptake in areas other than bone marrow was interpreted as extramedullary myeloma.
PET/CT
All 18F-FDG PET/CT imagings were done according to the standard protocol. Patients fasted for at least 6 h and their pre-injection blood glucose levels were below 160 mg/dl. Sixty minutes after the injection of 18F-FDG (dose 0.14 mCi/kg) imaging was started on a Discovery LS PET/CT scanner (General Electric Medical Systems, Milwaukee, WI, USA). Intravenous contrast material was not used. A real whole-body (head to toe) emission PET scanning in 3-D mode (at 3 min/bed position) was done following a low-dose (120 keV, 10–100 mAs) whole-body CT that was principally used for attenuation correction purposes. The acquired PET and CT images were displayed as coregistered orthogonal slices (axial, coronal and sagittal) with a slice thickness of 3.75 mm.
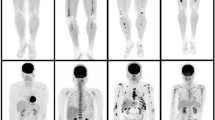
All 18F-FDG PET/CT images were visually evaluated and quantified by a single nuclear medicine physician. In patients with more than one lesion with positive FDG uptake, the lesion with the highest SUVmax was included in the analysis. In the quantification of 18F-FDG uptake of lesions SUVmax was used. SUVmax was calculated using the following formula: tissue concentration (MBq/g)/injected dose (MBq)/body weight (g). For the quantitive evaluation of bone marrow 18F-FDG uptake, the mean of bone marrow SUVs (SUVmarrow) that was calculated under CT guided anatomical reference from the third to fifth lumbar vertebral corpuses using a cubical volume of interest (VOI) excluding the cortical bone was used. Other lumbar or thoracic vertebrae were used if a focal lesion in one of these lumbar vertebrae was observed (Figs. 1 and 2).
Statistical methods
The statistical evaluation of the data was performed using SPSS software for Windows V.11.5 (SPSS Inc., Chicago, IL, USA). Differences between groups were analysed by Student’s t test. Relationships between variables were evaluated with Pearson’s or Spearman’s correlation tests. A value of p < 0.05 was considered to represent a statistically significant difference. Survival analysis was carried out by using Kaplan-Meier and log-rank tests. Overall survival (OS) was measured from the date of registration until death from any cause. Survivors were censored at the time of last contact. Univariate and multivariate analyses of prognostic factors were carried out using Cox regression. The variables found to be independently predictive of survival in an univariate analysis were entered into the multiple regression method. A receiver-operating characteristic (ROC) curve analysis was performed to assess the accuracy of SUVmax in predicting the degree of bone marrow plasma cell infiltration.
Results
Fifty-five patients with MM and six patients with plasmacytoma were examined with 18F-FDG PET/CT scans as part of their imaging during initial diagnosis. The clinical significance of FDG uptake in bone marrow and the extramedullary lesion with the highest SUVmax was evaluated by correlating uptake values with the levels of β2-microglobulin, CRP, albumin, creatinine, per cent of bone marrow plasma cells, serum FLC ratio, ISS and stage according to Durie-Salmon (Table 2). In 49 of 61 patients (80.3%) there were ≥ 1 extramedullary lesions with FDG uptake. The extramedullary lesion with the highest SUVmax was used for the analysis. The SUVmax of extramedullary lesions showed significant correlation with bone marrow FDG uptake (r = 0.28, p = 0.027) and ISS (r = 0.27, p = 0.048). However, the extramedullary lesion with the highest SUVmax showed no correlation with levels of β2-microglobulin, CRP, albumin, creatinine, per cent of bone marrow plasma cells and stage according to Durie-Salmon. Bone marrow SUVmax significantly correlated with the per cent of bone marrow plasma cell count (r = 0.301, p = 0.024), CRP (r = 0.377, p = 0.012) and ISS (r = 0.350, p = 0.013). Haemoglobin levels at the time of PET/CT scans did not show any correlation with bone marrow 18F-FDG uptake (r = 0.189, p = 0.106). The mean values of SUVmax in extramedullary lesions were significantly higher in stage III MM when compared to stages I and II (6.23 ± 6.32 vs 2.85 ± 3.44, p = 0.023). Bone marrow FDG uptake did not show a significant difference between MM stages (p > 0.05). In kappa and lambda light chain MM patients the serum FLC ratio did not show any correlation with SUVmax of bone marrow and SUVmax of extramedullary lesions [(r = 0.133, p = 0.599) and (r = 0.229, p = 0.345) and (r = 0.230, p = 0.359) and (r = 0.155, p = 0.526), respectively]. In ROC curve analysis bone marrow SUVmax greater than 2.05 significantly predicted the presence of > 30% plasma cells in bone marrow (sensitivity 71.9% and specificity 58.2%, p = 0.04) (Fig. 3). Involvement of bone marrow in MRI also predicted the presence of > 30% plasma cells (p = 0.004). In univariate regression analysis there was a significant relationship between bone marrow plasma cell counts of > 30% and bone marrow involvement in both MRI and PET/CT. However, in multivariate analysis MRI independently predicted the bone marrow plasma cell counts > 30% (p = 0.018).
The median follow-up time for 55 MM patients was 26 months (range 1–211 months) and the 5-year estimated OS was 69.96% (Fig. 4). In six patients with plasmacytoma, the 5-year estimated OS was 66.67%. Forty-four MM patients with FDG uptake-positive extramedullary lesions in PET/CT showed inferior 5-year estimated survival (61.73%) when compared to 11 patients without FDG-positive lesions, all of whom were alive (p = 0.01) (Fig. 5). In Cox regression analysis the SUVmax of the extramedullary lesions with the highest FDG uptake showed significant association with OS (p < 0.001; hazard ratio 1.16). We could not find a significant effect of bone marrow FDG uptake in PET/CT or bone marrow involvement in MRI on OS (p = 0.59 and p = 0.22, respectively). When a cutoff value 2.05 for bone marrow SUVmax was taken for OS analysis, the 5-year estimated survival was not significantly different in patients with bone marrow SUVmax ≤ 2.05 vs > 2.05 (71.9 vs 59.5%, p = 0.315) (Fig. 6).
In multivariate analysis of the parameters including age, creatinine, ISS, Durie-Salmon stage and SUVmax of the most significant lesions the only independent predictor of OS was SUVmax values of the lesions (p = 0.03).
Discussion
The present study shows that 18F-FDG uptakes of bone marrow and extramedullary lesions on PET/CT scans are significantly correlated with established prognostic factors including ISS and disease stage. Although 18F-FDG uptake of bone marrow on PET/CT scan significantly predicts the percentage of plasma cell infiltration, in multivariate analysis MRI was the independent predictor of the bone marrow plasma cell counts in MM patients. At baseline PET/CT scans higher levels of SUVmax of extramedullary lesions significantly predicted inferior OS. The diagnosis and staging of MM is based on laboratory parameters and imaging analysis. Appropriate use of imaging techniques is critical for the identification of the extent of disease. Although conventional skeletal survey is the gold standard in evaluating lytic bone lesions, this method leads to underestimation in diagnosing and staging of patients with MM [10, 13, 14]. In addition to conventional skeletal survey, MRI became the preferred imaging modality in the assessment of axial skeleton and bone marrow in staging of patients with MM [5, 13, 14). In our study we also demonstrated the correlation between bone marrow activity in MRI and the per cent of plasma cells. However, combinations of X-ray images, MRI and CT give information about the morphological extent of the disease, not the functional assessment. With respect to these standard imaging modalities a new imaging technique using PET/CT provides both functional and morphological assessment of patients with MM and solitary plasmacytoma [9, 11, 15–19].
In our study 80.3% of our patients demonstrated FDG uptake-positive focal lesions in PET/CT. There was a positive correlation between SUVmax of bone marrow and extramedullary lesions in reflecting disease activity. Patients with advanced disease stage had higher SUVmax for extramedullary lesions with respect to earlier disease stages. In a recent retrospective analysis of 66 patients with MM or related monoclonal gammopathies, whole-body PET identified additional multiple focal lesions in 25% of 16 newly diagnosed patients. In ten patients with nonsecretory MM during follow-up PET showed new focal sites of disease in 60% of patients. In relapsing patients PET identified new sites of involvement in 81% of patients. Negative PET findings strongly supported the diagnosis of monoclonal gammopathy with undetermined significance. In their study Durie et al. showed that both the presence of residual myeloma after treatment and the presence of extramedullary myeloma by PET indicate high-risk patients and poor prognosis [10].
According to correlation analysis, the SUVmax of bone marrow positively correlated with the parameters including the per cent of bone marrow plasma cells, CRP and ISS. As a functional imaging technique SUVmax of bone marrow > 2.05 in PET/CT scans significantly predicted > 30% plasma cells in bone marrow biopsies. In univariate regression analysis the presence of extramedullary lesions with FDG uptake predicted shorter OS. In Cox regression analysis extramedullary lesions with higher SUVmax were associated with inferior OS. However, neither FDG uptake of bone marrow in PET/CT nor the bone marrow involvement in MRI showed a significant association with OS. In multivariate Cox regression analysis higher SUVmax of extramedullary lesions remained an independent adverse prognostic factor for OS.
In recent years the widespread use of more sensitive imaging techniques has increased the awareness of extramedullary disease both at diagnosis and during follow-up. In a retrospective analysis of 1,003 MM patients in three time periods (1971–1993, 1994–1999 and 2000–2007), the incidence of extramedullary involvement at diagnosis (p = 0.02) and during follow-up (p = 0.03) significantly increased in the 2000–2007 time period. In this study the presence of extramedullary involvement at diagnosis was significantly associated with shorter progression-free survival (PFS) (18 versus 30 months, p = 0.003), while the median OS was not statistically different (p = 0.36). However, the presence of extramedullary disease at any time in the course of the disease was significantly associated with shorter OS and PFS (p < 0.0001 and p = 0.04, respectively). In the light of novel therapeutic agents and better supportive care in the treatment of MM, early detection of extramedullary disease with new whole-body imaging modalities may lead to improvement in survival [20].
PET/CT images give the opportunity to make functional and morphological assessment of lesions where FDG uptake indicates active MM. In the analysis of 33 patients with newly diagnosed MM, whole-body PET/CT was compared with whole-body 99mTc-methoxyisobutylisonitrile (MIBI) scintigraphy and MRI of the spine and pelvis. Whole-body PET/CT visualized more focal lesions (5.94 ± 9.29) than 99mTc-MIBI scintigraphy (1.91 ± 4.45) and MRI (1.54 ± 2.45) (p < 0.001). However, 99mTc-MIBI scintigraphy and MRI detected diffuse patterns of bone marrow involvement better than PET/CT. These three imaging methods either alone or in combination influenced the clinical management in 18% of patients [21]. Hur et al. also demonstrated that MRI is superior to FDG PET in detecting bone marrow involvement in the spine of patients with advanced MM [22].
There are limited data evaluating the prognostic value of FDG uptake in MM. Strauss et al. evaluated the impact of changes in kinetic parameters (SUV, the phosphorylation rate k3 and the fractal dimension) of FDG at baseline and prior to the second cycle of chemotherapy in 19 MM patients. Although they found a significant decrease in the kinetic parameters between baseline and the second PET study, they could not find a correlation between the changes in kinetic parameters and the PFS. However higher SUVs (> 4) and k3 values (> 0.07) at baseline PET predicted a significantly shorter PFS [23].
As part of total therapy 3 metastatic bone survey (MBS), MRI and FDG PET scanning were evaluated in 239 newly diagnosed MM patients. In the low-risk group defined according to the gene expression profiling, more than three focal lesions by PET predicted inferior OS and event-free survival (EFS). In the high-risk group all had a poor prognosis. This study analysed the role of early post-treatment PET/CT changes and found no effect on outcome. However, complete FDG suppression before transplantation conferred superior OS and EFS [24].
In another study bone marrow uptake was evaluated in 18 newly diagnosed MM patients who underwent MIBI and PET study. Mean SUV (mSUV) and target to background ratio (TG/BKG) significantly correlated with plasma cell percentage. The ROC analysis revealed a more rapid clinical course in patients with mSUV greater than 0.79. In univariate regression analysis mSUV, TG/BKG and β2-microglobulin were related to survival. In multiple regression analysis mSUV was the only independent predictor of survival [25].
Various imaging technologies have been used for the diagnosis and management of MM patients. Although the advantages of whole-body PET/CT over skeletal survey and MRI have been described in previous reports, it cannot be recommended for routine use in MM. Based on the recently available data, the IMWG recommended the use of PET/CT as an additional diagnostic tool in MM at baseline and during follow-up [13].
In conclusion, as mentioned in previous reports our data also support the observation that PET/CT allows identification of patients with high-risk myeloma. Higher SUVmax of extramedullary lesions independently predicted inferior OS in those patients.
References
Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1998. CA Cancer J Clin 1998;48:6–29.
International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol 2003;121:749–57.
Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer 1975;36:842–54.
Durie BG. The role of anatomic and functional staging in myloma: description of Durie/Salmon plus staging system. Eur J Cancer 2006;42:1539–43.
Delorme S, Baur-Melnyk A. Imaging in multiple myeloma. Eur J Radiol 2009;70:401–8.
Sasaki M, Ichiya Y, Kuwabara Y, Otsuka M, Fukumura T, Kawai Y, et al. Fluorine-18-fluorodeoxyglucose positron emission tomography in technetium-99m-hydroxymethylenediphosphate negative bone tumors. J Nucl Med 1993;34:288–90.
el-Shirbiny AM, Yeung H, Imbriaco M, Michaeli J, Macapinlac H, Larson SM. Technetium-99m-MIBI versus fluorine-18-FDG in diffuse multiple myeloma. J Nucl Med 1997;38:1208–10.
Orchard K, Barrington S, Buscombe J, Hilson A, Prentice HG, Mehta A. Fluoro-deoxyglucose positron emission tomography imaging for the detection of occult disease in multiple myeloma. Br J Haematol 2002;117:133–5.
Jadvar H, Conti PS. Diagnostic utility of FDG PET in multiple myeloma. Skeletal Radiol 2002;31:690–4.
Durie BGM, Waxman AD, D’Agnolo A, Williams CM. Whole-body (18)F-FDG PET identifies high-risk myeloma. J Nucl Med 2002;43:1457–63.
Schirrmeister H, Bommer M, Buck AK, Müller S, Messer P, Bunjes D, et al. Initial results in the assessment of multiple myeloma using 18F-FDG PET. Eur J Nucl Med Mol Imaging 2002;29(3):361–6.
Bladé J, Samson D, Reece D, Apperley J, Björkstrand B, Gahrton G, et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haematopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant. Br J Haematol 1998;102:1115–23.
Dimopoulos M, Terpos E, Comenzo RL, Tosi P, Beksac M, Sezer O, et al. International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple myeloma. Leukemia 2009;23:1545–56.
Lütje S, de Rooy JWJ, Croockewit S, Koedam E, Oyen WJG, Raymakers RA. Role of radiography, MRI and FDG-PET/CT in diagnosing, staging and therapeutical evaluation of patients with multiple myeloma. Ann Hematol 2009;88:1161–8.
Mileshkin L, Blum R, Seymour JF, Patrikeos A, Hicks RJ, Prince M. A comparison of fluorine-18 fluoro-deoxyglucose PET and technetium-99m sestamibi in assessing patients with multiple myeloma. Eur J Haematol 2004;72:32–7.
Schirrmeister H, Buck AK, Bergmann L, Reske SN, Bommer M. Positron emission tomography (PET) for staging of solitary plasmacytoma. Cancer Biother Radiopharm 2003;18:841–5.
Nanni C, Zamagni E, Farsad M, Castellucci P, Tosi P, Cangini D, et al. Role of 18F-FDG PET/CT in the assessment of bone involvement in newly diagnosed multiple myeloma: preliminary results. Eur J Nucl Med Mol Imaging 2006;33:525–31.
Breyer RJ, Mulligan ME, Smith SE, Line BR, Badros AZ. Comparison of imaging with FDG PET/CT with other imaging modalities in myeloma. Skeletal Radiol 2006;35:632–40.
Mulligan ME, Badros AZ. PET/CT and MR imaging in myeloma. Skeletal Radiol 2007;36:5–16.
Varettoni M, Corso A, Pica G, Mangiacavalli S, Pascutto C, Lazzarino M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol 2010;21:325–30.
Fonti R, Salvatore B, Quarantelli M, Sirignano C, Segreto S, Petruzziello F, et al. 18F-FDG PET/CT, 99mTc-MIBI, and MRI in evaluation of patients with multiple myeloma. J Nucl Med 2008;49:195–200.
Hur J, Yoon CS, Ryu YH, Yun MJ, Suh JS. Comparative study of fluorodeoxyglucose positron emission tomography and magnetic resonance imaging for the detection of spinal bone marrow infiltration in untreated patients with multiple myeloma. Acta Radiol 2008;49:427–35.
Dimitrakopoulou-Strauss DA, Hoffmann M, Bergner R, Uppenkamp M, Haberkorn U, Strauss LG. Prediction of progression-free survival in patients with multiple myeloma following anthracycline-based chemotherapy based on dynamic FDG-PET. Clin Nucl Med 2009;34:576–84.
Bartel TB, Haessler J, Brown LYT, Shaughnessy JD, van Rhee F, Anaissie E, et al. F18-fluorodeoxyglucose positron emission tomography in the context of other imaging techniques and prognostic factors in multiple myeloma. Blood 2009;114:2068–76.
Castellani M, Carletto M, Baldini L, Calori R, Longari V, Soligo D, et al. The prognostic value of F-18 fluorodeoxyglucose bone marrow uptake in patients with recent diagnosis of multiple myeloma: a comparative study with Tc-99m sestamibi. Clin Nucl Med 2010;35:1–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haznedar, R., Akı, S.Z., Akdemir, Ö.U. et al. Value of 18F-fluorodeoxyglucose uptake in positron emission tomography/computed tomography in predicting survival in multiple myeloma. Eur J Nucl Med Mol Imaging 38, 1046–1053 (2011). https://doi.org/10.1007/s00259-011-1738-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1738-8