Abstract
Purpose
The 2-(2-nitroimidazol-1-yl)-N-(3,3,3-trifluoropropyl)acetamide (EF3) is a 2-nitroimidazole derivative which undergoes bioreductive activation under hypoxic conditions. Using the PET tracer [18F]EF3 in mice, tumour-to-muscle ratios ranging from 1.3 to 3.5 were observed. This study investigated the impact of various interventions aimed at increasing [18F]EF3 elimination, thus potentially increasing the tumour-to-noise ratio in mice, by increasing the renal filtration rate (spironolactone, furosemide), decreasing tubular re-absorption (metronidazole, ornidazole, amino acid solution) or stimulating gastro-intestinal elimination (phenobarbital).
Methods
C3H mice were injected i.v. with an average of 12.95 MBq of [18F]EF3. Drugs were injected i.v. 15 min before the tracer or daily 4 days prior to the experiment (phenobarbital). Anaesthetised mice were imaged from 30 to 300 min with a dedicated animal PET (Mosaic, Philips). Regions of interest were delineated around the tumour, bladder, heart, liver and leg muscle. Radioactivity was expressed as a percentage of injected activity per gram of tissue.
Results
Ornidazole decreased the urinary excretion and increased the liver uptake of [18F]EF3, but without causing any changes in the other organs. Phenobarbital significantly increased the liver concentration and decreased radioactivity in blood and muscle without affecting the tracer uptake in tumour. Consequently, a small but non-significant increase in tumour-to-noise ratio was observed. Although some effects were observed with other drugs, they did not modify the tumour-to-noise ratio.
Conclusion
Only phenobarbital induced a trend toward an increased tumour-to-noise ratio that could possibly be tested in the clinical situation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumour hypoxia has long been known to be an important prognostic factor in human oncology [1]. Hypoxia leads to a more aggressive phenotype and increases tumour resistance to both radiation and chemotherapy [2]. The level of hypoxia within a tumour is correlated with local recurrence and overall survival in several tumour types [3–5]. Therefore, identifying hypoxic fractions in tumours may lead to modification of treatment strategies, such as concomitant use of hypoxic sensitisers or bioreductive agents, or an increase in the radiation dose in hypoxic regions in order to overcome radiation resistance and improve tumour curability.
The use of the 2-nitroimidazole compounds is an attractive method to detect tumour hypoxia [6]. These molecules undergo intracellular reduction by nitroreductase enzymes, and under hypoxic conditions their reduced moieties covalently bind to intracellular macromolecules, mainly to thiol-containing proteins. These adducts, trapped in the hypoxic cells, can be detected using specific antibodies by immunohistochemistry or immunofluorescence on tissue sections, by flow cytometry on cell suspensions, or by nuclear medicine assay for compounds labelled with a radioisotope [7].
The tri-fluorinated etanidazole derivative, 2-(2-nitroimidazol-1-yl)-N-(3,3,3-[18F]trifluoropropyl) acetamide ([18F]EF3) was synthesised by our group [8]. With an intermediate level of lipophilicity (octanol-to-water partition coefficient of 1.25), this compound represents a good compromise between homogeneous biodistribution within the tumour and rapid elimination. While more rapid tracer clearance has been observed with more hydrophilic compounds such as FMISO and FETNIM (octanol-to-water partition coefficient of 0.4 and 0.17, respectively [9]), this results in a less homogeneous tracer biodistribution [10]. EF5, another very similar compound, is even more lipophilic than EF3 (octanol-to-water partition coefficient of 5.7) and has shown a much slower clearance in animal models [11].
A preclinical validation of [18F]EF3 in tumour-bearing mice showed a blood half-life of 73.9 min. [18F]EF3 was mainly eliminated in urine via the kidneys, and to a lesser extent via the gastro-intestinal tract, with 75% and 16% of the injected dose found in urine and faeces, respectively, by 13 h after injection. The biodistribution was rapid in all organs, including the tumour. In all organs except the large and small bowel and the brain, the maximum radioactivity peaked at 5 min after injection and then progressively decreased [12]. In mouse tumour models, a tumour-to-blood ratio of about 3 was observed under ambient air conditions. It rose to 5 under 7% O2 breathing and went down to close to 1 under carbogen breathing. When co-injected with the cold nitroimidazole EF5 compound, a significant correlation was observed between the [18F]EF3 tumour-to-muscle ratio and the fluorescence intensity of EF5 in different mouse tumour models [13].
The aim of this study was to investigate different pharmacological interventions aimed at improving the tumour-to-background ratio of the PET tracer [18F]EF3. Knowing that nitroimidazole compounds undergo glomerular filtration and tubular re-absorption, we tested whether the co-administration of furosemide and spironolactone increased its glomerular filtration, and whether metronidazole, ornidazole and amino acid solution decreased its tubular re-absorption [14]. It has been shown that the megalin complex, a multi-ligand scavenger receptor located in the proximal renal tubules, plays an important role in tubular re-absorption [15]. Inhibition of this receptor by a solution of amino acids was found to result in a significant increase in the urinary excretion of labelled somatostatin analogues [16]. Consequently, we hypothesised that such pharmacological intervention could also inhibit the re-absorption of EF3. Similarly, we hypothesised that the co-injection of metronidazole or ornidazole, two compounds with a chemical structure close to that of EF3, could result in increased renal excretion. Lastly, considering that the nitroimidazole compounds are metabolised in the liver via cytochrome P450-dependent enzymes, the impact of phenobarbital, a potent inducer of liver enzymatic activity, was also tested [17].
Materials and methods
Animal and tumour models
Eight- to 13-week-old male C3H/HeOuJIco (IFFA Credo, Belgium) mice were used. Animals were maintained in a facility approved by the Belgian Ministry of Agriculture in accordance with current regulations and standards. The experimental design was approved by the Ethics Committee on animal experimentations of the medical school of the Université Catholique de Louvain. “Principles of laboratory animal care” (NIH publication No. 86-23, revised 1985) were strictly followed. Animals were housed four or five per cage and fed ad libitum.
FSA II fibrosarcomas syngeneic to C3Hf/Kam were used. These tumours were kindly provided by Dr. L. Milas from the University of Texas, M.D. Anderson Cancer Center, Houston, USA. Maintenance and expansion were done as previously described [18]. Tumour growth was determined by daily measurements of the three orthogonal diameters with a caliper. Experiments were performed on 9–11 mm mean diameter intramuscular FSA II.
Synthesis of [18F]EF3
The synthesis of [18F]EF3 was performed as previously described [8, 12]. [18F]EF3 was isolated by reverse phase semi-preparative high-performance liquid chromatography (HPLC) using an aqueous NaH2PO4 (1.38 g/l)/acetonitrile mixture (7/3) as eluent. Acetonitrile was removed by evaporation (<400 ppm). Gamma counting of HPLC fractions of [18F]EF3 solution demonstrated a radiochemical purity higher than 95%. Specific activity was typically in the order of 37 GBq/mmol.
Pharmaceutical intervention to modulate [18F]EF3 elimination
Spironolactone (Soludactone, Sanofi Winthrop Industrie, Notre Dame de Bondeville, France) was injected i.v. at a dose of 50 mg/kg. Furosemide (Lasix, Aventis Pharma, Frankfurt, Germany) was injected i.v. at a dose of 10 mg/kg. Metronidazole (Flagyl, Baxter Healthcare S.A., Castlebar, Ireland; solution of 500 mg/ml for infusion) was injected i.v. at a dose of 20 mg/kg. Ornidazole (Tiberal, La Roche, Grenzach-Wyhlen, Germany; solution of 1 g/6 ml) was diluted in 0.9% saline to obtain a concentration of 50 mg/ml and injected i.v. at a dose of 200 mg/kg. A commercially available amino acid solution containing 16 g of amino acids per 100 ml (Proteinsteril Hepa 8%, Fresenius, Bad Homburg, Germany) was injected i.v. at a dose of 400 mg/kg. Phenobarbital (Luminal, Bayer AG, Leverkusen, Germany) was injected i.p. at a dose of 80 mg/kg daily 4 days before [18F]EF3 injection.
Experimental design
Pharmaceutical interventions to modulate [18F]EF3 elimination were first assessed in non-tumour-bearing mice. Drugs which were efficient at inducing pharmacokinetic modulation in non-tumour-bearing mice were then evaluated in tumour-bearing mice. Animals were randomly assigned to receive spironolactone, furosemide, metronidazole, ornidazole, an amino acid solution or a vehicle only (control animals). Four mice were included per group.
Before [18F]EF3 injection, animals in the spironolactone and metronidazole groups and their control group (“control 1”) were anaesthetised with 80 mg/kg of ketamine (Ketalar, Parke-Davis, Warner Lambert S.A., Belgium) and 8 mg/kg of xylazine (Rompun, Bayer AG, Germany) injected i.p. This induction was followed by subcutaneous injection of 20 mg/kg of ketamine in the neck every 45 min. Because of the long duration of the experiments, this method resulted in a prohibitive mortality, especially at later time points in the amino acid and ornidazole groups. A modified protocol was thus designed. Mice randomised to the furosemide, ornidazole and amino acid groups and their control group (“control 2”), and tumour-bearing mice, were anaesthetised with a combination of zolazepam 50 mg/ml and tiletamine hypochloride 50 mg/ml (Zoletil 100, Virbac, Carros, France) and xylazine. The induction dose was 50 mg/kg of Zoletil and 8 mg/kg of xylazine injected i.p. Maintenance doses of 25 mg/kg of Zoletil and 2 mg/kg of xylazine were injected subcutaneously in the neck every 30 min.
As soon as the mice had been anaesthetised, the various drugs aiming at modulating the tracer elimination were injected in the tail vein. Fifteen minutes later, [18F]EF3 (average radioactivity of 12.95 MBq or 0.35 mCi) was injected i.v.. Animals were then taped on a specially designed bed to undergo micro-PET image acquisition.
A second group of animals included FSA tumour-bearing mice. Only pharmacological interventions that proved to be of potential interest were studied. Mice (five per group) were randomised to receive amino acids, ornidazole, phenobarbital or the vehicle only. Anaesthesia was performed with the zolazepam/tiletamine/xylazine protocol.
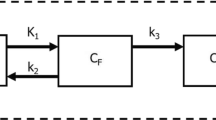
PET imaging and data analysis
PET imaging was performed using a dedicated small-animal PET scanner (MOSAIC, Philips Medical Systems, Cleveland, USA) [19]. Sequential static acquisitions were performed at 30, 60, 90, 120, 150, 180, 210, 240 and 300 min after [18F]EF3 injection. Acquisition duration was adapted to compensate for decay: 10 min during the first 2 h (first four images), 20 min during the next 2 h (four images) and 40 min for the last 2 h (last two images). All images contained at least 24×106 true events. Before reconstruction, raw data were corrected for random and scattered coincidences and for system dead-time. Transmission scans were acquired in single mode using a 370 MBq 137Cs source for attenuation correction of emission data. All images were reconstructed with a fully 3D iterative algorithm (3D-RAMLA). Each reconstructed matrix was composed of 120 transverse 128×128 images with cubic voxels of 1 mm.
Regions of interest (ROIs) were manually delineated on the heart (taken as a surrogate for blood), liver and lower leg muscle. ROIs were delineated in the first frame after window and level setting adjustments for maximal organ visibility and then transferred to the other frames. The bladder was automatically segmented using a combined clustering–watershed algorithm (J.A. Lee, unpublished data, 2006).
Results are expressed as the percentage of the injected dose per gram of tissue assuming a density value of 1 for all tissues. All data were corrected for isotope decay. Data were analysed with NCSS 2004 (Number Cruncher Statistical System, Kaysville, USA, 2005). The areas under the curves from 30 to 300 min (AUC30–300) were determined to assess tracer distribution in normal tissues and tumour, as well as bladder accumulation. Groups were compared using a bilateral t test on AUC30–300 values after logarithmic transformation, with a significance threshold level of 0.05. Tumour-to-blood (TBR) and tumour-to-muscle (TMR) ratios between the control group and treated groups were compared using a repeated measure analysis of variance model, with a significance threshold level of 0.05.
Results
Pharmacokinetics of [18F]EF3 in non-tumour-bearing mice after pharmacological interventions
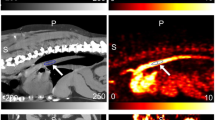
The pharmacokinetics of [18F]EF3 in the blood, muscle, liver and urine is presented in Fig. 1. Metronidazole, furosemide and spironolactone had no influence on the pharmacokinetics of [18F]EF3. The injection of the amino acid solution decreased [18F]EF3 uptake in the leg but not at a statistically significant level (p = 0.08). No differences were observed in the other organs. Ornidazole decreased the tracer’s urinary elimination (p = 0.007) and muscular uptake (p = 0.04). It also induced a borderline reduction in the tracer’s blood uptake (p = 0.114), but increased its liver uptake (p = 0.02).
AUC30–300 values of [18F]EF3 uptake in non-tumour-bearing mice after various pharmacological interventions in ketamine/xylazine (grey bars) and zolazepam/tiletamine/xylazine anaesthetised mice (white bars). Spiro spironolactone, Mtz metronidazole, AA amino acid solution, Orn ornidazole, Furo furosemide
Pharmacokinetics of [18F]EF3 in tumour-bearing mice after pharmacological interventions
The previous experiments have shown that both ornidazole and (to a lesser extent) the amino acid solution were able to decrease the background level of [18F]EF3 in normal tissues. In this experiment, we investigated whether this translated into an increased tumour-to-normal tissue ratio. In addition to ornidazole and amino acids, phenobarbital was tested on tumour-bearing mice. The borderline results observed with the amino acids injected in non-tumour-bearing mice were not confirmed with the tumour-bearing mice (Fig. 2). The amino acids did not modify the pharmacokinetics of [18F]EF3 in the tumour or normal tissues. Consequently, no increase in the TMR and TBR was observed (Fig. 3). As previously reported, the co-injection of ornidazole decreased the urinary excretion of [18F]EF3 (p = 0.002) and increased its liver uptake (p<0.001) (Fig. 2). However, for tumour-bearing mice, no significant effect was observed in the tumour and blood, and a decreasing trend was observed only in muscle uptake (p = 0.24). Consequently, ornidazole did not modify the TMR or TBR (Fig. 3). Lastly, the injection of phenobarbital significantly increased the liver concentration of [18F]EF3 (p = 0.001) but significantly decreased the blood (p = 0.027) and muscle (p = 0.014) radioactivity (Fig. 2). However, it did not modify the pharmacokinetics of [18F]EF3 in the tumour. Consequently, a small increase in TBR and TMR was observed after the injection of phenobarbital, but it did not reach a significant level (p = 0.27 and 0.17 for the TBR and the TMR respectively) (Fig. 3).
Discussion
This study was designed to explore different pharmacological interventions aimed at selectively increasing the elimination of the hypoxic tracer [18F]EF3 in normal tissues, and thus increasing the tumour-to-normal tissue ratio. None of the compounds tested were able to significantly affect the selective uptake of [18F]EF3 in mouse tumour. Borderline results obtained with amino acids and ornidazole in the first part of the study were not confirmed subsequently. Only phenobarbital was able to significantly decrease the background level of radioactivity in blood and in muscle, without affecting the tracer uptake in tumour. Unfortunately, this only translated into a non-significant increase in tumour-to-normal tissue ratios.
It has been previously reported that a spironolactone (soludactone), a diuretic acting at the distal tubular level, increased misonidazole excretion in rat by 28% [14]. As tubular re-absorption typically occurs at the proximal part of the tubule, it was hypothesised that this finding was due to an aspecific diuretic effect. This is the reason why in the present study, furosemide, a much more potent diuretic, was also tested. Both compounds, however, failed to modify the pharmacokinetics of [18F]EF3.
Another intervention was to compete with proximal tubular re-absorption. It has been demonstrated that the megalin complex is essential for tubular re-absorption of somatostatin analogues and that this mechanism can be substantially inhibited by co-infusion of an amino acid solution [16]. It was hypothesised that the megalin complex could also be involved in nitroimidazole tubular re-absorption, but our results did not demonstrate any modification of [18F]EF3 pharmacokinetics after injection of an amino acid solution. Similarly, the co-injection of [18F]EF3 with two other nitroimidazole compounds, i.e. metronidazole and ornidazole, which hypothetically compete with [18F]EF3 for tubular re-absorption, did not result in a modification of its pharmacokinetics.
The only therapeutic intervention to increase [18F]EF3 elimination and increase the tumour-to-normal tissue ratios was co-injection with phenobarbital. This observation agrees with published data showing that nitroimidazole compounds are more rapidly cleared after microsomal enzyme induction by phenobarbital [20]. In the present study, the effect of phenobarbital was only marginal, which could be explained by the wide heterogeneity of metabolic modifications observed in the group of mice tested. Indeed, in one mouse no effect or even decreased elimination was observed after phenobarbital treatment. The reason for this unexpected behaviour is not known.
In all the control mice, we observed that the urinary elimination of [18F]EF3 was much lower than in the preclinical experiments previously reported by our group. By 330 min after tracer injection, 63% of the injected dose was expected in the urine; however, in the present experiments, on average only 29% of the injected dose was measured in the urine by 330 min. Similarly, the half-life of [18F]EF3 in blood was measured at 154.1 min in the present experiments, compared with 73.9 min in our previous studies [12]. Long-term anaesthesia could be an explanation for this reduced elimination. It has been shown that an i.p. injection of ketamine/xylazine (150 mg/kg/15 mg/kg) dramatically decreases heart rate and cardiac output in mice [21]. As a consequence, the glomerular filtration of [18F]EF3 could then be decreased. Our observation is in line with published data showing that anaesthesia with methoxyflurane decreases both liver and kidney perfusion, thus substantially decreasing the clearance of [125I]IAZA [22]. A similar effect of anaesthesia with ketamine and xylazine has also been reported for the elimination of [99mTc]MAG3, a dynamic renal SPECT tracer (S. Walrand, unpublished data, 2006). However, even if a possible effect of anaesthesia on EF3 pharmacokinetics cannot be excluded, it is unlikely that an important effect of all these drugs could have been missed, since all groups of mice were treated similarly.
In conclusion, the different pharmacological interventions aimed at increasing the clearance of [18F]EF3 did not result in increased tumour-to-normal tissue ratios. Only phenobarbital showed a trend that could possibly be tested in clinical situations. A cytochrome induction could easily be implemented in clinical practice with a phenobarbital intake of 150 mg over 7 days.
References
Bush RS, Jenkin RD, Allt WE, Beale FA, Bean H, Dembo AJ, et al. Definitive evidence for hypoxic cells influencing cure in cancer therapy. Br J Cancer Suppl 1978;37:302–6.
Hockel M, Schlenger K, Aral B, Mitze M, Schaffer U, Vaupel P. Association between tumor hypoxia and malignant progression in advanced cancer of the uterine cervix. Cancer Res 1996;56:4509–15.
Fyles AW, Milosevic M, Wong R, Kavanagh MC, Pintilie M, Sun A, et al. Oxygenation predicts radiation response and survival in patients with cervix cancer. Radiother Oncol 1998;48:149–56.
Hockel M, Knoop C, Schlenger K, Vorndran B, Baussmann E, Mitze M, et al. Intratumoral pO2 predicts survival in advanced cancer of the uterine cervix. Radiother Oncol 1993;26:45–50.
Nordsmark M, Overgaard M, Overgaard J. Pretreatment oxygenation predicts radiation response in advanced squamous cell carcinoma of the head and neck. Radiother Oncol 1996;41:31–9.
Hodgkiss RJ. Use of 2-nitroimidazoles as bioreductive markers for tumour hypoxia. Anticancer Drug Des 1998;13:687–702.
Sorensen M, Horsman MR, Cumming P, Munk OL, Keiding S. Effect of intratumoral heterogeneity in oxygenation status on FMISO PET, autoradiography, and electrode pO2 measurements in murine tumors. Int J Radiat Oncol Biol Phys 2005;62:854–61.
Josse O, Labar D, Georges B, Gregoire V, Marchand-Brynaert J. Synthesis of [18F]-labeled EF3 [2-(2-nitroimidazol-1-yl)-N-(3,3,3-trifluoropropyl)-acetamide], a marker for PET detection of hypoxia. Bioorg Med Chem 2001;9:665–75.
Yang DJ, Wallace S, Cherif A, Li C, Gretzer MB, Kim EE, et al. Development of F-18-labeled fluoroerythronitroimidazole as a PET agent for imaging tumor hypoxia. Radiology 1995;194:795–800.
Evans SM, Kachur AV, Shiue CY, Hustinx R, Jenkins WT, Shive GG, et al. Noninvasive detection of tumor hypoxia using the 2-nitroimidazole [18F]EF1. J Nucl Med 2000;41:327–36.
Ziemer LS, Evans SM, Kachur AV, Shuman AL, Cardi CA, Jenkins WT, et al. Noninvasive imaging of tumor hypoxia in rats using the 2-nitroimidazole [18F]EF5. Eur J Nucl Med Mol Imaging 2003;30:259–66.
Mahy P, De Bast M, Leveque PH, Gillart J, Labar D, Marchand J, et al. Preclinical validation of the hypoxia tracer 2-(2-nitroimidazol-1-yl)-N-(3,3,3-[18F]trifluoropropyl)acetamide, [18F]EF3. Eur J Nucl Med Mol Imaging 2004;31:1263–72.
Mahy P, De Bast M, Gillart J, Labar D, Gregoire V. Detection of tumour hypoxia: comparison between EF5 adducts and [18F]EF3 uptake on an individual mouse tumour basis. Eur J Nucl Med Mol Imaging 2006;33:553–6.
Akel G, Canal P, Soula G. Renal elimination of the hypoxic cell radiosensitizer misonidazole in Wistar rats: influence of some drugs on its excretion. Eur J Drug Metab Pharmacokinet 1985;10:181–7.
de Jong M, Barone R, Krenning E, Bernard B, Melis M, Visser T, et al. Megalin is essential for renal proximal tubule reabsorption of 111In-DTPA-octreotide. J Nucl Med 2005;46:1696–700.
Barone R, Pauwels S, De Camps J, Krenning EP, Kvols LK, Smith MC, et al. Metabolic effects of amino acid solutions infused for renal protection during therapy with radiolabelled somatostatin analogues. Nephrol Dial Transplant 2004;19:2275–81.
Schuetz EG. Induction of cytochromes P450. Curr Drug Metab 2001;2:139–47.
Milas L, Hunter N, Mason K, Withers HR. Immunological resistance to pulmonary metastases in C3Hf-Bu mice bearing syngeneic fibrosarcoma of different sizes. Cancer Res 1974;34:61–71.
Surti S, Karp JS, Perkins AE, Cardi CA, Daube-Witherspoon ME, Kuhn A, et al. Imaging performance of A-PET: a small animal PET camera. IEEE Transactions on Medical Imaging 2005;24:844–52.
Workman P, Brown JM. Structure-pharmacokinetic relationships for misonidazole analogues in mice. Cancer Chemother Pharmacol 1981;6:39–49.
Yang XP, Liu YH, Rhaleb NE, Kurihara N, Kim HE, Carretero OA. Echocardiographic assessment of cardiac function in conscious and anesthetized mice. Am J Physiol 1999;277:H1967–74.
Stypinski D, Wiebe LI, Tam YK, Mercer JR, McEwan AJ. Effects of methoxyflurane anesthesia on the pharmacokinetics of 125I-IAZA in Sprague-Dawley rats. Nucl Med Biol 1999;26:959–65.
Acknowledgements
Nicolas Christian is a research fellow of the Fonds de la Recherche Scientifique of Belgium (F.R.I.A., Fonds pour la formation à la Recherche dans l’Industrie et l’Agriculture). The project was supported by a grant from the “Fonds Joseph Maisin”, Brussels, Belgium, by the European Commission’s Sixth Framework Programme funding (Contract no. LSHC-CT-2004-505785), and by a program project from the “Institut National du Cancer” of France (Project INCa N° RS 020).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christian, N., Bol, A., De Bast, M. et al. Determination of tumour hypoxia with the PET tracer [18F]EF3: improvement of the tumour-to-background ratio in a mouse tumour model. Eur J Nucl Med Mol Imaging 34, 1348–1354 (2007). https://doi.org/10.1007/s00259-007-0376-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0376-7