Abstract
Purpose
In clinical routine somatostatin analogue positron emission tomography/computed tomography (PET/CT) such as 68Ga-DOTA-Tyr-octreotide (DOTATOC)-PET/CT could substitute conventional 111In-Octreotide scintigraphy. Immunohistochemistry (IHC) for somatostatin receptor 2 (SSTR2) might be a tool to predict positivity of 68Ga-DOTATOC in patients where initial staging was not performed, e.g., in incidental findings. We therefore compared a score of SSTR2-IHC with the in vivo standard uptake value (SUV) of preoperative or prebiopsy 68Ga-DOTATOC PET/CT.
Materials and methods
In 18 patients, 68Ga-DOTATOC PET/CT scans were quantified with SUV calculations and correlated to a cell membrane-based SSTR2-IHC score (ranging from 0 to 3).
Results
Negative IHC scores were consistent with SUV values below 10. Furthermore, all score 2 and 3 specimens corresponded with high SUV values (above 15).
Conclusion
SSTR2-IHC scores correlated well with SUV values and we propose to use SSTR2 immunohistochemistry in patients missing a preoperative PET scan to indicate 68Ga-DOTATOC-PET/CT as method for restaging and follow-up in individual patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although neuroendocrine tumours are generally slow progressing, in case of metastatic spread, therapeutic options are limited, and cure rates are low. For clinical management, somatostatin receptor (SSTR) scintigraphy such as 111In-Octreotide scintigraphy has become obligatory in staging and restaging of most patients. It allows sensitive localisation of tumour manifestations, accurate follow-up and will select patients eligible for somatostatin receptor radiotherapy [1–3]. With availability of somatostatin analogues suitable as positron emission tomography (PET) tracers, improved sensitivity and the advantage of comparable quantification has been suggested. Many of the available PET tracers are utilizing the generator-derived positron emitter 68Ga and display higher affinities to the somatostatin receptor 2 than conventionally used 111In-DTPA-octreotide (Octreoscan). For example, 68Ga-DOTA-Tyr-octreotide (DOTATOC) displays a very high SSTR2 receptor binding with an inhibitory concentration 50% (IC50, with 123I-Tyr-octreotide as radioligand) of 2.5 nmol/L in comparison to 22 nmol/L of 111In-DTPA-octreotide [4, 5]. Additionally, with significant shorter study times and increasing availability of hybrid technology including computed tomography (CT), PET has the potential of substituting conventional 111In-DTPA-octreotide scintigraphy and single photon emission tomography (SPECT) when available [6]. Direct comparison already showed an increased diagnostic effectiveness of 68Ga-DOTATOC PET over 111In-DTPA-octreotide SPECT [7].
The indication of SSTR imaging for restaging and follow-up is based on a preoperative scan proving the expression of the SSTR2. However, the neuroendocrine phenotype of tumours is frequently detected only after surgery by histopathological analysis of the resection specimen. In this clinical setting, the use of SSTR imaging for restaging is uncertain, as a baseline scan is not available, and the tumour might not sufficiently express somatostatin receptors. Immunohistochemistry is able to detect SSTR2 on tumour specimens. In one retrospective study, immunohistochemical analysis of SSTR2 showed a 77% concordance when compared to 111In-DTPA-octreotide scintigraphy [8]. Translation of these findings to PET using a somatostatin analogue as PET tracer is likely to be feasible; however, 68Ga-DOTATOC binds more specifically to SSTR2, and therefore, the correlation might even be better. We therefore correlated a semiquantitative SSTR2 scoring of immunohistochemistry with the standardised uptake value calculated from 68Ga-DOTATOC PET/CT scans performed in a retrospective series of 17 patients with neuroendocrine tumours and one thymoma patient.
Materials and methods
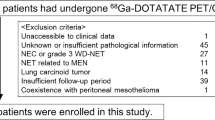
In 18 patients (mean age 53 years, eight female, ten male) with available tumour specimens and 68Ga-DOTATOC PET/CT scans, specific 68Ga-DOTATOC uptake in tumour lesions was quantified by calculation of standardized uptake values (SUV). PET/CT scans were acquired on a Siemens Biograph 16 at 20 min after application of approximately 120 MBq of 68Ga-DOTATOC (mean 112 MBq, SD 15 MBq). Seven or eight bed positions with 4 min emission time were acquired. PET images were reconstructed using CT attenuation correction (OSEM). SUV calculations were performed on a Siemens Syngo workstation, and mean and maximum SUV (activity concentration corrected for patient weight and total injected dose) were determined using individual 50% of maximum isocontours in tumour lesions. Histopathologic specimens from either operation (14 patients) or biopsy (four patients) were formalin fixed and embedded in paraffin according to standard procedures. Thin paraffin sections, 4 µm, were immunostained after deparaffinisation and protease-based antigen retrieval (6 min, Benchmark, Ventana) with antibodies against SSTR2 (1:600; Gramsch laboratories, Schwabhausen, Germany) on an automated immunostainer (Benchmark, Ventana) using the ABC method. For semiquantitative analysis of the SSTR2 staining, a four-tiered grading system (Fig. 1) was used in analogy to the DAKO-score for her2-neu: 0 (negative), 1+ (weak partial membrane positivity), 2+ (intermediate complete membrane positivity) and 3+ (strong complete membrane positivity). According to this system, only membranous (not cytoplasmic) staining was scored. Two investigators (A.P., S.S.) performed the analysis independently, blinded to the SUV values. Statistical analysis [one-way analysis of variance (ANOVA)] was done with GraphPad Prism 3.0.
Results
The patients included had the following tumours: 11 neuroendocrine carcinomas (NEC) of the digestive tract, two metastasised medullary thyroid carcinomas, one pulmonary carcinoid, one NEC each of the thoracic wall and the bladder and a primary presacral neuroendocrine carcinoma (probably arising in a tailgut cyst), as well as one thymoma (Table 1). Semiquantitative scoring of the SSTR2 immunohistochemistry revealed five tumours with score 0, four tumours with score 1, two tumours with score 2 and seven tumours with score 3. Of the five histopathologically SSTR2-negative tumours, all had low mean standard uptake values on 68Ga-DOTATOC PET ranging from 1.8 in the thymoma to 6.2 in liver metastases of a grade 3 coecal NEC (Fig. 2). However, all these tumours were still visible on the PET images. For all SSTR2-positive tumours (score 1–3), SUV values were significantly higher, except for a NEC of the bladder with score 1 at immunohistochemistry and a measured mean SUV of 5.9. A correlation between pathological score and SUV was evident (Fig. 3) and one-way ANOVA showed significant differences between the SUV (mean and max) for the different pathological scores (P < 0.05) and a linear trend (P < 0.05) in posttest analysis. Two tumours with strong cytoplasmic and weak membranous immunopositivity both showed a weak SUV confirming the approach to only score membranous positivity. A correlation of SUV with the proliferation index (Ki67) showed that the four grade 3 NECs were only partly associated with low SUV values. However, no clear correlation between SUV and proliferation index was evident (Fig. 4).
Coronal 68Ga-DOTATOC PET images of tumour lesions (upper row: low uptake, middle and lower row: high uptake). a Lymph node metastasis of a medullary thyroid carcinoma (SUV mean = 5, IHC score = 0); b NEC of the thoracic wall (SUV mean = 4, IHC score = 0); c pulmonary carcinoid (SUV mean = 9, IHC score = 1); d liver metastasis of a NEC of the ileum (SUV mean = 19, IHC score = 2); e primary presacral NEC (SUV mean = 31, IHC score = 3); f NEC of the pancreas (SUV mean = 48, IHC score = 3)
Discussion
We show that positive somatostatin receptor-2 immunostaining correlates with 68Ga-DOTATOC PET positivity. While SSTR2 immunonegative tumours could not be visualized in 111In-DTPA-octreotide scans [9], we demonstrate evidence that they can still be visualized when somatostatin analogue PET is performed. However, negative membranous SSTR2 immunhistochemistry is associated with a low mean standardised uptake value (approximately 5) and a low maximum SUV (below 10) in these lesions (this might represent weak binding to somatostatin receptor 5). Therefore, we propose to include SUV measurements into the interpretation of 68Ga-DOTATOC PET studies. In an earlier immunohistochemical study, grouping of scores 0 and 1 as negative lead to best concordance with 111In-DTPA-octreotide scintigraphy [9]. In the present comparison with 68Ga-DOTATOC PET also, two of the four specimens displaying a immunohistochemical score of 1 showed very intense uptake. This result might be explained by the higher affinity of 68Ga-DOTATOC to SSTR2. As the number of score 1 tumours is small, further data are needed to clarify this issue. Of note, all tumours exhibiting an immunohistochemical SSTR2 score 2 and 3 showed high SUV (above 15). This correlation of immunohistochemical SSTR2 expression with 68Ga-DOTATOC PET has implications: In patients where the compulsory initial (preoperative) somatostatin receptor imaging was not performed because of the unknown neuroendocrine tumour phenotype, a strong SSTR2 immunohistochemistry (score 2/3) makes 68Ga-DOTATOC PET the imaging method of choice for restaging and follow-up. In this setting, SSTR2 immunohistochemistry might therefore be the best substitute for a positive preoperative somatostatin receptor imaging. Additionally, the correlation of the pathological score with 68Ga-DOTATOC accumulation provides evidence that SSTR2 immunohistochemistry could assist in identifying patients appropriate for further diagnostic workup potentially leading to somatostatin receptor radiotherapy. Alternatively, somatostatin receptor autoradiography would allow a receptor subtype quantification and is therefore superior to immunohistochemistry. However, this method is not widely available and needs fresh frozen tissue. Immunohistochemistry has the advantage to be feasible on formalin-fixed paraffin-embedded tissue, which is always available. One 1.4 cm lymph node metastasis of a gastrinoma with a tracer accumulation in the medium range showed an immunohistochemical score 3. In such small lesions (below 2.5 cm), a partial volume effect of the PET leading to low SUVs should be considered [10]. On the other hand, one large liver metastasis from a rectal NEC with intermediate tracer uptake displayed a pathological score of 1. This might be explained by heterogeneity of tumour tissue with regard to SSTR2 expression.
Conclusion
In neuroendocrine tumours, we detected a significant correlation of membranous SSTR2 expression as determined by immunohistochemistry and tumour uptake of the SSTR2 analogue 68Ga-DOTATOC as determined by PET and calculation of standardised uptake values. Therefore, we propose to use SSTR2 immunohistochemistry in patients missing a preoperative PET scan to indicate 68Ga-DOTATOC PET/CT as method of choice for restaging and follow-up in individual patients.
References
Krenning EP, Valkema R, Kwekkeboom DJ, de Herder WW, van Eijck CH, de Jong M, Pauwels S, Reubi JC. Molecular imaging as in vivo molecular pathology for gastroenteropancreatic neuroendocrine tumors: implications for follow-up after therapy. J Nucl Med 2005;46(Suppl 1):76S–82S.
Kwekkeboom DJ, Krenning EP. Radiolabeled somatostatin analog scintigraphy in oncology and immune diseases: an overview. Eur Radiol 1997;7(7):1103–9.
van der Lely AJ, de Herder WW, Krenning EP, Kwekkeboom DJ. Octreoscan radioreceptor imaging. Endocrine 2003;20(3):307–11.
Antunes P, Ginj M, Zhang H, Waser B, Baum RP, Reubi JC, Maecke H. Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging 2007;34(7):982–93.
Reubi JC, Schar JC, Waser B, Wenger S, Heppeler A, Schmitt JS, Macke HR. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med 2000;27(3):273–82.
Steinmuller T, Kianmanesh R, Falconi M, Scarpa A, Taal B, Kwekkeboom DJ, Lopes JM, Perren A, Nikou G, Yao J. Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2008;87(1):47–62.
Buchmann I, Henze M, Engelbrecht S, Eisenhut M, Runz A, Schafer M, Schilling T, Haufe S, Herrmann T, Haberkorn U. Comparison of 68Ga-DOTATOC PET and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2007;34(10):1617–26.
Volante M, Brizzi MP, Faggiano A, La Rosa S, Rapa I, Ferrero A, Mansueto G, Righi L, Garancini S, Capella C. Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol 2007;20(11):1172–82.
Asnacios A, Courbon F, Rochaix P, Bauvin E, Cances-Lauwers V, Susini C, Schulz S, Boneu A, Guimbaud R, Buscail L. Indium-111-pentetreotide scintigraphy and somatostatin receptor subtype 2 expression: new prognostic factors for malignant well-differentiated endocrine tumors. J Clin Oncol 2008;26(6):963–70.
Wieder H, Beer AJ, Poethko T, Meisetschlaeger G, Wester HJ, Rummeny E, Schwaiger M, Stahl AR. PET/CT with Gluc-Lys-([(18)F]FP)-TOCA: correlation between uptake, size and arterial perfusion in somatostatin receptor positive lesions. Eur J Nucl Med Mol Imaging 2008;35(2):264–71.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miederer, M., Seidl, S., Buck, A. et al. Correlation of immunohistopathological expression of somatostatin receptor 2 with standardised uptake values in 68Ga-DOTATOC PET/CT. Eur J Nucl Med Mol Imaging 36, 48–52 (2009). https://doi.org/10.1007/s00259-008-0944-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-0944-5