Abstract
Purpose
The aim of this study was to estimate 201Tl SPECT and CT-MRI cut-off values that lead to a validated prognostic classification for the end-point overall survival, in order to discriminate glioma patients with good and poor prognosis at an early stage during chemotherapeutic treatment.
Methods
We studied patients who underwent 201Tl SPECT and CT-MRI before and after two courses of chemotherapy. Cut-off values were retrieved from the Cox model. Patients were classified according to the computed cut-off values, creating subgroups of patients with different prognosis in terms of survival [tumour regression (TR); stable disease (SD); tumour progression (TP)]. The differences between the subgroups were assessed by Kaplan-Meier analyses. The predictive performance of the classification procedure was evaluated by a leave-one-out cross-validation method.
Results
201Tl SPECT classified 41% of the patients as SD, 25% as TR and 34% as TP. CT-MRI classified 82% of the patients as SD, and only 4% and 14% as TR and TP, respectively. Of those patients with a relatively long overall survival (i.e. ≥16 months), cross-validation estimates of 201Tl SPECT classification rates were 50% TR and 50% SD, and cross-validation estimates of CT-MRI classification rates were 7% TR, 72% SD, and 21% TP.
Conclusion
We constructed a 201Tl SPECT model that makes it possible to identify glioma patients with a good or a poor prognosis at an early stage during chemotherapeutic treatment. With this model, accurate predictions can be made with regard to the expected duration of survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Standard treatment of patients with newly diagnosed malignant glioma consists of surgery [1–3] and radiotherapy [4, 5], with or without adjuvant chemotherapy [6–8]. Despite multimodality treatment, malignant gliomas recur almost invariably, with a poor prognosis and few long-term survivors. Up to now, therapeutic options for patients with recurrent glioma have been limited. Second surgery, re-irradiation, chemotherapy, immune therapy and gene therapy are possible treatment modalities in case of tumour recurrence. Chemotherapy may be effective, particularly in tumours of oligodendroglial origin [9, 10], although response percentages are not high in recurrent malignant astrocytoma [11]. With limited response rates and potential toxicity of chemotherapeutic treatment, reliable and early response assessment is essential.
In 1990, Macdonald et al. [12] introduced the currently used imaging-based criteria for response assessment in clinical trials of supratentorial malignant glioma. These criteria were derived from those used in general oncology, based on major changes in tumour size on enhanced computed tomography (CT) or magnetic resonance imaging (MRI), in combination with steroid use and neurological findings. However, over time, it has become apparent that the Macdonald criteria have certain shortcomings [13]. They are not applicable to all clinical situations in which brain tumour response needs to be assessed. Moreover, quantitative evaluation of treatment response with CT or MRI is not without limitations [14–21], and has been proven to be susceptible to considerable inter-observer variability [22]. Functional brain imaging techniques, such as single-photon emission computed tomography (SPECT) and positron emission tomography (PET), are claimed to be more specific than structural imaging methods, such as CT and MRI, in the follow-up of glioma patients. During the last decade, thallium-201 (201Tl) SPECT has been used to differentiate tumour recurrence from radiation necrosis [23–27], and more recently, its role in the evaluation of glioma treatment response during chemotherapy has been explored [28–32].
In view of the limitations of structural brain imaging techniques and the growing interest in functional brain imaging techniques, we recently established the value of 201Tl SPECT as a predictor of overall survival (OS) and response to chemotherapy in patients with recurrent glioma, as compared with that of conventional CT and MRI [28]. In that study, response classification on CT-MRI was derived from the criteria developed by Macdonald et al. [12], differentiating patients with tumour regression (TR) (≥50% reduction in tumour size), tumour progression (TP) (≥25% increase in tumour size), and stable disease (SD) (all other situations). As there are no comparable, generally accepted criteria for the classification of glioma treatment response on 201Tl SPECT, 201Tl SPECT response classification was also based on the −50/+25% criteria as constructed for CT-MRI. That study demonstrated that 201Tl SPECT was superior to CT and MRI as an early predictor of OS and response to chemotherapy in patients with recurrent glioma. Especially maximal tumour intensity on 201Tl SPECT appeared to be a powerful predictor of outcome, both at baseline and after two courses of chemotherapy.
The aim of the present study was to estimate 201Tl SPECT cut-off values that lead to a validated prognostic classification for the end-point OS, in order to discriminate patients with a good and those with a poor prognosis at an early stage during treatment. To evaluate the validity of the Macdonald criteria for the prediction of OS, CT-MRI cut-off values were computed as well.
Materials and methods
Patients
Patients treated with paclitaxel or the combination of procarbazine, CCNU and vincristine (PCV) chemotherapy for recurrent glioma were identified in the brain tumour database of the VU University Medical Centre (Amsterdam, the Netherlands). Patients who had undergone adequate 201Tl SPECT and CT or MRI (before and after contrast material administration) before and after two courses of chemotherapy were included. This applied to the same patients as described in (the follow-up analysis of) our previous study [28].
Imaging
SPECT was started 30 min after intravenous injection of 150 MBq 201Tl-chloride, using a dual-head gamma camera (Genesys, ADAC, Milpitas CA). Projection data were acquired with a 64×64 matrix, 60 s per projection, collecting 64 projections. Images were reconstructed with a Hanning filter (cut-off frequency 0.56 cycles/cm), without attenuation correction. All CT scans were performed using a standard protocol including 3–5 mm slices for the posterior fossa and 8–10 mm slices for the remainder of the brain, before and after contrast material administration. All MRI scans were performed using a standard protocol including transverse T2-weighted images and T1-weighted images, before and after contrast material administration.
201Tl SPECT scans were evaluated by one nuclear medicine physician, whereas CT and MRI scans were evaluated by one neuroradiologist; both were unaware of the patient’s outcome and of the alternative imaging test results. 201Tl SPECT analysis comprised measurement of the maximal tumour intensity at baseline (before chemotherapy) and at follow-up (after two courses of chemotherapy). Maximal tumour intensity was defined as the ratio of the mean tumour counts in the axial slice with the maximal tumour activity to the mean activity in the contralateral supratentorial hemisphere. Each baseline and follow-up CT and MRI scan was evaluated on the basis of the image slice on which the lesion showed the largest diameter, and tumour size was measured on this slice. Tumour size was defined as the product of the two largest perpendicular transverse enhancing tumour diameters on the post-contrast images. The diameters were measured on the hard copies, by reference to the centimetre scale printed on the film. The percentage change in maximal tumour intensity on 201Tl SPECT, and in tumour size on CT-MRI, was calculated by dividing follow-up data by baseline data for every individual patient. With respect to the calculation of the change in 201Tl SPECT maximal tumour intensity, a correction was made for the partial non-tumour-related change in intensity. As maximal tumour intensity is defined as the ratio of the mean tumour counts in the axial slice with the maximal tumour intensity to the mean activity in the contralateral supratentorial hemisphere, the maximal intensity of normal brain tissue is 1. In order to calculate only the tumour-related change in intensity, we subtracted 1 from all baseline and follow-up maximal tumour intensity data.
Statistical analysis
To compute 201Tl SPECT and CT-MRI cut-off values for the prediction of OS, we performed Cox regression analyses in which OS was predicted by baseline 201Tl SPECT maximal tumour intensity or CT-MRI tumour size and the percentage change after two courses of chemotherapy. Overall survival was defined as the interval (in months) from start of chemotherapy to death. Because of the proven impact of histology on prognosis in glioma [33], the prognostic value of histology was examined in additional regression analyses. Therefore, tumour histology was dichotomised [glioblastoma multiforme (GBM) versus non-GBM]. The cut-off values were subsequently determined by setting the Cox model chance of surviving 10 months (i.e. the median OS of the included patients) equal to (50−Y)% and (50+Y)%. The value of Y was chosen such that the differences in OS between the response groups, as measured by the log-rank statistic, were maximised, both for 201Tl SPECT and for CT-MRI. Patients demonstrating a chance of at least (50+Y)% to survive 10 months were classified as “good prognosis patients”; in other words, these patients were predicted to demonstrate TR. Those with a chance of at most (50−Y)% to survive 10 months were classified as “poor prognosis patients”; these patients were predicted to demonstrate TP. Those with a chance over (50−Y)% and less than (50+Y)% to survive 10 months were classified as “intermediate prognosis patients”; these patients were predicted to demonstrate SD.
Thereafter, we classified our patients according to the computed cut-off values, creating subgroups of patients with different survival prognoses (TR; SD; TP). The differences between the three subgroups of patients with regard to OS were assessed by Kaplan-Meier analyses. The predictive performance of the classification procedure was assessed by a leave-one-out cross-validation method. Instead of using an external data set, prediction was mimicked by removing one patient from the data set, determining cut-off values on the basis of all other patients, and providing a prognosis for the removed patient. This prognosis was compared with the observed OS of the patient.
Results
Patient characteristics
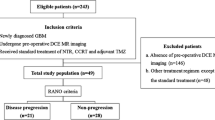
From January 1994 to April 2001, 67 patients had been treated with PCV (procarbazine, CCNU, vincristine) or paclitaxel for recurrent glioma in the VU University Medical Centre. Forty-four of these 67 patients were included in the current study. Patient characteristics are shown in Table 1. Primary tumour histologies included GBM (n=27), anaplastic astrocytoma (n=7), (anaplastic) oligodendroglioma (n=9) and oligo-astrocytoma (n=1); altogether, there were 27 GBMs versus 17 non-GBMs. All patients had previously undergone cranial surgery and radiation therapy. Thirty-two patients had been treated with PCV, and 12 with paclitaxel. The median OS was 10 months (range 3–47 months).
Computation of cut-off values
Cox regression analyses (results not tabulated) demonstrated that 201Tl SPECT maximal tumour intensity, and particularly the percentage change after two courses of chemotherapy (baseline P=0.01; change P<0.01), was strongly related to OS. Tumour size on CT-MRI (baseline P=0.05; change P=0.01) had an effect on OS as well. We found no significant association between histology and survival in addition to 201Tl SPECT maximal tumour intensity (P=0.20) or CT-MRI tumour size (P=0.07). Therefore, we decided to construct cut-off values that were not adjusted for histology. The cut-off values for 201Tl SPECT and CT-MRI are graphically displayed in Fig. 1. As can be read from Fig. 1, prognosis depended on both baseline and follow-up data, as for a certain change in 201Tl SPECT maximal tumour intensity or CT-MRI tumour size, prognosis was better if the baseline maximal tumour intensity was lower, or its size smaller (and vice versa). For TP, the chance of surviving 10 months was equal to or less than 33%, and for TR, the chance of surviving 10 months was at least 67%. The patients classified as SD had an intermediate prognosis. The chances 33% and 67% led to maximum differences in OS between the response groups as measured by the log-rank statistic, both for 201Tl SPECT and for CT-MRI. An important difference between Fig. 1a and Fig. 1b is that the vertical distance between the lines in Fig. 1b is much larger. This suggests a less powerful performance of CT-MRI in separating patients with regard to OS in comparison with 201Tl SPECT.
Cut-off values for the prediction of OS. TR tumour regression, defined as ≥67% chance of surviving 10 months; SD stable disease, defined as >33% and <67% chance of surviving 10 months; TP tumour progression, defined as ≤33% chance of surviving 10 months. *Applies to the 10th, 25th, 50th, 75th and 90th percentiles of all baseline measurements. a 201Tl SPECT; b CT-MRI
The results of the Kaplan-Meier analyses are demonstrated in Fig. 2, and indicate that both 201Tl SPECT (P<0.01; Fig. 2a) and CT-MRI (P<0.01; Fig. 2b) could distinguish all three subgroups of patients (TR, SD, TP), who differed significantly with regard to OS. The median OS in the TR, SD and TP groups was 31, 10 and 7 months with 201Tl SPECT, and 45, 11 and 5 months with CT-MRI, respectively.
The predicted numbers of patients with TR, SD and TP are presented in Table 2. 201Tl SPECT classified 25% of the patients as TR and 34% as TP, whereas CT-MRI classified the vast majority (82%) of patients as SD, and only 4% and 14% as TR and TP, respectively. Using cross-validation methodology, 201Tl SPECT classified 50% (7/14) of the patients with OS ≥16 months as TR (chance of surviving 10 months ≥67%) , and the remaining 50% (7/14) as SD. From the patients with OS ≤7 months, 201Tl SPECT classified 57% (8/14) as TP (chance of surviving 10 months ≤33%), and the remaining 43% (6/14) as SD. CT-MRI classified only 7% (1/14) of the patients with OS ≥16 months as TR, and only 21% (3/14) of the patients with OS ≤7 months as TP. Moreover, 21% (3/14) of the patients with OS ≥16 months were wrongly classified as TP with CT-MRI.
Discussion
In the current study, we estimated cut-off values that lead to a validated prognostic classification for the end-point OS, both for 201Tl SPECT and for CT-MRI, in a subgroup of patients treated with chemotherapy for recurrent glioma in our hospital. Kaplan-Meier survival curves, constructed by the classification of patients according to the computed cut-off values, indicated that both 201Tl SPECT and CT-MRI were able to distinguish subgroups of patients that differed significantly with regard to OS. With respect to CT-MRI, the current model differentiates the subgroups of patients more strongly with regard to OS than the classification used in our previous study [28]. However, as the vast majority (82%) of patients were now classified as SD, this model appears to be of limited value. The model constructed for 201Tl SPECT, on the other hand, classified a substantial percentage (59%) of patients as TR or TP, and thus appears to be useful in the identification of both good and poor prognosis patients. With respect to patients with a relatively long survival time of at least 16 months, results were even more pronounced after cross-validation. 201Tl SPECT classified 50% of these patients as TR and 50% as SD, whereas CT-MRI classified only 7% of these patients as TR, and 21% wrongly as TP.
A limitation of our study is the small number of patients included. Nevertheless, the sample size was large enough to validate the predictions by cross-validation. A more elaborate approach to validate the current 201Tl SPECT model would be to use an external data set. A source of concern in this respect is the heterogeneity of the 201Tl SPECT literature regarding the quantitative methodology of the various measurement techniques: different methods are being used to define tumour as well as reference tissue activity. In a previous study, however, we provided 201Tl SPECT nomograms, which can be used to convert results of different 201Tl SPECT data sets [34].
In conclusion, we constructed a 201Tl SPECT model that makes it possible to identify patients with a good or a poor prognosis at an early stage during chemotherapeutic treatment for recurrent glioma. With this model, on the basis of two 201Tl SPECT scans, accurate predictions can be made with regard to the expected duration of survival. Such information offers the treating physician the possibility to select responding patients for further treatment, and to avoid ineffective, potentially toxic treatment in non-responding patients. After further refinement of the current 201Tl SPECT model, it would also be interesting to evaluate its utility in the evaluation of response to new brain tumour therapies.
References
Hess KR. Extent of resection as a prognostic variable in the treatment of gliomas. J Neuro-oncol 1999;42:227–31
Simpson JR, Horton J, Scott C, Curran WJ, Rubin P, Fischbach J, et al. Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys 1993;26:239–44
Metcalfe SE, Grant R. Biopsy versus resection for malignant glioma. Cochrane Database Syst Rev 2001;(3):CD002034
Walker MD, Alexander E Jr, Hunt WE, MacCarty CS, Mahaley MS, Mealey J Jr, et al. Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg 1978;49:333–43
Kristiansen K, Hagen S, Kollevold T, Torvik A, Holme I, Nesbakken R, et al. Combined modality therapy of operated astrocytomas grade III and IV. Confirmation of the value of postoperative irradiation and lack of potentiation of bleomycin on survival time: a prospective multicenter trial of the Scandinavian Glioblastoma Study Group. Cancer 1981;47:649–52
Fine HA, Dear KB, Loeffler JS, Black PM, Canellos GP. Meta-analysis of radiation therapy with and without adjuvant chemotherapy for malignant gliomas in adults. Cancer 1993;71:2585–97
Medical Research Council Brain Tumor Working Party. Randomized trial of procarbazine, lomustine, and vincristine in the adjuvant treatment of high-grade astrocytoma: a Medical Research Council trial. J Clin Oncol 2001;19:509–18
Stewart LA. Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 2002;359:1011–8
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, et al. Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 1998;90:1473–9
van den Bent MJ, Kros JM, Heimans JJ, Pronk LC, van Groeningen CJ, Krouwer HG, et al. Response rate and prognostic factors of recurrent oligodendroglioma treated with procarbazine, CCNU, and vincristine chemotherapy. Dutch Neuro-oncology Group. Neurology 1998;51:1140–5
Wong ET, Hess KR, Gleason MJ, Jaeckle KA, Kyritsis AP, Prados MD, et al. Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 1999;17:2572
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 1990;8:1277–80
Perry JR, Cairncross JG. Glioma therapies: how to tell which work? J Clin Oncol 2003;21:3547–9
Perry JR, DeAngelis LM, Schold SC Jr, Burger PC, Brem H, Brown MT, et al. Challenges in the design and conduct of phase III brain tumor therapy trials. Neurology 1997;49:912–7
Zeltzer PM, Friedman HS, Norris DG, Ragab AH. Criteria and definitions for response and relapse in children with brain tumors. Cancer 1985;56:1824–6
Brada M, Yung WK. Clinical trial end points in malignant glioma: need for effective trial design strategy. Semin Oncol 2000;27:11–9
Byrne TN. Imaging of gliomas. Semin Oncol 1994;21:162–71
Kaplan RS. Complexities, pitfalls, and strategies for evaluating brain tumor therapies. Curr Opin Oncol 1998;10:175–8
Cairncross JG, Pexman JHW, Rathbone MP, DelMaestro RF. Postoperative contrast enhancement in patients with brain tumor. Ann Neurol 1985;17:570–2
Forsyth PAJ, Petrov E, Mahallati H, Cairncross JG, Brasher P, MacRae ME, et al. Prospective study of postoperative magnetic resonance imaging in patients with malignant gliomas. J Clin Oncol 1997;15:2076–81
Kumar AJ, Leeds NE, Fuller GN, van Tassel P, Maor MH, Sawaya RE, et al. Malignant gliomas: MR imaging spectrum of radiation therapy-and chemotherapy-induced necrosis of the brain after treatment. Radiology 2000;217:377–84
Vos MJ, Uitdehaag BMJ, Barkhof F, Heimans JJ, Baayen HC, Boogerd W, et al. Interobserver variability in the radiological assessment of response to chemotherapy in glioma. Neurology 2003;60:826–30
Benard F, Romsa J, Hustinx R. Imaging gliomas with positron emission tomography and single-photon emission computed tomography. Semin Nucl Med 2003;33:148–62
Yamamoto Y, Nishiyama Y, Toyama Y, Kunishio K, Satoh K, Ohkawa M. 99mTc-MIBI and 201Tl SPET in the detection of recurrent brain tumours after radiation therapy. Nucl Med Commun 2002;23:1183–90
Schwartz RB, Holman BL, Polak JF, Garada BM, Schwartz MS, Folkerth R, et al. Dual-isotope single-photon emission computerized tomography scanning in patients with glioblastoma multiforme: association with patient survival and histopathological characteristics of tumor after high-dose radiotherapy. J Neurosurg 1998;89:60–8
Schwartz RB, Carvalho PA, Alexander E III, Loeffler JS, Folkerth R, Holman BL. Radiation necrosis vs high-grade recurrent glioma: differentiation by using dual-isotope SPECT with 201TI and 99mTc-HMPAO. Am J Neuroradiol 1991;12:1187–92
Gomez-Rio M, Martinez del Valle Torres D, Rodriguez-Fernandez A, Llamas-Elvira JM, Lozano SO, Font CR, et al. 201TI-SPECT in low-grade gliomas: diagnostic accuracy in differential diagnosis between tumour recurrence and radionecrosis. Eur J Nucl Med Mol Imaging 2004;31:1237–43
Vos MJ, Hoekstra OS, Barkhof F, Berkhof J, Heimans JJ, van Groeningen CJ, et al. Thallium-201 single-photon emission computed tomography as an early predictor of outcome in recurrent glioma. J Clin Oncol 2003;21:3559–65
Roesdi MF, Postma TJ, Hoekstra OS, van Groeningen CJ, Wolbers JG, Heimans JJ. Thallium-201 SPECT as response parameter for PCV chemotherapy in recurrent glioma. J Neurooncol 1998;40:251–5
Källén K, Geijer B, Malmström P, Andersson AM, Holtas S, Ryding E, et al. Quantitative 201Tl SPET imaging in the follow-up of treatment for brain tumour: a sensitive tool for the early identification of response to chemotherapy? Nucl Med Commun 2000;21:259–67
Källén K, Burtscher IM, Holtås S, Ryding E, Rosen I. 201Thallium SPECT and 1H-MRS compared with MRI in chemotherapy monitoring of high-grade malignant astrocytomas. J Neurooncol 2000;46:173–85
Vallejos V, Balaña C, Fraile M, Roussos Y, Capellades J, Cuadras P, et al. Use of 201Tl SPECT imaging to assess the response to therapy in patients with high grade gliomas. J Neurooncol 2002;59:81–90
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fischbach AJ, et al. Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 1993;85:704–10
Tony B, Vos MJ, Berkhof J, Postma TJ, van Lingen A, Heimans JJ, et al. Interobserver variability in the semi-quantitative assessment of 201Tl SPECT in cerebral gliomas. Nucl Med Commun 2005;26:45–8
Acknowledgements
The authors would like to thank B.M.J. Uitdehaag for statistical assistence.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vos, M.J., Berkhof, J., Postma, T.J. et al. Thallium-201 SPECT: the optimal prediction of response in glioma therapy. Eur J Nucl Med Mol Imaging 33, 222–227 (2006). https://doi.org/10.1007/s00259-005-1883-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-1883-z