Abstract
Purpose
The purpose of this prospective study was to determine the diagnostic impact and influence on patient treatment of posttherapeutic 131I SPECT-CT when the findings on planar posttherapeutic whole-body scintigraphy (ptWBS) were inconclusive.
Materials and methods
A total of 53 SPECT-CT scans were performed in 41 patients with thyroid cancer after high-dose 131I therapy (2.944 to 7.526 GBq 131I) because of diagnostic uncertainty on ptWBS. Physiological uptake in the salivary glands, gastric mucosa, gut, nasal mucosa, urinary tract and liver were considered to be normal. Any other foci of increased 131I uptake, except iodine uptake clearly located in the thyroid bed, were considered to be abnormal. The data were evaluated on a lesion and a patient basis.
Results
Regarding neck lesions, SPECT-CT provided a diagnostic impact in 26/90 lesions (28.9%) and confirmed the diagnosis in 64/90 lesions (71.1%). On a patient basis, SPECT-CT changed N status in 12/33 patients (36.4%), provided a diagnostic impact in 21/33 patients (63.6%) and led to a treatment change in 8/33 patients (24.2%). Regarding lesions distant from the neck, SPECT-CT confirmed the diagnosis in 62/71 lesions (87.3%) and had a diagnostic impact in 9/71 lesions (12.7%). On a patient basis, SPECT-CT changed M status in 4/19 patients (21.1%), had a diagnostic impact in 14/19 patients (73.7%) and led to a treatment change in 2/19 patients (10.5%). Considering all patients, SPECT-CT led to a treatment change in 10/41 patients (24.4%).
Conclusion
Integrated SPECT-CT is a useful tool, especially in cases of diagnostic uncertainty and helps to individualize patient management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posttherapeutic whole-body scintigraphy (ptWBS) performed 5–7 days after administration of high activities of 131I in patients with differentiated thyroid cancer (DTC) is of great importance for judging the effectiveness of, and staging after, radioiodine therapy [1–9]. WBS is performed to localize 131I uptake and offers the opportunity to detect residual or recurrent disease as well as distant metastases often before visualization by conventional imaging is possible. The precise anatomical localization of foci with increased uptake and the determination of physiological or pathological iodine uptake is sometimes difficult on planar images because of the lack of anatomical landmarks and limited specificity [10–14]. WBS may reveal foci of 131I uptake owing to a variety of other causes, such as ectopic foci of normal thyroid tissue, nonthyroid physiological sites, due to contamination, ectopic gastric mucosa, gastrointestinal or urinary tract abnormalities, inflammation and infection, mammary abnormalities, nonthyroid neoplasms, serious cavities and cysts [10]. In particular, the diagnosis of iodine-positive lymph node metastases in the neck versus thyroid remnant, lung versus bone or mediastinal metastases is sometimes difficult [15–19]. Performing SPECT with side-by-side comparison to CT, MR and ultrasound images may be helpful in some cases. Software image fusion has proved helpful for anatomical localization of abnormalities detected on SPECT images in patients with DTC [15, 20]. However, this technique involves fusion of images acquired during two separate imaging sessions on two different scanners with the possibility of misregistration. With the availability of integrated SPECT-CT, a dual imaging modality, the combination of the scintigraphic functional data (SPECT) with the anatomic information (CT) in one single examination is possible. The possibility of combined imaging permits a high diagnostic accuracy by better recognition of pathological processes with exact anatomical localization [21–23, 16–19].
The purpose of this prospective study was to determine the diagnostic impact of 131I SPECT-CT with a low-dose CT component performed when the findings on conventional planar ptWBS after administration of high activities of 131I in patients with DTC are inconclusive. A further point was to investigate the clinical value of the better diagnostic accuracy and to evaluate the impact on, and possible changes in, the treatment and management of patients with thyroid cancer.
Materials and methods
In this prospective study 53 SPECT-CT scans were performed between November 2006 and April 2008 when the findings on conventional 131I ptWBS in DTC patients were inconclusive. A group of 41 patients (aged 25–86 years at time of therapy, mean age 60.6 years; 23 women, 18 men) underwent ptWBS 5 days after administration of 2.944 to 7.526 GBq 131I according to disease status. In 23 patients the iodine therapy was their first ablative therapy, and 18 had already undergone two or more iodine therapies (2–8 131I therapies, mean 3.96 therapies).
The histological types of the thyroid carcinoma were follicular (9 patients), follicular oxyphilic subtype (5), medullary–follicular (1), papillary (21), papillary follicular subtype (4), without classification (1) (Table 1).
During this period a total of 268 conventional ptWBS scans were performed in 234 patients in our institution. Because of inconclusive findings on the planar studies 53 SPECT-CT scans were performed (19.8%). Of the 215 ptWBS scans without SPECT-CT, 7 showed disseminated lung metastases, and in four patients the scan showed already diagnosed bone metastases. Therefore we decided that there was no need to perform SPECT-CT to evaluate the diagnostic impact. All the other ptWBS showed “clearly normal uptake” in thyroid remnants or a lobus pyramidalis.
Posttherapeutic 131I WBS was performed 5 days after 131I therapy. The acquisition was performed with the patient in the supine position as spot imaging in the anterior and posterior projections from the head and neck, thorax, abdomen and pelvis for 10 min per position using a dual-head gamma camera with a high-energy high-resolution collimator.
Because of inconclusive findings in the planar studies (interpreted by two experienced nuclear medicine specialists), SPECT-CT of the region of interest was performed on a dedicated scanner (Siemens Symbia T, Siemens Medical Systems) in order to evaluate areas of increased uptake. The CT scan of the region of interest (neck, thorax, and abdomen) was performed with the patient in the supine position with a low-dose protocol (25 mAs, 130 kV, pitch 1.5, 5-mm slice thickness, kernel B60s) without administration of contrast medium. SPECT was performed before CT, acquiring images at 30–55 s per view over 180°. The data were stored in a 128 × 128 matrix and iteratively reconstructed (OSEM Flash 3D, four subsets, eight iterations) using CT data for attenuation correction.
The ptWBS scans were interpreted by two experienced nuclear medicine physicians in consensus, and one of five experienced nuclear medicine physicians determined the need for performing SPECT-CT. In the interpretation of the scans physiologically symmetrical salivary gland uptake, gastric mucosa uptake, gut activity, nasal mucosal uptake, urinary tract excretion and liver uptake in those with a large residual thyroid tissue were considered to be normal. Any other foci of increased 131I uptake, except iodine uptake clearly located in the thyroid bed, were considered to be abnormal. The lesions on the planar ptWBS scan were classified as lesions in the neck and distant from the neck, and were interpreted by two nuclear medicine specialists in consensus.
SPECT-CT images were viewed and interpreted together with an experienced radiologist also in consensus. The SPECT-CT and WBS images were acquired on the same day and were interpreted independently from each other. The standard of reference for confirming the presence or absence of malignancy was either histopathology or clinical and imaging follow-up data.
Results
The results were evaluated on a lesional basis and on a patient basis.
Evaluation on a lesional basis in the neck
A total of 161 lesions were detected on planar images compared to 188 on SPECT-CT (+16.8%).
Regarding the lesions in the neck (Table 2), 90 were found on planar images and 95 on SPECT-CT (+5.6%). Of 11 equivocal lesions in the neck, 9 were diagnosed as benign by SPECT-CT (6 due to asymmetric uptake in the salivary glands, 1 due to periodontal surgery, 1 with asymmetric uptake due to sinusitis, and 1 due to a concretion in the parotid gland and parotitis), 1 was diagnosed as a lymph node metastasis, and 1 was diagnosed as a local recurrence. On SPECT-CT the diagnosis in 37 lesions seen on ptWBS was confirmed as remnant/local recurrence and 27 lesions as lymph node metastases in the neck. Nine lesions were diagnosed as remnant on SPECT-CT instead of lymph node metastases on ptWBS. Six lesions were diagnosed as lymph node metastases on SPECT-CT instead of remnant on ptWBS. Thus SPECT-CT was able to provide a diagnostic impact in 26/90 lesions (28.9%) and confirmed the diagnosis on ptWBS in 64/90 lesions (71.1%). Furthermore, three additional lymph node metastases and two local recurrences were diagnosed on SPECT-CT that were missed on ptWBS.
Evaluation on a lesional basis distant from the neck
Regarding the lesions distant from the neck (Table 2), 71 were detected on ptWBS and 93 on SPECT-CT (+31%). Of 62 lesions whose diagnosis was confirmed, 56 were confirmed as lung metastases on SPECT-CT, 3 as mediastinal metastases and 3 as bone metastases. Of four equivocal lesions, two were diagnosed as bone metastases and two as lymph node metastases (axillary and subpectoral lymph nodes). Three lesions were diagnosed as bone metastases instead of lung metastases and two were localized as mediastinal instead of lung metastases. In summary, on SPECT-CT confirmed the diagnosis in 62/71 lesions seen on ptWBS (87.3%) and had a diagnostic impact in 9/71 lesions (12.7%). Furthermore, 22 additional lesions were detected on SPECT-CT (17 lung metastases, 1 mediastinal metastasis, and 4 bone metastases). This phenomenon can be predominantly explained due to the accurately focused localization provided by SPECT especially in the field of lung metastases and by the possibility of localizing a faint iodine uptake with the morphological pathology visible on CT.
Evaluation on a patient basis in the neck
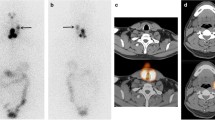
Uptake in the neck was evaluated in 33 patients on planar scintigraphy. On a patient-based analysis the additional information obtained from SPECT-CT led to an upstaging in N status in the neck in five patients who underwent ablative 131I therapy (Fig. 1). On the other hand, SPECT-CT led to a downstaging of N status in the neck in three patients because it excluded iodine-positive metastases that were diagnosed on planar scintigraphy (uptake due to remnants). In four patients additional iodine-negative metastases in the neck were diagnosed on SPECT-CT. In two patients cytologically proven lymph node metastases were present in the neck and after high-dose 131I therapy SPECT-CT clearly revealed iodine uptake in remnants and not in the metastases. In two patients enlarged, pathologically shaped lymph nodes were detected on SPECT-CT demonstrating no iodine uptake. All the iodine-negative lymph node metastases were histologically proven after complete neck dissection. In summary, SPECT-CT changed N status (N0/N1, N1/N0, iodine-negative lymph node metastases) in 12 of 33 patients (36.4%). SPECT-CT demonstrated additional diagnostic information in 21/33 patients with inconclusive findings in the neck (63.6%). The results obtained from SPECT-CT in the neck had a direct impact on the management of 8 of 33 patients (24.2%) in whom surgery was performed (6 patients with complete neck dissection, 2 for local recurrence), and due to precise anatomical information a detailed report of the pathologies could be given to the surgeons (Table 3).
Additional information obtained from SPECT-CT. a 131I ptWBS performed 5 days after 131I administration shows clear iodine uptake in the left neck and faint iodine uptake caudal and cranial. b SPECT-CT demonstrates 131I-positive lymph node metastases in the cervical region in the left neck. Because of the size of the lymph node metastases surgery was performed with precise anatomical information provided to the surgeons preoperatively
Evaluation on a patient basis distant from the neck
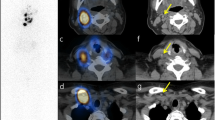
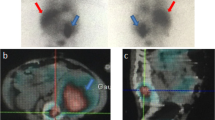
Uptake distant from the neck was evaluated in 19 patients on planar scintigraphy. Due to the anatomical mapping SPECT-CT was able to precisely localize the increased iodine uptake and led to an upstaging in M status in three patients (additional bone metastases in one patient, additional bone and pleural metastases in one patient and additional iodine-negative metastases) and to a change in M status in one patient (mediastinal versus bone metastasis; Fig. 2). Furthermore, in seven patients SPECT-CT revealed additional iodine-negative lung metastases (in six patients confirmed by PET-CT) indicating a worse outcome (Fig. 3). In seven patients a larger number of lung metastases were diagnosed on SPECT-CT compared to the planar ptWBS, therefore leading to a diagnostic impact, but not necessarily leading to an impact on patient management. The results obtained from SPECT-CT had a direct impact on the management in two patients, in whom external radiation therapy for stabilization of bone metastases was performed. In summary, SPECT-CT had an impact on M status (upstaging, change) in 4/19 patients (21.1%). A diagnostic impact in 14/19 patients (73.7%), and a direct impact on management with further action taken (external radiation therapy) in 2/19 patients (10.5%; Table 3).
Diagnostic impact of SPECT-CT. a 131I ptWBS 5 days after administration of high-dose iodine therapy with inconclusive findings in the thorax (iodine uptake due to mediastinal/lung or bone metastasis). b SPECT-CT demonstrates an iodine-positive bone metastasis in the 6th vertebral body of the thoracic spine. External radiation therapy was performed to avoid a pathological fracture. Another iodine-positive metastasis can be seen in the right supraclavicular region
Diagnostic impact of SPECT-CT. a 131I SPECT-CT performed 5 days after high-dose iodine administration demonstrates several iodine-positive lung metastases and also iodine-negative metastases visible on CT (arrows).b 18F-FDG PET-CT shows multiple FDG-positive metastases in the same patient due to dedifferentiation of the tumour cells, indicating a worse prognosis: flip-flop phenomenon
With regard to the impact on patient management overall (lesions in the neck and distant from the neck together), a direct consequential action was taken in 10/41 patients (24.4%).
Discussion
There is no doubt that the performance of ptWBS after administration of high-dose 131I therapy is of great value and a standard procedure in order to judge the effectiveness of therapy and for staging in DTC patients [1–9]. There are, however, a few limitations and difficulties in interpretation. On the one hand, normal thyroid remnants and residual or metastatic foci of DTC have the ability to store iodine and, on the other hand, ectopic thyroid tissue, nonthyroidal physiological sites, contamination, physiological excretion or abnormalities may cause foci of increased iodine uptake on the ptWBS scan that are difficult to interpret [10]. Bakheet and Hammami [11] reported cases of an ectopic kidney, chronic sinusitis, dacryocystitis and an artificial eye mimicking metastases on the posttherapy WBS scan. Thus they concluded that nonthyroidal pathology should be excluded before diagnosing iodine-positive metastases. Andreas et al. [12] reported a patient with follicular thyroid carcinoma who underwent ablative 131I therapy. Posttherapy WBS detected iodine accumulation in the area of the right occiput, suspicious for a metastasis; MRI however showed porencephaly in the right posterior calvarium mimicking a metastasis. Leitha and Staudenherz [14] concluded that the major clinical problems in posttherapy WBS include contamination, superimposed intestinal retention, hot nose, isolated peripheral metastasis, unexpected breast activity and kidney metastasis.
Software image fusion was introduced several years ago, and has proved to be helpful for anatomic localization of abnormalities detected on SPECT imaging. Yamamoto et al. [15] reported the clinical usefulness of the fusion of 131I SPECT and CT images in DTC using external markers for registration of anatomical and functional images. Fusion images were considered to be of benefit in 15 of 17 patients (88%). Cherng et al. [20] reported the rare case of a malignant struma ovarii with peritoneal implants and pelvic structures and liver metastases demonstrated by fusion of 131I SPECT and low-dose CT images. However, while very useful, this technique involves fusion of images acquired during two separate imaging sessions on two different scanners with the possibility of misregistration. There are a few case reports of 131I SPECT-CT in patients with DTC. Von Falck et al. [21] reported a patient with follicular DTC who developed renal metastases. The lesions were detected on SPECT-CT, and subsequent surgery and histopathological analysis of the renal lesion confirmed the diagnosis. Sakahara et al. [22] reported three patients with DTC in whom SPECT-CT visualized the nasolacrimal system after radioiodine therapy. Aide et al. [23] reported the accurate depiction of an unusual intratracheal metastasis of DTC by SPECT-CT after radioiodine ablation.
There are two main studies dealing with 131I posttherapy SPECT-CT. Ruf et al. [17] studied 25 DTC patients with inconclusive foci on planar scintigraphy after ablative radioiodine therapy. They concluded that the changed interpretation of 15/39 foci (38%) would have been relevant for therapy in the focus-based analysis. Also in the patient-based analysis the information was still therapeutically relevant in 6/24 patients (25%). Tharp et al. [18] also investigated the impact of 131I SPECT-CT images obtained with an integrated system in the follow-up of patients with thyroid carcinoma. They concluded that integrated 131I SPECT-CT had an additional value over planar imaging, SPECT-CT imaging had an incremental diagnostic value in 57% of patients (41/71).
In this prospective study we evaluated 53 SPECT-CT scans in 41 patients after high-dose iodine treatment, similar to the study by Ruf et al. [17]. Tharp et al. [18], however, also included 17 patients referred for diagnostic SPECT-CT. We applied a lesion-based analysis and a patient-based analysis to classify the inconclusive foci of increased iodine uptake in lesions in the neck and distant from the neck. The lesion-based analysis showed a diagnostic impact of SPECT-CT in the neck of 28.9%. Ruf et al. reported a change in interpretation in 38% of all foci together. Our patient-based analysis of the diagnostic impact of SPECT-CT in the neck proved to be helpful in the assessment of lymph node metastases. SPECT-CT changed the N status in 36.4% of patients (12/33). This would have a further impact for the patient as it leads to a change in risk stratification [24–31] or may lead to further treatment options, e.g. surgery. Altogether SPECT-CT yielded additional diagnostic information in 21/33 patients with inconclusive findings in the neck (63.6%). Tharp et al. demonstrated in their study a diagnostic value in 57% of patients not divided into separated regions.
In our study SPECT-CT in the neck had a direct impact on the management of 8/33 patients (24.2%). In these patients surgery was performed (six patients with completed neck dissection, two for local recurrence) and due the precise anatomical information a detailed report of the pathologies could be given to the surgeons. In the lesions distant from the neck SPECT-CT had an impact on M status (upstaging, change) in 4/19 patients (21.1%). A diagnostic impact was found in 14/19 patients (73.7%). This high percentage was partly influenced by the CT component, which was responsible for detection of iodine-negative metastases at an early stage of disease. SPECT-CT revealed seven patients with iodine-negative lung metastases (in six patients confirmed by PET-CT) indicating a worse prognosis. In addition in seven patients a larger number of lung metastases was diagnosed on SPECT-CT compared to the planar ptWBS, which had a diagnostic impact but not necessarily an impact on patient management. This phenomenon can be predominantly explained by the accurate focus localization on the SPECT especially in the field of lung metastases and by the possibility of localizing a faint iodine uptake with the morphological pathology visible by CT. SPECT-CT had a direct impact on management with further action taken (external radiation therapy) in 2/19 patients (10.5%).
With regard to the impact on patient management overall (lesions in the neck and distant from the neck together), a direct consequential action was taken in 10/41 patients (24.4%). This result is similar to the findings of Ruf et al. [17] who reported therapeutic relevance in 25% of patients (6/24) in a patient-based analysis.
Conclusion
Integrated 131I SPECT-CT provided valuable additional information especially in the assessment of lymph node metastases in the neck for precise localization versus remnant thyroid tissue and helped to optimize anatomical information for surgery. Valuable additional information from the precise localization was also obtained from SPECT-CT of the chest regarding size and number of metastases (lung versus mediastinal and bone metastases). Furthermore, iodine-negative metastases in the lung could be detected. SPECT-CT is a very useful tool, especially in cases of diagnostic uncertainty and helps to individualize the management of patients with DTC.
References
Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JWA, Wiersinga W; European Thyroid Cancer Taskforce. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 2006;154:787–803.
Fatourechi V, Hay ID, Mullan BP, Wiseman GA, Eghbali-Fatourechi GZ, Thorson LM, et al. Are posttherapy radioiodine scans informative and do they influence subsequent therapy of patients with differentiated thyroid cancer? Thyroid 2000;10:573–7.
Schlumberger M, Berg G, Cohen O, Duntas L, Jamar F, Jarzab B, et al. Follow-up of low risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol 2004;150:105–12.
Schlumberger M, Pacini F, Wiersinga WM, Toft A, Smit JW, Franco FS, et al. Follow-up and management of differentiated thyroid carcinoma: a European perspective in clinical practice. Eur J Endocrinol 2004;151:539–48.
Spies WG, Wojtowicz CH, Spies SM, Shah AY, Zimmer AM. Value of post-therapy whole-body imaging in the evaluation of patients with thyroid carcinoma having undergone high-dose I-131 therapy. Clin Nucl Med 1989;14:793–800.
Cavalieri RR. Nuclear imaging in the management of thyroid carcinoma. Thyroid 1996;6:485–92.
Sherman SI, Tielens ET, Sostre S, Wharam MD Jr, Ladenson PW. Clinical utility of posttreatment radioiodine scans in the management of patients with thyroid carcinoma. J Clin Endocrinol Metab 1994;78:629–34.
Pacini F, Schlumberger M, Harmer C, Berg GG, Cohen O, Duntas L, et al. Post-surgical use of radioiodine (131 I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation: a consensus report. Eur J Endocrinol 2005;153:651–9.
Lind P, Kohlfürst S. Respective roles of thyroglobulin, radioiodine imaging, and positron emission tomography in the assessment of thyroid cancer. Semin Nucl Med 2006;36:194–205.
Shapiro B, Rufini V, Jarwan A. Artifacts, anatomical and physiological variants, and unrelated diseases that might cause false-positive whole-body 131 I scans in patients with thyroid cancer. Semin Nucl Med 2000;30:115–32.
Bakheet SM, Hammami MM. False positive radioiodine whole-body scan in thyroid cancer patients due to unrelated pathology. Clin Nucl Med 1994;19:325–9.
Andreas J, Bruhl K, Eissner D. False-positive I-131 whole-body imaging after I-131 therapy for a follicular carcinoma. Clin Nucl Med 1997;22:123–4.
Sherman SI, Tielens ET, Sostre S, Wharam MD Jr, Ladenson PW. Clinical utility of posttreatment radioiodine scans in the management of patients with thyroid carcinoma. J Clin Endocrinol Metab 1994;78:629–34.
Leitha T, Staudenherz A. Frequency of diagnostic dilemmas in 131 I whole body scanning. Nuklearmedizin 2003;42:55–62.
Yamamoto Y, Nishiyama Y, Monden T, Matsumura Y, Satoh K, Ohkawa M. Clinical usefulness of fusion of 131I SPECT and CT images in patients with differentiated thyroid carcinoma. J Nucl Med 2003;44:1905–10.
Krausz Y, Klein M, Uziely B, et al. Impact of SPECT/CT on assessment of 131 I-avid sites in differentiated thyroid cancer (abstract). J Nucl Med 2004;45:349.
Ruf J, Lehmkuhl L, Bertram H, Sandrock D, Amthauer H, Humplik B, et al. Impact of SPECT and integrated low-dose CT after radioiodine therapy on the management of patients with thyroid carcinoma. Nucl Med Commun 2004;25:1177–82.
Tharp K, Israel O, Hausmann J, Bettman L, Martin WH, Daitzchman M, et al. Impact of 131I-SPECT/CT images obtained with an integrated system in the follow-up of patients with thyroid carcinoma. Eur J Nucl Med Mol Imaging 2004;31:1435–42.
Krausz Y, Israel O. Single-photon emission computed tomography/computed tomography in endocrinology. Semin Nucl Med 2006;36:267–74.
Cherng SC, Wang YF, Fan YM, Chen CY, Yuan YN, Cheng CY. Malignant struma ovarii with peritoneal implants and pelvic structures and liver metastases demonstrated by I-131 SPECT and low-dose CT. Clin Nucl Med 2005;30:797–8.
von Falck C, Beer G, Gratz KF, Galanski M. Renal metastases from follicular thyroid cancer on SPECT/CT. Clin Nucl Med 2007;32:751–2.
Sakahara H, Yamashita S, Suzuki K, Imai M, Kosugi T. Visualization of nasolacrimal drainage system after radioiodine therapy in patients with thyroid cancer. Ann Nucl Med 2007;21:525–7.
Aide N, Lehembre E, Gervais R, Bardet S. Unusual intratracheal metastasis of differentiated thyroid cancer accurately depicted by SPECT/CT acquisition after radioiodine ablation. Thyroid 2007;17:1305–6.
Mazzaferri EL, Jiang SM. Long term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 1994;49:418–28.
Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at an institution during 1940 through 1989. Surgery 1993;114:1050–7.
Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1990): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 2002;8:879–85.
Byar DP, Green SB, Dor P, Williams ED, Colon J, van Gilse HA, et al. A prognostic index for thyroid carcinoma. A study of the E.O.R.T.C. Thyroid Cancer Cooperative Group. Eur J Cancer 1979;15:1033–41.
Tenvall J, Biorklund A, Moller T, Ranstam J, Akerman M. Is the EORTC prognostic index of thyroid cancer valid in differentiated thyroid carcinoma? Retrospective multivariate analysis of differentiated thyroid carcinoma with long follow-up. Cancer 1986;57:1405–14.
Shaha AR, Loree TR, Shah JP. Prognostic factors and risk group analysis in follicular carcinoma of the thyroid. Surgery 1995;118:1131–6.
Sherman SI, Brierly JD, Sperling M, Ain KB, Bigos ST, Cooper DS, et al. Prospective multicenter study of thyroid cancer treatment: initial analysis of staging and outcome. National Thyroid Cancer Treatment Study Registry Group. Cancer 1998;83:1012–21.
Links TP, van Tol KM, Jager PL, Plukker JT, Piers DA, Boezen HM, et al. Life expectancy in differentiated thyroid cancer: a novel approach to survival analysis. Endocr Relat Cancer 2005;12:273–80.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kohlfuerst, S., Igerc, I., Lobnig, M. et al. Posttherapeutic 131I SPECT-CT offers high diagnostic accuracy when the findings on conventional planar imaging are inconclusive and allows a tailored patient treatment regimen. Eur J Nucl Med Mol Imaging 36, 886–893 (2009). https://doi.org/10.1007/s00259-008-1044-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-1044-2