Abstract
Purpose
We tested the hypothesis that increased abdominal visceral accumulation (VFA) is associated with insulin resistance and cardiovascular autonomic dysfunction in type 2 diabetic patients not receiving insulin treatment.
Methods
The fat distribution was evaluated by measuring the VFA by abdominal computed tomography at the umbilical level. The study group consisted of 24 type 2 diabetic patients with high VFA (≥100 cm2, age 60 ± 8 years, high VFA group). The control group consisted of 19 age-matched type 2 diabetic patients with normal VFA (<100 cm2, age 60 ± 7 years, normal VFA group). Cardiovascular autonomic function was assessed by baroreflex sensitivity, heart rate variability, plasma norepinephrine concentrations, and cardiac 123I-metaiodobenzylguanidine (MIBG) scintigraphy.
Results
Early and delayed 123I-MIBG myocardial uptake values were lower (p < 0.005 and p < 0.0001, respectively) and the percent washout rate of 123I-MIBG was higher (p < 0.0005) in the high VFA group than in the normal VFA group. The fasting plasma insulin concentrations (p < 0.005) and the homeostasis model assessment (HOMA) index values (p < 0.0005) were higher in the high VFA group than in normal VFA group. Multiple regression analysis revealed that the level of VFA was independently predicted by the HOMA index values and the myocardial uptake of 123I-MIBG during the delayed phase.
Conclusion
Our results demonstrate that the level of VFA is associated with depressed cardiovascular autonomic function and insulin resistance in patients with type 2 diabetes mellitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A central pattern of body fat distribution, rather than regional or generalized obesity, is now generally considered to play an important role in the metabolic syndrome, which involves insulin resistance, hyperinsulinemia, dyslipidemia, obesity, diabetes mellitus, and hypertension [1–4].
An increased visceral fat accumulation (VFA) is a risk factor for cardiovascular disease [5, 6] and is associated with insulin resistance in healthy subjects [7] and type 2 diabetic patients [8]. Also, impaired autonomic neural activity has been recognized as a crucial risk factor of cardiac dysfunction and is strongly associated with an increased risk for harmful events and overall mortality in diabetic patients [9, 10]. Recently, we have reported that depressed cardiovascular autonomic function is related to insulin resistance in type 2 diabetic patients [11–13]. However, the relationship among VFA levels, insulin resistance, and cardiac autonomic dysfunction has not been adequately investigated.
Cardiac autonomic function has been assessed by measurements of baroreflex sensitivity (BRS), heart rate variability (HRV), and the concentration of norepinephrine, but the reliability coefficients of these parameters have been shown to be around 50% [14]. A reduction in myocardial uptake of 123I-metaiodobenzylguanidine (MIBG) reflects a reduction in the concentration of norepinephrine at presynaptic sites or a reduction in the neural density, whereas an enhanced washout rate of 123I-MIBG reflects enhanced release of norepinephrine from presynaptic sites [15].
Recent technical advances such as 123I-MIBG scintigraphy allow cardiac autonomic function to be assessed more precisely [16, 17]. For the analysis, furthermore, VFA measured through computed tomography (CT) has been used [18].
We hypothesized that increased VFA is associated with cardiovascular autonomic dysfunction and insulin resistance in type 2 diabetic patients. To test our hypothesis, we compared BRS, HRV, plasma norepinephrine concentrations, and cardiac 123I-MIBG scintigraphy in addition to the metabolic profiles of Japanese type 2 diabetic patients with normal VFA and those with high VFA, and independent predictors of the level of VFA in these populations were evaluated.
Materials and methods
We screened 105 consecutive Japanese patients with type 2 diabetes mellitus who were admitted to our department between January 2005 and May 2006. Among these subjects, we enrolled 65 patients who did not have organic heart disease as determined by physical examinations, chest X-rays, 12-lead electrocardiography (ECG), echocardiography, treadmill exercise ECG, and 201Tl cardiac scintigraphy. All patients underwent clinical examinations to exclude the presence of secondary hypertension. Essential hypertension was defined as diastolic blood pressure ≥90 mmHg, systolic blood pressure ≥140 mmHg, or self-reported use of antihypertensive medication [19].
Blood was taken at 7:00 a.m. from the antecubital vein with the patient in the recumbent position after an overnight fast. All patients underwent routine laboratory tests including assays for serum electrolytes, serum total cholesterol, serum triglycerides, serum high-density lipoprotein, fasting plasma glucose, and fasting immunoreactive insulin. Insulin resistance was evaluated by the homeostasis model assessment (HOMA) index: [fasting plasma insulin (μU/ml) × fasting plasma glucose (mmol/l)]/22.5 [20].
All subjects underwent CT at the level of the umbilicus to measure cross-sectional abdominal visceral fat areas; the scans were analyzed with Fat scan version 3 software (N2 Systems, LT, Osaka, Japan). Details of the procedures have been described previously [21]. This method has been validated by other determinations of VFA [22] and widely adopted as a practical method to evaluate regional adiposity.
Twenty-four patients were determined to have high VFA (≥100 cm2; high VFA group). We also included 19 age-matched patients from the original 65 enrolled patients who had normal VFA (<100 cm2; normal VFA group), the classification of which has previously been validated [23]. The clinical characteristics of patients in the normal and high VFA groups are summarized in Table 1. Sixteen of the 24 patients in the high VFA group and 12 of the 19 patients in the normal VFA group met the criteria for essential hypertension and all of these patients were being treated with calcium channel antagonists, angiotensin-converting enzyme inhibitors, and/or angiotensin II receptor blockers with diuretics. None of the patients was being treated with beta-blockers or insulin. Dyslipidemia was defined as a fasting triglycerides level ≥200 mg/dl or an HDL-cholesterol concentration <45 mg/dl for women and <35 mg/dl for men [19]. Eight of the 24 patients in the high VFA group and six of the 19 patients in the normal VFA group met the criteria for dyslipidemia. Patients with abnormal plasma creatinine concentrations (≥1.5 mg/dl) were excluded from the study.
All subjects gave their written informed consent to participation in the study, and the study protocol was approved by the ethics committee of the Oita University Hospital.
Echocardiography
M-mode and two-dimensional echocardiography and cardiac Doppler recordings were obtained using a phase-array echo-Doppler system. Echocardiograms were obtained using standard parasternal, short axis, and apical views. The left ventricular mass was calculated as: \(1.04 \times {\left( {{\left[ {{\text{LVIDd}} + {\text{IVSTd}} + {\text{PWTd}}} \right]}^{3} - {\text{LVIDd}}^{3} } \right)} - 14\,{\text{g,}}\) where LVIDd is the left ventricular internal diameter at end-diastole, IVSTd is the interventricular septal thickness at end-diastole, and PWTd is the posterior wall thickness at end-diastole. The left ventricular mass was divided by the body surface accumulation to calculate the left ventricular mass index. Pulsed Doppler recordings were made from a standard apical four-chamber view. Mitral inflow velocity was recorded with the sample volume at the mitral annulus level taking the average from at least three cardiac cycles. The peak velocity of early (E) and late ventricular filling (A) was determined, and the ratio (E/A) and deceleration time were recorded.
Cardiovascular autonomic function tests
Autonomic function was assessed according to methods described in previous studies [10–12]. During the tests, which were performed between 9:00 and 11:00 a.m., all subjects were in the supine position in a quiet room with dimmed lights. Autonomic function tests were performed in the morning after an overnight (≥12 h) fast. A blood sample was obtained from a venous catheter for measurement of the plasma norepinephrine concentration. The catheter was inserted in the right cubital vein, and arterial blood pressure was recorded noninvasively through a tonometric sensor (Jentow-7700; Nihon Colin, Komaki, Japan) attached over the left radial artery. The accuracy of continuous blood pressure monitoring has been demonstrated previously [24]. Arterial blood pressure and a standard 12-lead ECG were monitored simultaneously; data were stored in a PCM data recorder (RD-200T; TEAC, Tokyo). Three-lead precordial Holter ECG recordings (model-459; Del Mar Avionics, Irvine, CA) were also obtained throughout the procedure for analysis of HRV.
After an interval of 30 min to permit stabilization of the cardiovascular baroreflex mechanism, the patient was asked to breathe at a rate of 15 breaths/min using a metronome to stabilize the relationship between respiration and cardiovascular function. BRS was assessed by the phenylephrine method. Briefly, phenylephrine (2–3 μg/kg) was injected for 15 s to obtain a 15- 40-mmHg rise in systolic blood pressure. BRS was calculated as the slope of the linear regression function relating systolic blood pressure changes to changes in the RR interval. Regression lines with more than 20 data points and a correlation coefficient (r) greater than 0.8 were accepted for analysis. The average of the two slopes was taken as the BRS value.
HRV was analyzed using Holter ECG recordings (Marquette Electronics Inc., Milwaukee, WI, USA). The power spectrum of the RR interval was computed by a fast Fourier transformation and expressed as the accumulation under the power spectrum. We calculated the power of two spectral bands: the normal frequency (LF) component at 0.04–0.15 Hz and the high-frequency (HF) component at 0.15–0.40 Hz. Based on their skewed distribution, the measured values of HRV were transformed to natural logarithmic values. The ratio of LF to HF (LF/HF) was also computed.
Planar and single-photon emission computed tomography studies were performed 15 min (early) and 4 h (delayed) after the injection of 111 MBq of 123I-MIBG using a rotating gamma camera (ZLC 7500; Siemens, Munich, Germany). Data were analyzed with analysis software (SCINTIPAC; Shimadzu, Kyoto, Japan). The anterior planar images from early and delayed 123I-MIBG studies were analyzed visually. For semiquantitative analysis, regions of interest were identified within the whole heart and a 10 × 10 mm accumulation over the upper mediastinum on the early and delayed planar images was used to calculate the mean heart-to-mediastinum (H/M) ratio. After correcting for the physical decay of 123I, the percent washout rate (WR) of the tracer from the myocardium was determined over a 4-h period.
Anthropometric and body composition measurements
The anthropometric and body composition characteristics of the patients were evaluated using the following parameters: height, body weight, body mass index (BMI), waist circumference, hip circumference, and waist-to-hip ratio. BMI was calculated as weight/(height2) (kg/m2). The waist circumference was measured midway between the lower rib margin and the iliac crest, and the hip circumference was measured at the widest circumference over the trochanter in standing subjects after normal expiration.
Statistical analysis
Data are presented as means±SD. Differences between two groups were analyzed with the unpaired Student’s t test, chi-square test, or Fisher’s exact probability test. A p value <0.05 was considered statistically significant. Simple (Spearman’s rank) correlation coefficients between VFA and various parameters were calculated. Stepwise multiple regression analysis was then used to evaluate the association between the levels of VFA and other factors, such as the BMI, waist circumference, waist-to-hip ratio, E/A ratio, triglyceride levels, HDL-cholesterol levels, uric acid levels, fasting plasma glucose, and plasma insulin concentrations, HOMA index values, urinary albumin excretion, BRS, the percent WR of 123I-MIBG, and the H/M ratio during the early and delayed phase after 123I-MIBG administration. In our multivariate analysis, F values ≥4 were considered significant.
Results
As shown in Table 1, the mean ages of the high and normal VFA groups were similar, and there were no significant differences between the groups with respect to gender, duration of diabetes, or administered medications. The BMI values, waist circumferences, and waist-to-hip ratios were larger in the high VFA group than in the normal VFA group (p = 0.0385, p = 0.0015, and p = 0.0389, respectively). Regarding glucose metabolism, fasting plasma glucose and insulin concentrations and HOMA index values were higher in the high VFA group than in the normal VFA group (p = 0.0379, p = 0.0011, and p = 0.0003, respectively). There was, however, no significant difference in the levels of hemoglobin A1c. With regard to lipid metabolism, the concentration of serum triglyceride was higher and the concentration of serum HDL-cholesterol was lower in the high VFA group than in the normal VFA group (p = 0.0490 and p = 0.0256, respectively), whereas serum total cholesterol levels were not significantly different between the groups. The concentration of uric acid was higher in the high VFA group than in the normal VFA group (p = 0.0116). Renal function tests showed no significant difference in serum concentration between the two groups. The hemodynamic data listed in Table 1 were obtained immediately before BRS assessment. The resting heart rate and the systolic and diastolic blood pressures were not significantly different between the two groups.
Table 2 presents a summary of the echocardiographic findings. The left ventricular dimensions at end-diastole and end-systole, the intraventricular septal and posterior wall thicknesses at end-diastole, the ejection fraction, and the left ventricular mass index values were similar in the two groups. With regard to left ventricular diastolic function, the peak velocity of late ventricular filling (A) was higher and the E/A ratio was lower in the high VFA group compared with the normal VFA group (p = 0.0136 and p = 0.0060, respectively). The deceleration time was longer in the high VFA group than in the normal VFA group (p = 0.0102).
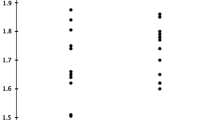
Figure 1 summarizes the results of the cardiovascular autonomic function tests. The BRS was lower in the high VFA group than in the normal VFA group (high VFA group, 8.4 ± 4.2 vs normal VFA group, 12.0 ± 5.1 ms/mmHg, p = 0.0141; Fig. 1a). The plasma norepinephrine concentration was similar in both groups (high VFA group, 242 ± 83 pg/ml; normal VFA group, 207 ± 65 pg/ml; p=ns; Fig. 1b). Furthermore, analysis of HRV in the high and normal VFA groups revealed that the HF power (3.4 ± 1.0 and 3.9 ± 1.2 ln-ms2, respectively; p=ns) and the LF/HF ratios (1.2 ± 0.7 and 1.4 ± 1.1, respectively; p=ns, Fig. 1c) were not significantly different between the two groups. Cardiac 123I-MIBG scintigraphy disclosed that the H/M ratios at early and delayed phases in the high VFA group were significantly smaller than those in the normal VFA group (early phase: 2.03 ± 0.15 vs 2.25 ± 0.27, respectively; p = 0.0021; delayed phase: 1.88 ± 0.18 vs 2.20 ± 0.21, respectively, p < 0.0001; Fig. 1d). The percent WR of 123I-MIBG was higher in the high VFA group than in the normal VFA group (44.8 ± 8.5% vs 35.7 ± 7.6%, p = 0.0005; Fig. 1d).
Comparison of autonomic function tests of type 2 diabetes mellitus patients with normal visceral fat accumulation (normal VFA) or high visceral fat accumulation (high VFA). a Baroreflex sensitivity (BRS). b Plasma norepinephrine (NE) concentration. c Heart rate variability (HRV). Power of the high-frequency component (HF, 0.15–0.40 Hz; a) and the ratio of the low-frequency power (LF; 0.04 to 0.15 Hz) to HF power (LF/HF, b). The distribution of HRV values was skewed and the values were thus transformed to natural logarithmic values. d Cardiac 123I-MIBG scintigraphic findings. Myocardial uptake of 123I-MIBG during the early (a) and delayed (b) phases. Myocardial uptake of 123I-MIBG is expressed as the mean heart-to-mediastinum (H/M) ratio. c Percent washout rate (WR) of 123I-MIBG. Data are mean±SD. ns not significant
Table 3 depicts the correlation between the VFA level and age, the body mass index, and other variables in both the high and the normal VFA group. The VFA levels were positively correlated with body mass index values, waist circumference, waist-to-hip ratio, triglyceride levels, uric acid levels, fasting plasma glucose and insulin concentration, HOMA index values, urinary albumin excretion, and percent WR of 123I-MIBG, and were negatively correlated with HDL-cholesterol levels, BRS, the E/A ratio, and the H/M ratio during the early and the delayed phase.
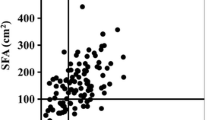
Figure 2 shows the positive correlation between the VFA level and the HOMA index values (r = 0.569, p < 0.0001; Fig. 2a) and the negative correlation between the VFA level and the H/M ratios measured using cardiac 123I-MIBG scintigraphy during the delayed phase (r = −0.509, p = 0.0005; Fig. 2b) in type 2 diabetes mellitus.
Multiple regression analysis was performed using the stepwise procedure. The level of VFA was predicted from the HOMA index values and the H/M ratio during the delayed phase (Table 4). In the other model analysis, the H/M ratio during the delayed phase was independently predicted from the level of VFA and the HOMA index values (data not shown).
Discussion
In this study, type 2 diabetic patients with high VFA levels had decreased uptake and enhanced clearance of 123I-MIBG in the heart relative to the values measured in type 2 diabetic patients with normal VFA levels. In addition, multiple regression analysis revealed that the level of VFA in the patients could be independently predicted by the HOMA index values and the H/M ratio during the delayed phase.
There are several reports indicating that an elevated VFA concentration is associated with insulin resistance in healthy subjects [7] and patients with type 2 diabetes mellitus [8]. Raji et al. [7] investigated the association between VFA levels and insulin resistance using a hyperinsulinemic–euglycemic clamp in non-obese healthy subjects. They found a significant increase in the VFA levels of healthy subjects with insulin resistance. Gastaldelli et al. [8] demonstrated that VFA has a significant negative impact on glycemic control through a decrease in peripheral insulin sensitivity in type 2 diabetic patients. In the present study, the level of VFA correlated with the body mass index, triglyceride levels, HDL-cholesterol levels, the fasting plasma insulin concentration, and the HOMA index values.
Although the specific mechanism that links the VFA level and insulin resistance remains to be elucidated, several mechanisms could explain our observations. Arner [25] has suggested that the flux of lipid from the visceral fat depot to liver might account for hepatic insulin resistance. In a canine model, development of insulin resistance occurred concomitantly with visceral adiposity because of a modest fat content in the diet but without increased calories [26]. The other possible mechanism is the contribution of an adipocyte-associated bioactive substance such as tumor necrosis factor-α (TNF-α), adiponectin, or resistin. TNF-α levels are essentially dependent on VFA [27] and inversely correlated with insulin sensitivity in obese type 2 diabetic patients [28]. Adiponectin decreases as VFA increases [29], and hypoadiponectinemia in patients with increased VFA is closely related to insulin resistance and hyperinsulinemia [30]. Gene and protein expression of resistin increased in abdominal fat and may also contribute to insulin resistance [31]. Resistin levels have been reported to be markedly elevated in obese mice and to be decreased by insulin sensitizers, such as thiazolidinediones [32].
The relationship between VFA and cardiovascular autonomic function has been examined in previous studies using HRV analysis or BRS [33, 34]. Lindmark et al. [33] have shown that VFA is associated with insulin resistance and signs of a high ratio of sympathetic versus parasympathetic reactivity by HRV. Beske et al. demonstrated reduced BRS associated with the level of VFA [34]. However, these parameters had reliability coefficients of around 50% [14]. In the present study, HRV and the plasma norepinephrine concentrations were not different between the two groups. But, a significant difference was seen in 123I-MIBG parameters. These results may suggest association of VFA in diabetic patients with impairment of uptake-1 (norepinephrine transporter) as well as the acceleration of norepinephrine turnover in sympathetic nerve terminal. Impairment in uptake-1 in diabetic rats has been reported [35]. However, 123I-MIBG uses the same uptake system and storage site as norepinephrine [36]. Our and others’ previous studies [11–13, 37] have demonstrated that 123I-MIBG scintigraphy is a fairly sensitive method for detecting cardiac sympathetic dysfunction in diabetic patients. The present results support the potential of 123I-MIBG scintigraphy for diagnosis of cardiovascular autonomic dysfunction.
Although the precise mechanisms underlying the interactions between high VFA and impaired autonomic function remain unclear, in our opinion there are several possible mechanisms. First, VFA may affect autonomic function through endothelial dysfunction and impairment of the nitrate oxide system. Visceral fat obesity is associated with endothelial dysfunction by oxidant stress [38]. Nitric oxidant damage and endothelial dysfunction are associated with cardiac autonomic dysfunction and increased HRV [39]. Moreover, we have recently reported that the HOMA index and the myocardial uptake of 123I-MIBG during the delayed phase were independent predictors of high-sensitivity C reactive protein (HSCRP) [12]. In fact, in a recent report demonstrating the association between increased VFA, insulin resistance, and HSCRP, the authors stressed the central role of endothelial dysfunction [40]. Second, VFA may cause dysregulation of autonomic nervous system through enhanced release of free fatty acids. Insulin resistance is strongly associated with VFA and free fatty acids [33, 41]. An increased release of free fatty acids from visceral adiposity into the portal circulation acts on the liver and secondarily leads to sympathetic activation [42].
Taken together, it is possible that VFA, insulin resistance, and autonomic dysfunction interact and reinforce each other through mechanisms that may be associated with endothelial dysfunction.
Compared with the normal VFA group, patients in the high VFA group showed cardiac diastolic dysfunction. Consistent with the present results, a previous study demonstrated that cardiac diastolic dysfunction is associated with cardiovascular autonomic dysfunction and insulin resistance [19]. Morricone et al. [43] reported that increased VFA is associated with cardiac left ventricular diastolic dysfunction in diabetic patients. Although the precise mechanism is unclear, diastolic dysfunction may interact with cardiac sympathetic nervous function through insulin resistance.
There are several limitations to this study. Firstly, subjects in the present study population had essential hypertension, which was treated with one or more antihypertensive drugs. These characteristics of the patients’ backgrounds have been reported to affect insulin resistance [44, 45] and sympathetic nerve function [46, 47]. Nonetheless, the results indicate that VFA in diabetic patients is related to cardiac depression and insulin resistance. Secondly, we have previously reported that HSCRP and hyperhomocysteine are associated with insulin resistance as well as cardiac sympathetic nerve function assessed by 123I-MIBG [12, 13]. Therefore, further studies are required to evaluate the association among the levels of VFA, HSCRP, hyperhomocysteine, HOMA index values, and 123I-MIBG parameters. In addition, the prognostic implications of cardiac autonomic function as assessed by 123I-MIBG scintigraphy remain to be addressed, although there are prognostic studies of heart failure patients using cardiac 123I-MIBG imaging [48].
In conclusion, our findings suggest that increased VFA in patients with type 2 diabetes are associated with depressed cardiovascular autonomic function and insulin resistance.
References
Kaplan NM. The deadly quartet. Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med 1989;149:1514–20.
Despres JP, Moorjani S, Lupien PJ, Tremblay A, Nadeau A, Bouchard C. Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 1990;10:497–511.
Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care 2000;23:465–71.
Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity and the prevalence of hypertension in Japanese-Americans. Circulation 2003;108:1718–23.
Fujimoto W, Bergstrom R, Boyko E, Chen K, Leonetti D, Newell-Morris L, et al. Visceral adiposity and incident coronary heart disease in Japanese-American men: the 10-year follow-up results of the Seattle Japanese-American Community Diabetes Study. Diabetes Care 1999;22:1808–12.
St-Pierre J, Lemieux I, Vohl MC, Perron P, Tremblay G, Despres JP, et al. Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am J Cardiol 2002;90:15–8.
Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab 2001;86:5366–71.
Gastaldelli A, Miyazaki Y, Pettiti M, Matsuda M, Mahankali S, Santini E, et al. Metabolic effects of visceral fat accumulation in type 2 diabetes mellitus. J Clin Endocrinol Metab 2002;87:5098–103.
Tsuji H, Larson MG, Venditti FJ Jr, Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Study. Circulation 1996;94:2850–5.
La Rovere MT, Bigger JT Jr, Marcus FI, Mortara A, Schwartz PJ. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infraction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infraction) Investigators. Lancet 1998;351:478–84.
Takahashi N, Nakagawa M, Saikawa T, Ooie T, Yufu K, Shigematsu S, et al. Effect of essential hypertension on cardiac autonomic function in type 2 diabetic patients. J Am Coll Cardiol 2001;38:232–7.
Anan F, Takahashi N, Nakagawa M, Ooie T, Saikawa T, Yoshimatsu H. High-sensitivity C-reactive protein is associated with insulin resistance and cardiovascular autonomic dysfunction in type 2 diabetic patients. Metabolism 2005;54:552–8.
Anan F, Yonemochi H, Masaki T, Takahashi N, Nakagawa M, Eshima N, et al. Homocysteine levels are associated with the results of 123I-metaiodobenzylguanidine myocardial scintigraphy in type 2 diabetic patients. Eur J Nucl Med Mol Imaging 2007;34:28–35.
Gerritsen J, TenVoorde BJ, Dekker JM, Kingma R, Kostense PJ, Bouter LM, et al. Measures of cardiovascular autonomic dysfunction nervous function: agreement, reproducibility, and reference values in middle age and elderly subjects. Diabetologia 2003;46:330–8.
Sakata K, Shirotani M, Yoshida H, Kurata C. Cardiac sympathetic nervous system in early essential hypertension assessed by 123I-MIBG. J Nucl Med 1999;40:6–11.
Spallone V, Menzinger G. Diagnosis of cardiovascular autonomic neuropathy in diabetes. Diabetes 1997;46:S67–76.
Watanabe K, Sekiya M, Tsuruoka T, Funada J, Kameoka H, Miyagawa M, et al. Relationship between insulin resistance and cardiac sympathetic nervous function in essential hypertension. J Hypertens 1999;17:1161–8.
Matsuzawa Y. Pathophysiology and molecular mechanisms of visceral fat syndrome: the Japanese experience. Diabetes Metab Rev 1997;13:313.
Liao D, Sloan RP, Cascio WE, Folsom AR, Liese AD, Evans GW, et al. Multiple metabolic syndrome is associated with lower heart rate variability. The Atherosclerosis Risk in Communities Study. Diabetes Care 1998;21:2116–22.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9.
Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K, et al. Abdominal fat: standardized technique for measurement at CT. Radiology 1999;211:283–6.
Kvist H, Chowdhury B, Sjostrom L, Tylen U, Cederblad A. Adipose tissue volume determination in males by computed tomography and 40K. Int J Obes 1988;12:249–66.
The Examination Committee of Criteria for ‘Obesity Disease’ in Japan, Japan Society for the Study of Obesity. New criteria for ‘Obesity Disease’ in Japan. Circ J 2002;66:987–92.
Sato T, Nishinaga M, Kawamoto A, Ozawa T, Takatsuji H. Accuracy of a continuous blood pressure monitor based on arterial tonometry. Hypertension 1993;21:866–74.
Arner P. Insulin resistance in type 2 diabetes: role of fatty acids. Diabete Metab Res Rev 2002;18:S5–9.
Mittelman SD, Van Citters GW, Kim SP, Davis DA, Dea MK, Hamilton-Wessler M, et al. Longitudinal compensation for fat-induced insulin resistance includes reduced insulin clearance and enhanced β-cell response. Diabetes 2000;49:2116–25.
Bertin E, Nguyen P, Guenounou M, Durlach V, Potron G, Leutenegger M. Plasma levels of tumor necrosis factor-alpha (TNF-α) are essentially dependent on visceral fat amount in type 2 diabetic patients. Diabetes Metab 2000;26:178–82.
Katsuki A, Sumida Y, Murashima S, Murata K, Takarada Y, Ito K, et al. Serum levels of tumor necrosis factor-α are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1998;83:859–62.
Hotta K, Funahashi T, Bodkin NL, Ortmeyer HK, Arita Y, Hansen BC, et al. Circulating concentrations of the adipocyte protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes 2001;50:1126–233.
Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endcrinol Metab 2001;86:1930–5.
McTernan PG, McTernan CL, Chetty R, Jenner K, Fisher FM, Lauer MN, et al. Increased resistin gene and protein expression in human abdominal adipose tissue. J Clin Endocrinol Metab 2002;87:2407.
Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, et al. The hormone resistin kinks obesity to diabetes. Nature 2001;409:307–12.
Lindmark S, Wiklund U, Olsson T, Eriksson JW. Dysregulation of the autonomic nervous system can be a link between visceral adiposity and insulin resistance. Obes Res 2005;13:717–28.
Beske SD, Alvarez GE, Ballard TP, Davy KP. Reduced cardiovagal baroreflex gain in visceral obesity: implications for the metabolic syndrome. Am J Physiol Heart Circ Physiol 2002;282:H630–5.
Kinjyo Y, Kajiyama S, Fujiwara H, Kanegawa N, Saji H. Influence of the polyol pathway on transporter reduction in diabetic cardiac sympathetic nerve: implication for heterogeneous accumulation of MIBG. Eur J Nucl Med Imaging 2005;32:438–42.
Glowniak JV, Kilty JE, Amara SG, Hoffman BJ, Turner FE. Evaluation of metaiodobenzylguanidine uptake by the norepinephrine, dopamine and serotonin transporters. J Nucl Med 1993;34:1140–6.
Mantysaari M, Kuikka J, Mustonen J, Tahvanainen K, Vanninen E, Lansimies E, et al. Noninvasive detection of cardiac sympathetic nervous dysfunction in diabetic patients using [123I] metaiodobenzylguanidine. Diabetes 1992;41:1069–75.
Perticone F, Ceravolo R, Candigliota M, Ventura G, Iacopino S, Sinopoli F, et al. Obesity and body fat distribution induce endothelial dysfunction by oxidant stress: protective effect of vitamin C. Diabetes 2001;50:159–65.
Meigs J, Jacques P, Selhub J, Singer D, Nathan D, Rifai N, et al. Fasting plasma homocysteine levels in the insulin resistance syndrome. The Framingham Offspring study. Diabetes Care 2001;24:1403–10.
Taegher G, Bertolini L, Scala L, Zoppini G, Zenari L, Falezza G. Non-alcholic hepatic steatosis and its relation to increased plasma biomarkers of inflammation and endothelial dysfunction in non-diabetic men. Role of visceral adipose tissue. Diabet Med 2005;22:1354–8.
Borden G. Free fatty acids and insulin secretion in humans. Curr Diab Rep 2005;5:167–70.
Benthem L, Keizer K, Wiegman CH, de Boer SE, Strubbe JH, Steffens AB, et al. Excess portal venous long-chain fatty acids induce syndrome X via HPA axis and sympathetic activation. Am J Physiol Endocrinol Metab 2000;279:E1286–93.
Morricone L, Malavazos AE, Coman C, Donati C, Hassan T, Caviezel F. Echocardiographic abnormalities in normotensive obese patients: relationship with visceral fat. Obes Res 2002;10:489–98.
Gavras HP. Issues in hypertension: drug tolerability and special populations. Am J Hypertens 2001;14 (Pt 2):231S–6S.
Lender D, Arauz-Pacheco C, Breen L, Mora-Mora P, Ramirez LC, Raskin P. A double blind comparison of the effects of amlodipine and enalapril on insulin sensitivity in hypertensive patients. Am J Hypertens 1999;12:298–303.
Kontopoulos AG, Athyros VG, Didangelos TP, Papageorgiou AA, Avramidis MJ, Mayroudi MC, et al. Effect of chronic quinapril administration on heart rate variability in patients with diabetic autonomic neuropathy. Diabetes Care 1997;20:355–61.
Rodgers JE, Patterson JH. Angiotensin II-receptor blockers: clinical relevance and therapeutic role. Am J Health Syst Pharm 2001;58:671–83.
Yamashina S, Yamazaki J. Role of MIBG myocardial scintigraphy in the assessment of heart failure: the need to establish evidence. Eur J Nucl Med Mol Imaging 2004;31:1353–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anan, F., Masaki, T., Yonemochi, H. et al. Abdominal visceral fat accumulation is associated with the results of 123I-metaiodobenzylguanidine myocardial scintigraphy in type 2 diabetic patients. Eur J Nucl Med Mol Imaging 34, 1189–1197 (2007). https://doi.org/10.1007/s00259-007-0421-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0421-6