Abstract
Purpose
Few studies have investigated the clinical impact of whole-body positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG) in endometrial cancer. We aimed to assess the value of integrating FDG-PET into the management of endometrial cancer in comparison with conventional imaging alone.
Methods
All patients with histologically confirmed primary advanced (stage III/IV) or suspicious/documented recurrent endometrial cancer, with poor prognostic features (serum CA-125 >35 U/ml or unfavourable cell types), or surveillance after salvage therapy were eligible. Before FDG-PET scanning, each patient had received magnetic resonance imaging and/or computed tomography (MRI-CT). The receiver operating characteristic curve method with calculation of the area under the curve (AUC) was used to compare the diagnostic efficacy. Clinical impacts were determined on a scan basis.
Results
Forty-nine eligible patients were accrued and 60 studies were performed (27 primary staging, 33 post-therapy surveillance or restaging on relapse). The clinical impact was positive in 29 (48.3%) of the 60 scans. Mean standardised uptake values (SUVs) of true-positive lesions were 13.2 (range 5.7–37.4) for central pelvic lesions and 11.1 (range 1.5–37.4) for metastases. The sensitivity of FDG-PET alone (P<0.0001) or FDG-PET plus MRI-CT (P<0.0001) was significantly higher than that of MRI-CT alone in overall lesion detection. FDG-PET plus MRI-CT was significantly superior to MRI-CT alone in overall lesion detection (AUC 0.949 vs 0.872; P=0.004), detection of pelvic nodal/soft tissue metastases (P=0.048) and detection of extrapelvic metastases (P=0.010), while FDG-PET alone was only marginally superior by AUC (P=0.063).
Conclusion
Whole-body FDG-PET coupled with MRI-CT facilitated optimal management of endometrial cancer in well-selected cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endometrial cancer is a common gynaecological cancer and is generally classified as a tumour with a good prognosis. The overall survival rate of patients with endometrial cancer is expected to be high because a high percentage of patients have early-stage disease at the time of diagnosis [1, 2]. Unfortunately, the prognosis is poor in advanced [1, 3, 4] or recurrent endometrial carcinoma, except for isolated vaginal recurrence [3, 5]. The situation becomes more difficult when the extrapelvic sites have been previously irradiated or are multifocal, although occasionally successful salvage has been achieved with long-term survival after hormone therapy, radical surgery and radiotherapy/chemotherapy [3, 6–8].
Imaging studies such as magnetic resonance imaging and/or computed tomography (MRI-CT) can be used to evaluate disease extension and provide important information for treatment planning [9, 10]. Preoperative CA-125 measurement may play a role in predicting extrauterine spread of clinically localised endometrial cancer [11–13].
Metabolic imaging by positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG) is now widely used in the evaluation of cervical and ovarian carcinoma [14–18]. However, limited information is available regarding the usefulness of FDG-PET in endometrial cancer [19–23]. In the literature, two retrospective case series [19, 20] investigated the role of PET for post-therapy surveillance and a single prospective study evaluated the sensitivity and specificity of FDG-PET for detection of pelvic and para-aortic node metastasis preoperatively [23]. The diagnostic efficacy and benefit of FDG-PET in other settings of endometrial cancer are still uncertain.
In this prospective study, we aimed to assess the value of integrating whole-body FDG-PET into the management of endometrial cancer in comparison with conventional MRI-CT imaging alone.
Materials and methods
Patients
Patients with histologically confirmed endometrial cancer (any type, any differentiation) were eligible if they met any one of the following criteria: (1) absence of previous treatment or immediate postoperative state with (a) clinical stage III on MRI-CT, clinical stage IVA (histology-proven) or clinical stage IVB [supraclavicular lymph node (LN) or inguinal LN or other solitary distant metastasis], (b) preoperative tentative diagnosis of any stage and CA-125 >35 U/ml, or (c) unfavourable cell type (serous papillary, clear cell or small cell undifferentiated carcinomas); (2) after primary definitive treatment with (a) unexplained CA-125 >35 U/ml in two consecutive measurements at least 1 month apart (MRI-CT score ≤2), (b) suspicious lesions on conventional studies (score ≥3), or (c) documented recurrence; or (3) after salvage therapy, (a) if routine follow-up studies were negative (MRI-CT score ≤2 and CA-125 <35 U/ml) 3 months after salvage therapy (in which case FDG-PET was performed 6–12 months after salvage therapy), (b) CA-125 >35 U/ml in two consecutive measurements at least 1 month apart (unexplained), or (c) if conventional studies were positive (score ≥3). This study was approved by the institutional review board of the Chang Gung Memorial Hospital, and informed consent was obtained from each enrolled patient.
Standard treatment
Generally, surgical staging and tailored hysterectomy were performed in our patients if clinically feasible. Total abdominal hysterectomy and bilateral salpingo-oophorectomy (TAH-BSO) was performed in clinical stage I patients and radical hysterectomy was employed only for unequivocal cervical involvement [24]. Indications for pelvic and para-aortic lymphadenectomy in high-risk patients in our institution were similar to those in other reports [25]. They were: (1) unfavourable histological subtypes (serous papillary, clear cell or small cell undifferentiated carcinomas), (2) histological grade 3, (3) myometrial invasion >1/2 and (4) clinically advanced disease with extrauterine or extrapelvic extension. Maximal cytoreduction was attempted in cases of extrauterine dissemination.
CT imaging
The CT images were obtained using a Hi-speed CT scanner (GE Medical Systems, Milwaukee, USA) or a Somatom Plus 4 multi-slice CT scanner (Volume Zone, Version A40, Siemens AG Medical, Forscheim, Germany). Patients fasted for at least 4 h before study and received oral meglumine diatrizoate (Gastrografin; Schering Health care, West Sussex, UK) for bowel preparation. Scanning was undertaken in the craniocaudal direction, between the diaphragm and the perineum with and without contrast enhancement. The Hi-speed CT scanner generated contiguous slices of 5 mm thickness whereas the Somatom Plus 4 multi-slice CT scanner generated contiguous slices of 10 mm thickness.
MRI
MR images were obtained by performing different pulse sequences with either a 1.5-Tesla Magnetom Vision or a Magnetom Expert scanner (Siemens Medical Systems, Erlangen, Germany) using a phased-array body coil. T2 spin-echo [time repetition (TR)/time echo (TE), 4,000/99] and T1 spin-echo (TR/TE, 500/15) sequences were acquired in transaxial, sagittal and coronal sections of abdomen and pelvis with a matrix size of 256×256 pixels. Slice thickness was 5 mm in the transaxial plane and 2.5 mm in the sagittal and coronal planes.
PET imaging
The imaging instrument used was an ECAT EXACT HR+PET camera (CTI, Knoxville, TN), with a full-width at half-maximum of 4.5 mm and a 15-cm transaxial field of view. After fasting for at least 6 h, the patient received 370 MBq of FDG. For optimal tumour identification, all patients were catheterised and given diuretics to reduce bladder activity. Dual-phase PET images were acquired at 40 min from the head to the upper thigh using a two-dimensional mode. An additional session of 3-h scans from T1–11 to the upper thigh in three-dimensional mode was obtained in some patients. Data acquisition and reconstruction were performed according to our previous protocol [14]. The semiquantitative evaluation was based on a region of interest (ROI) analysis, giving standardised uptake values (SUVs). The ROI was placed on the emission image over an FDG-avid area. The ROI edge was the contour for 75% of peak counts. Images were interpreted visually and semi-quantitatively on early and available late scans without explicit interpretative criteria. There was no preselected SUV cut-off value. In dual-phase PET, a combination of early and late images was used to determine whether the observed lesion was fixed or not as well as to calculate changes in SUV from early to late results [14].
Image interpretation
Both MRI-CT and FDG-PET images were interpreted visually and classified using a five-point scoring scale: 0, normal; 1, probably normal; 2, equivocal; 3, probably abnormal; 4, definitely abnormal [14]. The MRI-CT score with respect to LNs was further defined as: 0, a normal finding; 1, visible LNs less than 0.5 cm in size, considered reactive and unrelated to metastasis; 2, any LN of length 1 cm or a little less, giving an overall equivocal impression; 3, LNs more than 1 cm in length in the short axis and/or multiple LNs (n≥3) with a size of 0.5–1 cm; and 4, confluent LNs with central necrosis or irregular contours [14, 15, 26].
Determination of lesion status
Verification by either surgical exploration or CT- or ultrasound-guided biopsy was performed whenever possible for suspicious lesions (score ≥3) detected by CT-MRI or FDG-PET. Lesions with an unsettled status were either designated “indeterminate” or subjected to a second assessment (by both CT-MRI and FDG-PET) 3–6 months later to avoid false-negative results. Disease status was determined based on pathological findings or clinical follow-up.
Clinical impact of FDG-PET
The clinical impact of FDG-PET scanning was classified as: (1) negative: if PET led to unnecessary, additional invasive procedures; (2) no change: if PET yielded the same findings as MRI-CT, if false-positive and false-negative FDG-PET findings did not affect surgical staging or treatment, or if PET detected an incurable relapse; or (3) positive: (i) if PET led to modification of treatment owing to correct staging, with upstaging or downstaging in comparison with MRI-CT, (ii) if PET confirmed involvement of a single site by a distant recurrence (leading to adherence to curative treatment), (iii) if PET led to early detection of a curable recurrence or re-recurrence, (iv) if PET led to deferral of exploration following false-positive MRI-CT findings or (v) if PET resulted in a change to palliation, avoiding a futile salvage attempt.
Statistical analysis
We hypothesised that use of FDG-PET in addition to MRI-CT would have a positive clinical impact in 40% of patients. Based on a 95% confidence interval (CI) of ±12.5%, approximately 49 patients were to be accrued to provide a sufficient sample size for evaluation of the efficacy of FDG-PET in the management of endometrial cancer.
A visual score of 3 or 4 was considered to be positive and scores 0, 1 and 2 as negative for calculations of sensitivity, specificity and accuracy [14, 15, 19]. The receiver operating characteristic (ROC) curves were plotted and values of the area under the curves (AUCs) were calculated to compare the diagnostic efficacy of MRI-CT versus MRI-CT plus FDG-PET. Progression-free survival was measured from the date of FDG-PET to disease relapse or to the date of last follow-up (for disease-free patients). Overall survival was defined from the date of FDG-PET to the date of death. All statistical tests were two-sided.
Results
Between April 2001 and May 2004, 49 patients (age range 30–81 years, median 55 years) with endometrial cancer were recruited into the study. Demographic characteristics of patients are summarised in Table 1. The initial FIGO stage was IA in nine cases, IB in six, IC in three, IIA in one, IIB in five, IIIA in seven, IIIB in one, IIIC in 13, IVB in three and unstaged in one. Sixty whole-body FDG-PET studies were done, with nine patients receiving two scans and one patient receiving three scans. The mean follow-up period after PET scanning was 14.0±9.9 months (range 6 days to 46.7 months). Forty-six patients underwent surgery, one patient had radiotherapy alone and two patients did not receive treatment. The histological subtype was endometrioid carcinoma in 26 cases, adenosquamous carcinoma in six, serous papillary carcinoma in eight, clear cell carcinoma in eight and small cell undifferentiated carcinoma in one. Indications for FDG-PET included: 27 scans for primary staging, 26 for recurrence surveillance and seven after salvage treatment.
Diagnostic efficacy
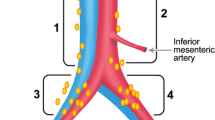
Although dual-phase PET scan was performed in all, no statistical significant differences in SUV or diagnostic efficacy between early and late images were found (data not shown). Therefore, we used 40-min scan results for all analyses in this study. The mean SUVs of true-positive lesions were 13.2 (range 5.7–37.4) for central pelvic lesions and 11.1 (range 1.5–37.4) for metastases (Fig. 1). For every scan, 11 sites were evaluated (11×60=660 sites). On a lesion-by-lesion basis, 45 ROIs with unsettled lesion status remained indeterminate and were not evaluated at the time of this report. Results of comparison between FDG-PET plus MRI-CT and MRI-CT alone in respect of the remaining 615 ROIs are summarised in Table 2. The sensitivity of FDG-PET plus MRI-CT (91%, 95%CI 83–96%) was significantly higher than that of MRI-CT alone (67%, 95%CI 56–76%) in overall lesion detection (P<0.0001), and a significant difference was also observed when comparing FDG-PET alone (87%, 95%CI 79–94%) with MRI-CT alone in overall detection (P<0.0001). Furthermore, the accuracy of FDG-PET plus MRI-CT was significantly different from that of MRI-CT alone (97%, 95%CI 96–99 vs 94%, 95%CI 91–95, P<0.0001); only specificity (99%, 95%CI 97–99 vs 98%, 95%CI 96–99, P=0.344) was not significantly different. We used the ROC method to evaluate the diagnostic efficacy of FDG-PET plus MRI-CT versus MRI-CT alone (Table 3). FDG-PET alone was marginally superior to MRI-CT in overall detection (AUC 0.929 vs 0.872; P=0.063). However, the integration of PET into conventional imaging studies significantly improved overall lesion detection (AUC 0.949 vs 0.872; P=0.004) (Fig. 2), detection of pelvic soft tissue and pelvic nodes (AUC 0.944 vs 0.868; P=0.048) and detection of extrapelvic metastases (AUC 0.949 vs 0.838; P=0.010). Additional FDG-PET was superior to MRI-CT alone in the detection of extrapelvic soft tissue metastases (P=0.007), but not in the detection of extrapelvic lymph nodes (P=0.237).
A 53-year-old female with clear cell carcinoma of the endometrium, stage IIIc, underwent radical hysterectomy and adjuvant chemotherapy. Progressive elevation of serum CA-125 (229 U/ml and 267 U/ml) was noted after completion of treatment. Conventional image study found tumour metastases in the pelvic cavity, pelvic lymph nodes and para-aortic lymph nodes. FDG-PET scan detected an additional metastatic lesion in a left supraclavicular lymph node (arrow; SUV=1.5)
Clinical impact of FDG-PET
Clinical impacts of the 60 scans are summarised in Table 4. Overall, the treatment plan was positively influenced as a result of 29 (48.3%) scans. Of the 27 scans included for primary staging, six (22.2%) had a positive clinical impact. These six patients had treatment modification owing to correct staging after FDG-PET evaluation. In three patients with clinical stage IB but elevated CA-125, surgery was changed to para-aortic lymphadenectomy plus standard surgical staging for occult para-aortic LNs or adnexal metastases. In addition, FDG-PET showed right adrenal gland metastasis in one patient with extensive pelvic and para-aortic LN metastases (on pretreatment MRI), who underwent optimal curative-intent surgery and removal of the metastatic right adrenal gland (Fig. 3). Microscopic residual disease was established in this patient because of the FDG-PET finding. In one of the patients with unstaged clear cell carcinoma who was referred after TAH-BSO, adjuvant radiotherapy was performed to the whole pelvis on the basis of the PET findings (score 3) in the pelvis, and no relapse was observed in the subsequent 23 months. In another patient, the treatment strategy was changed to palliative treatment because of FDG-PET detection of extensive dissemination with left sacral metastasis.
Of the 26 scans performed for surveillance of recurrence, 19 (73.1%) yielded a benefit. In seven patients PET confirmed isolated distant recurrences, resulting in adherence to curative salvage treatment (Table 5), while in five disseminated disease was confirmed. Among the remaining seven cases, negative FDG-PET results led to deferral of exploration in two patients who had false-positive findings on conventional studies. Both remained free of disease at 15.8 and 9.6 months of follow-up, respectively. In two other patients, FDG-PET facilitated early detection of disease recurrence in the presence of unexplained elevation of serum CA-125 and extensive but manageable LN metastases. In the remaining three patients absence of recurrence was confirmed by FDG-PET.
Seven PET scans were performed after salvage therapy and four (57.1%) yielded a clinical benefit. One patient had had a persistent elevated CA-125 and suspicious lung lesions (on CT) at 30 months after the third salvage treatment while PET scans were negative. Her first and second recurrences in the left parametrium and left iliac fossa, respectively, were controlled, as reported previously [8]. She had a third relapse at the upper margin of the intraoperative radiotherapy field, which was again controlled with surgery and adjuvant chemotherapy. Hence she was observed and subsequent follow-up CT and PET were negative; she has now been progression-free for 65 months after her third relapse. Another patient who presented with lung metastasis and multiple upper abdominal recurrences after initial surgery at another hospital underwent cytoreductive surgery and chemotherapy followed by high-dose progestin. Because of FDG-avid residual lung lesions, she received intensity-modulated radiotherapy to a residual lung nodule as consolidation. She has been disease-free for 27 months since salvage treatment. Two other patients with incurable disease were switched to palliative therapy for disseminated disease.
On the other hand, in one patient undergoing primary staging, both FDG-PET and MRI erroneously suggested a bone metastasis; this patient underwent a negative bone biopsy and has remained disease-free for 13.8 months. FDG-PET had a negative impact in three of the patients undergoing surveillance of recurrence/restaging post recurrence. One patient had an unnecessary liver aspiration for a false-positive liver lesion. The second patient underwent exploratory laparotomy for documented pelvic recurrence, with multiple liver metastases being revealed during surgery. Both FDG-PET and MRI were falsely negative for liver lesions in this case. The third patient, with clinically advanced cancer, was misinterpreted as being totally disease-free on the basis of FDG-PET shortly after postoperative chemoradiation therapy, and developed full-blown disseminated disease 3 months later. There was no adverse result in patients who have received salvage therapy.
Discussion
Limited information is available regarding the clinical utility of FDG-PET in endometrial cancer [19–23]. Only two reports have provided SUV data when assessing the FDG avidity of endometrial cancer: one included five patients who had a mean SUV of 18.8±9 [27] and the other included nine patients with a SUV range of 3.8–16.8 [28]. Lerman et al. found substantial variations in endometrial uptake when comparing patients with benign endometrial pathology (mean SUVmax 4.5±2.1, range 2.3–8.2), patients with normal menstrual cycles (menstrual phase: mean SUVmax 5±3.2, range 2.3–16.6; proliferative phase: mean SUVmax 2.6±1.1, range 1.1–5.7; ovulatory phase: mean SUVmax 3.7±0.9, range 2–5.4; secretory phase: mean SUVmax 2.5±1.1, range 1.3–5.6) and postmenopausal patients (mean SUVmax 1.7±0.5, range 0.8–3) [27]. Our data showed that the minimum SUV of true-positive central pelvic lesions was 5.7 (mean 13.2±7.1), whereas it could be as low as 1.5 (mean 11.1±6.4) for metastatic lesions, indicating a great variation in the uptake of endometrial cancer.
In a retrospective case series (n=34), Belhocine et al. noted that FDG-PET had a sensitivity of 96% and a specificity of 78% for post-therapy surveillance and led to alteration in treatment in 35% [19]. Saga et al. evaluated 30 scans in postoperative patients and found a sensitivity of 100%, with the treatment plan being affected in 33.3% [20]. Selecting well-defined clinical situations prospectively, we found that the sensitivity of FDG-PET alone (87%) or FDG-PET plus MRI-CT (91%) was significantly higher than that of MRI-CT alone (67%) in overall lesion detection. Furthermore, the accuracy of FDG-PET plus MRI-CT was significantly higher than that of MRI-CT alone (P<0.0001). Comparison of AUCs revealed that FDG-PET plus MRI-CT significantly improved diagnostic efficacy in overall lesion detection (p=0.004).
The value of an additional diagnostic tool should be judged on the basis of whether the information acquired may result in better clinical decisions, although the definition of clinical benefit could differ in various clinical situations. In our series, the treatment plan was positively influenced by 29 (48.3%) scans. Notably, in seven patients distant metastasis to a sole site was confirmed by FDG-PET, hence facilitating aggressive management and subsequent good outcome (Table 5). The reassurance offered by FDG-PET improved the chance of survival in these patients, in whom palliative treatment may be taken for granted.
Horowitz et al. [23] have recently reported a prospective study on the role of FDG-PET in primary staging. A total of 11% (2 of 18) patients had pathological nodal metastasis. PET predicted that three patients had positive nodes; two of these findings proved true positive and one, false positive. In the current consensus, endometrial cancer is a surgical disease and surgical staging must be instituted if feasible, though the extent of retroperitoneal lymph node dissection has been controversial. We expected a low yield of nodal metastases in clinical stage I or II disease. Moreover, it was our expectation that PET would not be sensitive enough to replace lymphadenectomy. Therefore we selected those patients with a high risk of extrauterine spread, unfavourable cell types or elevated serum CA-125 level for primary staging with additional PET.
Our results demonstrated that only 30% (three out of ten scans) of the subgroup with pre-treatment elevation of the CA-125 level derived clinical benefit from FDG-PET. Sometimes FDG-PET led to upstaging, or the FIGO stage remained the same but PET facilitated complete identification of tumour extent and facilitated a decision on the optimal extent of surgery. On the other hand, although both MRI-CT and FDG-PET missed one patient with positive peritoneal cytology, this did not on the whole affect the treatment (peritoneal lavage cytology is performed routinely for every endometrial cancer patient) and therefore the clinical impact was designated as “no change”. Three patients accrued owing to a CA-125 value of >35 U/ml had no clinical benefit from additional PET in the presence of coexisting adenomyosis. Elevated CA-125 levels are often encountered in patients with other gynaecological abnormalities such as subclinical endometriosis, adenomyosis and pelvic inflammatory disease.
In our series, additional FDG-PET had a positive impact in 73.1% of cases when performed for post-therapy surveillance; this confirms the findings of earlier retrospective studies [20, 21]. As mentioned above, one of our patients with stage IIIc cancer and chemoradiation had full-blown disseminated disease 3 months following a completely negative FDG-PET scan (performed within 2 months of the last course of chemotherapy). This was in contrast to the results of Saga et al., who found no false-negative FDG-PET cases among 30 FDG-PET examinations [21]. We assumed that previously irradiated tissues are likely to be inherently more heterogeneous, fibrotic and relatively poorly vascularised than untreated tumour, which may result in different metabolic uptake. Hence, the efficacy of FDG-PET could be compromised if it were to be used as an imaging tool in patients who have very recently undergone surgery and chemoradiation. On the other hand, distant metastasis at an unirradiated site could be identified by PET despite the absence of high FDG uptake (supraclavicular node in Fig. 1).
The aims of PET in patients with recurrence are to reduce the number of patients explored for occult disseminated disease and also to permit precise delivery of surgical or radiation treatment to all localised lesions. When the recurrence is localised, surgery such as exenteration can be employed to eradicate the previously irradiated recurrent cancer [3, 5, 29, 30]. Morris et al. and Barakat et al. reported 5-year survival rates of 45% and 20%, respectively, despite high operative complication rates of 60% and 80% [29, 30]. The rationale for salvage surgery could be more solid with PET restaging. Confirmation of persistent viable tumour cells or re-recurrent disease after salvage will help action to be taken at the earliest opportunity. The integration of whole-body FDG-PET scanning into conventional imaging studies exhibits superiority in delineating tumour extent for primary staging or restaging after relapse, in facilitating early detection of recurrence or re-recurrence and in avoiding over-treatment. Substantial benefits can be achieved in well-selected endometrial cancer patients.
References
Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, et al. Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group study. Gynecol Oncol 1991;40:55–65
Irvin WP, Rice LW, Berkowitz RS. Advances in the management of endometrial adenocarcinoma. A review. J Reprod Med 2002;47:173–189; discussion 189–90
Aalders JG, Abeler V, Kolstad P. Recurrent adenocarcinoma of the endometrium: a clinical and histopathological study of 379 patients. Gynecol Oncol 1984;17:85–103
Kao MS. Management of recurrent endometrial cancer. Chang Gung Med J 2004;27:639–45
Sears JD, Greven KM, Hoen HM, Randall ME. Prognostic factors and treatment outcome for patients with locally recurrent endometrial cancer. Cancer 1994;74:1303–8
Jeyarajah AR, Gallagher CJ, Blake PR, Oram DH, Dowsett M, Fisher C, et al. Long-term follow-up of gonadotrophin-releasing hormone analog treatment for recurrent endometrial cancer. Gynecol Oncol 1996;63:47–52
Moore TD, Phillips PH, Nerenstone SR, Cheson BD. Systemic treatment of advanced and recurrent endometrial carcinoma: current status and future directions. J Clin Oncol 1991;9:1071–88
Huang HJ, Lai CH, Tsai CS, Ng KK, Lin CT. Radical resection and intraoperative radiotherapy for a recurrent endometrial cancer after prolonged remission following aggressive salvage therapy: case report. Chang Gung Med J 1999;22:654–9
Manfredi R, Mirk P, Maresca G, Margariti PA,Testa A, Zannoni GF, et al. Local-regional staging of endometrial carcinoma: role of MR imaging in surgical planning. Radiology 2004;231:372–8
Frei KA, Kinkel K, Bonel HM, Lu Y, Zaloudek C, Hricak H. Prediction of deep myometrial invasion in patients with endometrial cancer: clinical utility of contrast-enhanced MR imaging—a meta-analysis and Bayesian analysis. Radiology 2000;216:444–9
Duk JM, Aalders JG, Fleuren GJ, de Bruijn HW. CA 125: a useful marker in endometrial carcinoma. Am J Obstet Gynecol 1986;155:1097–102
Patsner B, Mann WJ. The value of preoperative serum CA 125 levels in patients with a pelvic mass. Am J Obstet Gynecol 1988;159:873–6
Dotters DJ. Preoperative CA 125 in endometrial cancer: is it useful? Am J Obstet Gynecol 2000;182:1328–34
Yen TC, Ng KK, Ma SY, Chou HH, Tsai CS, Hsueh S, et al. Value of dual-phase 2-fluoro-2-deoxy-d-glucose positron emission tomography in cervical cancer. J Clin Oncol 2003;21:3651–8
Lai CH, Huang KG, See LC, Yen TC, Tsai CS, Chang TC, et al. Restaging of recurrent cervical carcinoma with dual-phase [18F]fluoro-2-deoxy-d-glucose positron emission tomography. Cancer 2004;100:544–52
Grigsby PW, Siegel BA, Dehdashti F. Lymph node staging by positron emission tomography in patients with carcinoma of the cervix. J Clin Oncol 2001;19:3745–9
Rose PG, Adler LP, Rodriguez M, Faulhaber PF, Abdul-Karim FW, Miraldi F. Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: a surgicopathologic study. J Clin Oncol 1999;17:41–5
Zimny M, Siggelkow W, Schroder W, Nowak B, Biemann S, Rath W, et al. 2-[Fluorine-18]-fluoro-2-deoxy-d-glucose positron emission tomography in the diagnosis of recurrent ovarian cancer. Gynecol Oncol 2001;83:310–5
Belhocine T, De Barsy C, Hustinx R, Willems-Foidart J. Usefulness of 18F-FDG PET in the post-therapy surveillance of endometrial carcinoma. Eur J Nucl Med Mol Imaging 2002;29:1132–9
Saga T, Higashi T, Ishimori T, Mamede M, Nakamoto Y, Mukai T, et al. Clinical value of FDG-PET in the follow up of post-operative patients with endometrial cancer. Ann Nucl Med 2003;17:197–203
Nakahara T, Fujii H, Ide M, Mochizuki Y, Takahashi W, Yasuda S, et al. F-18 FDG uptake in endometrial cancer. Clin Nucl Med 2001;26:82–3
Lentz SS. Endometrial carcinoma diagnosed by positron emission tomography: a case report. Gynecol Oncol 2002;86:223–4
Horowitz NS, Dehdashti F, Herzog TJ, Rader JS, Powell MA, Gibb RK, et al. Prospective evaluation of FDG-PET for detecting pelvic and para-aortic lymph node metastasis in uterine corpus cancer. Gynecol Oncol 2004;101:164–71
Mariani A, Webb MJ, Keeney GL, Calori G, Podratz KC. Role of wide/radical hysterectomy and pelvic lymph node dissection in endometrial cancer with cervical involvement. Gynecol Oncol 2001;83:72–80
Larson DM, Broste SK, Krawisz BR. Surgery without radiotherapy for primary treatment of endometrial cancer. Obstet Gynecol 1998;91:355–9
Dorfman RE, Alpern MB, Gross BH, Sandler MA. Upper abdominal lymph nodes: criteria for normal size determined with CT. Radiology 1991;180:319–22
Lerman H, Metser U, Grisaru D, Fishman A, Lievshitz G, Even-Sapir E. Normal and abnormal 18F-FDG endometrial and ovarian uptake in pre- and postmenopausal patients: assessment by PET/CT. J Nucl Med 2004;45:266–71
Torizuka T, Kanno T, Futatsubashi M, Okada H, Yoshikawa E, Nakamura F, et al. Imaging of gynecologic tumors: comparison of 11C-choline PET with 18F-FDG PET. J Nucl Med 2003;44:1051–6
Morris M, Alvarez RD, Kinney WK, Wilson TO. Treatment of recurrent adenocarcinoma of the endometrium with pelvic exenteration. Gynecol Oncol 1996;60:288–91
Barakat RR, Goldman NA, Patel DA, Venkatraman ES, Curtin JP. Pelvic exenteration for recurrent endometrial cancer. Gynecol Oncol 1999;75:99–102
Acknowledgements
This study was supported by grant CMRPG32022 from Chang Gung Memorial Hospital and grant NSC-93-NU-7-182-003 from the National Science Council and the Institute of Nuclear Energy Research, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chao, A., Chang, TC., Ng, KK. et al. 18F-FDG PET in the management of endometrial cancer. Eur J Nucl Med Mol Imaging 33, 36–44 (2006). https://doi.org/10.1007/s00259-005-1876-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-1876-y