Abstract
Purpose
The aim of this study was to evaluate the clinical usefulness of scintigraphy with 99mTc-depreotide in the assessment of loco-regional nodal spread in patients with suspected lung cancer in comparison with computed tomography (CT).
Methods
Eighty-six patients were investigated with single-photon emission computed tomography (SPECT) of the thorax after i.v. injection of 740 MBq 99mTc-depreotide. The results were evaluated in conjunction with a thoracic CT scan in all 86 patients with 204 lymph node stations. The scintigraphic results were correlated with cytological (38), histological (20) or clinical–radiological (146) findings and compared with CT. The quantitative evaluation of depreotide uptake was performed on 48 cytologically or histologically verified nodal stations from 28 patients by SPECT using region of interest analysis with four different reference regions.
Results
99mTc-depreotide scintigraphy for all 204 investigated lymph node stations had a sensitivity of 99% and a negative predictive value of 98% in determining lymph node involvement. Scintigraphy and CT showed the same level of accuracy, 76.4%. CT findings had a higher positive predictive value but a lower negative predictive value compared to 99mTc-depreotide scintigraphy. The quantitative evaluation of depreotide uptake in lymph nodes using vertebra as a reference region showed that a cut-off level of 0.56 excludes malignant involvement of lymph nodes, while a cut-off level of 1.66 excludes benign disease in lymph nodes. About 73% of all investigated lymph node stations showed uptake values between these cut-off levels.
Conclusion
Absence of 99mTc-depreotide uptake on scintigraphic imaging can exclude regional lymph node involvement with a high degree of probability and may be useful in clinical practice. The quantitative evaluation of depreotide uptake in regional lymph nodes did not increase the diagnostic accuracy of the method in general but did elucidate the lymph node status in some patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is one of the most prevalent cancers and is the leading course of cancer mortality in Europe and the USA. In the year 2003, 2,900 new cases of lung cancer were diagnosed in Sweden, and about 10% of these patients attended our hospital. At the time of diagnosis the disease had spread beyond the primary site in most cases. There is a clear relationship between tumour stage and survival. Thus, patients with a small tumour without nodal or distant metastasis (stage 1A) have a 60–80% 5-year survival rate after surgery, whereas patients with metastatic disease have less than a 5% 5-year survival rate [1]. Tumour stage is one of the decisive prognostic parameters and is crucial in choosing the appropriate therapeutic option. Using anatomical imaging techniques, such as helical computed tomography (CT), the nodal (N-) status is based entirely on nodal size, which correlates unsatisfactorily with tumour involvement [2]. Thus other molecular/anatomical functional imaging techniques have attracted increasing interest during the past decade.
Positron emission tomography (PET) with 18F-2-fluoro-2-deoxy-d-glucose (FDG), which is based on the recognition of altered metabolism, has been used for tumour staging in countries with access to PET cameras. A meta-analysis of use of this imaging technique in the detection of nodal spread revealed a sensitivity of 83% and a specificity of 89% [3]. Several other tracers, such as 67Ga citrate and 99mTc-sestamibi, have previously been studied in the imaging of lung cancer, but these tracers are not in routine use owing to their low accuracy. Recently, a radiolabelled somatostatin analogue, 99mTc-depreotide (NeoSpect), was approved by The National Swedish Board of Health and Welfare for the evaluation of pulmonary nodules. A multi-centre trial including 114 patients with indeterminate lung nodules showed a high sensitivity (96.6%) of somatostatin receptor scintigraphy with 99mTc-depreotide with respect to lung cancer [4]. However, the significance of 99mTc-depreotide uptake for the N status of lung cancer has not been properly investigated, and the purpose of this study was to address this issue.
In order to evaluate the clinical usefulness of 99mTc-Depreotide scintigraphy in the assessment of nodal involvement (hilar, mediastinal, supraclavicular and axillary regions) in patients with lung cancer, we posed the following questions: How do the results of somatostatin receptor scintigraphy correlate with cytological/pathological and/or clinical evaluation of lymph node involvement? Which method, CT or somatostatin receptor scintigraphy, correlates best with N status? Could quantitative analysis of depreotide uptake be used to achieve more accurate differentiation between malignant and benign conditions in regional lymph nodes?
Materials and methods
Study population
The study started after approval had been obtained from the local ethical and radiation safety committees. A total of 99 patients with lung lesions detected using CT were prospectively investigated at our department using 99mTc-depreotide scintigraphy (GE Healthcare Bio-Sciences, Amersham Health AB, Sweden) between April 2003 and January 2004. Seven of them did not have primary lung cancer and will not be discussed further; six patients without a final diagnosis were also excluded. Thus 86 patients, 41 women and 45 men (mean age 64.7 years, median 65 years, range 31–83 years), were included.
CT imaging
CT was performed as a part of the routine assessment. In 71 patients it was performed up to 70 days before scintigraphy. In patients in whom CT was performed more than 2 months before scintigraphy, a new CT scan was ordered, and in 18 patients a repeat CT was performed within a maximum of 60 days after scintigraphy. CT and scintigraphy were performed within 30 days in 57 of the 86 patients. The CT scans were performed at our hospital (n=59) or at referring departments (n=27). At our hospital, CT scans were performed either with the multi-slice spiral CT Somatom Volume Zoom (Siemens, Erlangen, Germany), slice thickness 4×1 mm, pitch 1.5, or with the spiral CT single-slice Tomoscan AVE1 (Philips Medical Systems, Eindhoven, the Netherlands), slice thickness 5 mm, pitch 1.5. Images were reconstructed with 5-mm slice thickness for mediastinum and 10-mm slice thickness for the lungs. All scans were performed during a single breath-hold, following the intravenous injection of 120 ml contrast medium. The CT technique of the referring hospitals varied, but was essentially the same as that in our hospital. CT scans were assessed as part of a routine clinical evaluation by at least two radiologists, one of whom was a thoracic radiologist. The CT scans from the referring departments were double read by the thoracic radiologist from our department and the co-worker in this study, and this assessment was used for study evaluations. The presence, site and size of mediastinal, hilar, supraclavicular and axillary nodes were recorded according to the American Thoracic Society lymph node station mapping system. Lymph nodes with a diameter of less than 1 cm in the shortest axis were considered normal in size and those with a diameter of 1 cm or more were defined as pathological.
99mTc-depreotide imaging
99mTc-depreotide (740 MBq, 20 mCi) was administered in an antecubital vein. The examination was performed with a double-headed gamma camera (DST-XL, Sopha Medical Vision Scandinavia AB, GE, USA or E-Cam Siemens, Germany) with low-energy, ultra-high-resolution, parallel-hole collimators. All patients were first examined with whole-body scanning and then with single-photon emission computed tomography (SPECT) of the thorax 2–4 h after injection. The arms were elevated during the SPECT study and were placed alongside the body during whole-body scanning. SPECT data were acquired in a 128×128 matrix through 360° rotation with 64 projections. The acquisition time for each projection was 40 s. Transverse slices were reconstructed with an iterative algorithm (HOSEM Iterative program; Hermes/NUD; Stockholm, Sweden) and formatted as a 128×128 matrix without attenuation correction. Images were post-filtered with a 3D Fourier filter (Butterworth filter with a cut-off frequency of 0.65 cycles/cm, order 5). The scintigrams were evaluated along with CT by a team consisting of two specialists: one thoracic radiologist and one radiologist/nuclear medicine physician. CT was used since reading of the scintigrams requires anatomical landmarks provided by CT images. Such an interpretive approach provides more definitive localisation of the abnormal depreotide uptake.
Correlation between CT, scintigraphy and N status
The definitive diagnosis of the lung lesions was made by cytological (n=36) or histological (n=37) investigation or by clinical–radiological follow-up (n=13). In the last group of 13 patients, either resolution of lung lesions or disease progression was used as a criterion for definitive diagnosis upon repetition of radiological investigation after at least 6 months. The patient’s demographic and clinical–pathological characteristics are summarised in Table 1.
Lymph node involvement was determined by histological examination of pre-operatively sampled hilar and/or mediastinal nodes (thoracotomy or mediastinoscopy) or by cytology from fine-needle aspiration of supraclavicular or axillary nodes. Lymph nodes were dissected in two parts if they were less than 10 mm in diameter and each part was separately embedded and routinely stained with haematoxylin-eosin (HE) for light microscopic investigation. Besides routine staining, immunohistochemical (IHC) evaluation was performed in most cases in order to establish the origin of the metastatic involvement. An experienced pathologist interpreted the histological examinations of removed lymph nodes.
In patients with generally extended metastatic disease at the time of diagnosis and in those with a low probability of malignancy at first visit to the oncologist, no histological/cytological verification of lymph node involvement was performed. The N status in these cases was determined on the basis of the CT scan (size, existence of necrosis) and clinical–radiological (chest X-ray or CT) follow-up at our department at least 6 months after the initial CT and scintigraphy. A summary of the data concerning lymph node evaluation is presented in Table 2.
The results of 99mTc-depreotide scintigraphy were compared with those of CT with regard to the N status. Per site sensitivity, specificity, accuracy and positive and negative predictive values were determined for each procedure. These values were calculated twice: first for the group of 28 patients with cytological/histological verification of nodal status in 48 lymph node stations, and second for all 204 lymph node stations with the lymph node status determined by pathological examinations and also clinical–radiological follow-up. The first calculation is considered more accurate.
Quantitative analysis
The quantitative evaluation of depreotide uptake was made retrospectively after surgery. From surgical reports we collected information about which individual lymph node stations (the 1983 American Thoracic Society scheme was used) had been sampled, along with the results of histological or cytological examination of these lymph nodes.
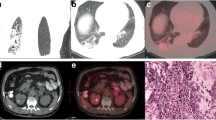
The quantitative evaluation of depreotide uptake in lymph nodes was made by SPECT in the 28 patients with cytological/histological verification of nodal status in 48 nodal stations. Of these patients, two were 45 and 49 years old, five were between 50 and 60 years old and 21 were older than 60 years. The median age of the 28 patients was 66 years. Because of its known low spatial resolution, scintigraphy cannot identify whether an increased 99mTc-depreotide uptake exists in one, two or more separate lymph nodes in each lymph node station. For this reason we analysed the correlation between depreotide uptake in lymph node stations and cytological or histological status irrespective of the number of metastatic lymph nodes in each station, e.g. if the histological examination revealed cancer involvement in one of three lymph nodes in paratracheal stations, the whole group was considered metastatic. The quantitative evaluation of thoracic lymph node uptake was made using regions of interest (ROIs) drawn on tomographic images over each lymph node station and for comparison over different reference areas: sternum, thoracic vertebra, lung parenchyma and spleen (Fig. 1). The reference areas were checked on corresponding CT scans for the absence of metastatic involvement. These ROIs contained identical pixel numbers. The tumour-to-reference ratio was calculated by dividing the tumour counts by the counts in the reference region. The absolute values varied considerably and we used the ratios instead of the absolute values.
Statistics
For two variables an extreme value might heavily influence and bias results; therefore a stratified Mann-Whitney test (non-parametric statistics) was performed and the p value calculated; p values less than 0.05 were considered significant. A chi-square test was used to analyse the association between size and diagnosis. The statistical measurement of agreement between the applied methods, e.g. 99mTc-depreotide scintigraphy or CT and cytological/histological N status, for the 48 lymph node stations was performed using Cohen’s kappa. The same approach was used to measure the agreement between these methods for all 204 investigated lymph node stations. Kappa values less than 0.40 indicate poor agreement, kappa values between 0.40 and 0.75, fair to good agreement, and kappa values above 0.75, strong agreement. Per site sensitivity, specificity, accuracy and positive and negative predictive values were determined for each applied procedure.
Results
Of the 86 patients included, 56 had malignant and 30 benign diagnoses. The histological subtypes of lung cancer for the aforementioned 56 patients are presented in Table 3, and the diagnoses in the 30 patients with benign lung lesions are presented in Table 4. Pathological depreotide uptake was seen in all but one patient with lung cancer and in several benign lesions. The patient with depreotide-negative bronco-alveolar carcinoma had no nodal involvement and no depreotide uptake in lymph nodes. Detailed discussion of depreotide uptake in lung lesions will be presented in a separate paper currently under preparation. The N status was determined for each patient on the basis of cytological (n=38), histological (n=20) or clinical–radiological findings (n=146). At the time of presentation, lymph node involvement was found in 39 of the 56 (70%) patients with lung cancer.
Correlation between CT, scintigraphy and N status
The correlation of 99mTc-depreotide scintigraphy and CT with cytological or histological nodal status of the 48 local/regional lymph node stations in 28 patients is presented in Table 5. 99mTc-depreotide scintigraphy had a sensitivity of 93.7% and a negative predictive value of 93.7% in determining lymph node involvement. Scintigraphy and CT showed almost the same level of accuracy, i.e. 62.5% and 64.5% respectively. CT findings had a lower positive predictive value and a lower negative predictive value compared to 99mTc-depreotide scintigraphy.
Lymph nodes in one station were slightly enlarged on CT and it was difficult to define the N status in this patient. This case was considered as “unclear, probably metastatic” by CT definition but was not metastatic in the subsequent cytological/histological examination. When defining the diagnostic accuracy of CT, this lymphatic station was graded as malignant in accordance with clinical practice (whereby malignancy is considered present until the opposite is proven). The same principle was used later when evaluating all 204 nodes.
The only false negative result on scintigraphy was seen in a patient with a poorly differentiated adenocarcinoma in the left upper lobe, with a diameter of 3 cm. There was high-intensity depreotide uptake in the primary tumour and absence of uptake in the hilar region. Histological examination of hilar lymph nodes revealed micro-metastases in one of two nodes.
The results of 99mTc-depreotide scintigraphy and CT findings in comparison with the N status for all 204 lymph node stations in all 86 patients, regardless of the examination method, are presented in Table 6.
False positive 99mTc-depreotide uptake was detected in 13 patients with benign lung diseases (39 lymph node stations): seven patients with pneumonia, one with pleural disease, two with sarcoidosis, one with a granuloma, one with round atelectasis and one with atelectasis. Moreover, eight patients with lung cancer showed 99mTc-depreotide uptake in lymph nodes whereas clinical–radiological N status (in two patients) or cytological/histological evaluation with routine HE staining (in six patients, with additional IHC evaluation in one of them) did not reveal metastatic spread to that nodal station. Three of these patients died within 6 months of diagnosis because of general disease progression, while five had no evidence of nodal involvement on plain X-ray examinations at follow-up after 12–16 months (only one of these patients underwent follow-up using CT).
There were 30 false positive diagnoses of nodal involvement on the CT scan. In addition, the nine unclear diagnoses were considered malignant until the opposite could be proven, and the total number of false positive results was thus 39. No metastases were found in the nine lymph node stations with an unclear CT diagnosis.
The diagnostic accuracy of 99mTc-depreotide scintigraphy and CT in the evaluation of N status is presented in Table 7. The statistical measurement of agreement between the applied methods (i.e. between 99mTc-depreotide scintigraphy or CT and cytological/histological diagnosis) for 48 lymph node stations, performed using Cohen’s kappa, showed a kappa value of 0.3 for scintigraphy and 0.2 for CT. The kappa value for all 204 lymph nodes in this study was 0.53 for scintigraphy and 0.54 for CT, which indicates that both methods showed poor agreement with microscopic examination and fair agreement with N status.
Quantitative analysis
In the group of 28 patients with cytological/histological verification of nodal status in 48 lymph node stations, lymph nodes with a short axis of less than 1 cm were found in 26 of the evaluated lymph node stations, while lymph nodes with a short axis of 1 cm or more were found in the remaining 22. Of the lymph nodes with a benign pathology, 67.7% were less than 1 cm in the shortest axis, while 70.5% of lymph nodes with a malignant pathology were 1 cm or more in the shortest axis.
A statistically significant difference in depreotide uptake was found between benign and metastatic lymph nodes for three reference regions, with p values of 0.009 for sternum, 0.003 for vertebra and 0.03 for spleen. The descriptive statistics for depreotide uptake in lymph nodes with different reference regions are presented for benign lymph node diseases in Table 8 and for metastatic lymph nodes in Table 9.
Using a thoracic vertebra as a reference region, there were no metastatic lymph nodes with depreotide uptake less than 0.56 and there were no benign lymph node diseases with an uptake of more than 1.66. Between these cut-off values there were 20 benign and 15 malignant lymph nodes. Thus, using these cut-off values, 72.9% of investigated lymph nodes had an “indeterminate” status, while N status was elucidated in about 27.1% of patients. For the sternum, a lower cut-off value of 0.61 and a higher cut-off value of 2.43 yielded 38 (79.1%) lymph nodes with an indeterminate status, while for the spleen, a lower cut-off value of 0.17 and a higher cut-off value of 0.84 yielded 37 (77%) lymph nodes with an indeterminate status.
Discussion
It is well known that radical surgery provides the only chance of a cure for lung cancer. However, if the cancer has extended to mediastinal lymph nodes, surgery is not generally applicable. Instead, chemotherapy and radiation therapy are used in different protocols. When distant metastases occur, only chemotherapy can be provided. These measures, however, are never curative.
The fact that somatostatin receptors are over-expressed in many malignant tumours provides the basis for differentiating malignant from other tissues by nuclear imaging using somatostatin receptor-binding radiotracers. There are a number of reports confirming the presence of somatostatin receptors on non-small cell lung cancer tumours and cell lines [5–7]. Thus, physiological imaging of somatostatin receptors with 99mTc-depreotide makes it possible to differentiate malignant from benign lesions in the lung. The metabolism and disposition of depreotide have not been studied in humans, and the normal biodistribution of 99mTc-depreotide, as well as its specific uptake in various pathological conditions, is not well documented. The normal variants include increased depreotide uptake in the spine, sternum and rib ends and low-level increased uptake in the hilar and mediastinal regions [8]. The diagnostic value of 99mTc-depreotide scintigraphy in the evaluation of solitary pulmonary nodules has been evaluated in a few studies [4, 9]. As the SPECT reconstruction volume includes both the primary lung lesion and regional lymph nodes, it is simple to assess information about both during the same imaging session.
Scintigraphic evaluation of regional lymph nodes displayed a high sensitivity (93.7–99%) in our study. The only false negative case was found in a patient with micro-metastatic involvement; this result could have been due to the limits of the technique in detecting a minimal tumour mass, and therefore somatostatin receptor scintigraphy seems less reliable in detecting minimal disease in mediastinal lymph nodes. Somewhat contradictory results were obtained in a trial by a Canadian group [10] who evaluated 99mTc-depreotide uptake in 260 regional lymph node stations in 51 patients with histologically proven lung cancer. Besides routine staining with HE, 100 lymph node stations with HE-negative readings were additionally tested with cytokeratin IHC stains. Overall sensitivity for hilar and/or mediastinal metastases was 95%, with a negative predictive value of 92%, which corresponds to our results. However, the rate of detection of micro-metastases was extremely high: 11 of 12 (92%) cases with proven micro-metastases were detected by depreotide. The differences in the findings of the two studies might be explained by the more frequent use of IHC by the Canadian group.
Another study performed on 166 subjects with suspected lung cancer, performed by Kahn et al. at the University of Iowa, showed a lower sensitivity (68%) and higher specificity (70%) than we found [11]. This difference can be explained by the selection of patients: only patients with operable and potentially curable lung cancer were enrolled, i.e. patients in the early stages of the disease. In the study from Iowa, 75% of patients were free from nodal involvement. Our situation was almost the opposite: 70% of our patients with lung cancer had extension to adjacent loco-regional lymph nodes at the time of presentation. Moreover, Kahn et al. compared depreotide uptake with 18F-FDG uptake on PET in patients with mediastinal involvement. The use of PET is still limited to a few hospitals in Sweden, while 30 different hospitals have nuclear medicine departments equipped with gamma cameras and can easily perform scintigraphy with depreotide.
The specificity of 99mTc-depreotide scintigraphy was poor in our cohort of patients, at ca. 45%. This is in accordance with the results from the Canadian group [10]. The large number of lymph nodes with false positive depreotide uptake has several possible explanations, one being the presence of inflammatory processes, and another the presence of somatostatin receptors in the vascular or bronchial walls [8, 11, 12].
The role of the regional lymph nodes in neoplasia in general and in metastasis in particular is as important as it is controversial. Unquestionably, the regional lymph nodes may be involved immunologically in the host response to neoplasms [13]. Tumour presence may stimulate the production and release of immunocompetent cells in the lymphoreticular system. The reaction commences in the regional lymph nodes, but later extends to distant nodes and the spleen.
It is well documented that somatostatin receptors are expressed on normal as well as activated monocytes, lymphocytes, lymphocytic leukaemia cells and lymphoid cell lines. Normal lymphocytes have low-affinity receptors; activated lymphocytes present somatostatin receptors with Kd values in the nanomolar range, which suggests that somatostatin receptor expression is related to activation and/or proliferation of these cells [14]. In previous studies, several radiolabelled somatostatin analogues have shown varying degrees of binding to haematopoietic cells, including lymphocytes, and this is also the case for depreotide [7]. There is still much research to be done, and one could assume that even depreotide uptake in lymphocytes might depend on their activation.
When comparing CT and depreotide scintigraphy, we found that neither correlated well with cytological/histological diagnosis and that both methods showed the same level of accuracy (76%). Enlargement of lymph nodes can be due to hyperplasia of lymph node follicles accompanied by proliferation of reticulum cells and sinus endothelium or active growth of tumour cells. CT findings, based on nodal size, i.e. a morphological criterion, have a higher positive predictive value than depreotide scintigraphy based on over-expression of somatostatin receptors. The absence of over-expression of somatostatin receptors is a more reliable non-morphological criterion for exclusion of malignant nodal extension. Thus, in patients with enlarged lymph nodes on CT, negative results of 99mTc-depreotide scintigraphy might exclude nodal spread.
Shih and Samayoa [15] evaluated the biodistribution of 99mTc-depreotide and made several observations: (1) the very faint uptake in normal lungs makes depreotide especially suitable for the detection of lung cancer, (2) the high intensity of radioactivity in the spleen can provide useful guidance for the categorisation of pulmonary lesions and (3) the mild uptake in the sternum and the thoracic vertebrae could be used as a landmark. The depreotide uptake in bone structures had the same level of intensity in all 29 investigated patients regardless of age. Age distribution in that study was 44–82 years, with an average age of 65.79 years, which is almost the same as in our cohort of patients. They further pointed out that depreotide imaging is similar to bone scintigraphy, but bone/bone marrow activity is much less than that on bone scan. We could not readily explain the exact mechanism of the 99mTc-depreotide uptake in these areas, but it may well be due to bone marrow uptake—which was constantly high in another study [16].
In the quantitative evaluation of lung lesions, both the normal lung parenchyma and thoracic vertebrae have been used as reference regions [14]. However, no data exist concerning quantitative evaluation of depreotide uptake in lymph nodes. We found some consistent similarities with respect to depreotide uptake in different reference regions: the sternum, vertebrae and spleen showed high depreotide uptake in all images, and all are considered normal variants by us and by others [8, 15]. The healthy lung parenchyma demonstrated very faint tracer uptake. The same pattern of depreotide uptake has been seen even in patients with benign lesions. As the sternum, vertebrae and spleen are easily delineated structures included in the reconstruction volume, all were used as reference regions. Since 21 of the 28 patients included in the quantitative evaluation were older than 60 years (the median age for all 28 patients was 66 years), we considered that there would not be substantial bias due to age. Moreover, all reference areas were checked on corresponding CT scans to exclude any metastatic involvement. The statistical analyses showed that sternum, thoracic vertebrae and spleen could be used as reference regions with statistically significant p values. When a thoracic vertebra was used as the reference region, a depreotide uptake value of >1.66 resulted in 100% specificity and a positive predictive value highly suggestive of metastatic involvement. In contrast, uptake values of less than 0.56 resulted in 100% sensitivity in excluding lymph node involvement. Twenty benign and 15 malignant lymph node stations were within the uptake range of 0.56–1.66. Using these cut-off values, 73% of the investigated lymph nodes had an “indeterminate” status, which would not be helpful in daily practice. On the other hand, 27% of patients had their N status elucidated by adding quantitative analysis. The practical situation when using the sternum and spleen as reference regions was similar: 79% and 77%, respectively, of lymph nodes were between cut-off values, and quantitative evaluation of these would not be helpful in determining the nature of the lymph nodes.
In conclusion, a negative result with scintigraphic imaging with 99mTc-depreotide can exclude cancer involvement of loco-regional lymph nodes with a high degree of probability and may be very useful in clinical practice. The quantitative evaluation of depreotide uptake in regional lymph nodes did not increase the diagnostic accuracy of the method in general but did elucidate the N status in some patients.
References
Mountain CF. Revisions in the international system for staging lung cancer. Chest 1997;111:1710–7.
Webb WR, Catsonis C, Zerhouni EA, Heelan RT, Glazer GM, Francis IR. CT and MR imaging in staging non-small cell bronchogenic carcinoma: report of the Radiologic Diagnostic Oncology Group. Radiology 1991;178:705–13.
Ho Shon I, O’ Doherty MJ, Maisey MN. Positron emission tomography in lung cancer. Semin Nuclear Med 2003;XXXII(4):240–71.
Blum J, Handmaker H, Lister-James J, Rinne N, NeoTect Solitary Pulmonary Nodule Study Group. A multicenter trial with a somatostatin analog 99m-Tc depreotide in the evaluation of solitary pulmonary nodules. Chest 2000;117:1232–8.
Reubi JC, Laissue J, Krenning EP, Lamberts SWJ. Somatostatin receptors in human cancer: incidence, characteristics, functional correlates and clinical application. J Steroid Biochem Mol Biol 1992;43:27–35.
O’Byrne KJ, Carney DN. Somatostatin and the lung. Lung Cancer 1993;10:151–72.
Virgolini I, Leimer M, Handmaker H, Lastoria S, Bischof C, Muto P, et al. Somatostatin receptor subtype specificity and in vitro binding of a novel tumour tracer, 99mTc-P829. Cancer Res 1998;58:1850–9.
Menda Y, Kahn D, Bushnell DL, Thomas M, Miller S, McLaughlin K, et al. Non-specific mediastinal uptake of 99m-Tc depreotide (NeoTect™). J Nucl Med 2001;42:304P.
Grewal RK, Dadparvar S, Yu JQ, Babaria CJ, Cavanaugh T, Sherman M, et al. Efficacy of Tc-99m depreotide scintigraphy in the evaluation of solitary pulmonary nodules. Cancer J 2002;8(5):400–4.
Tcherniantchouk O, Waxman AD, Williams CM, Kononov Y, Alsabeh R, ’Agnolo D, et al. Evaluation of hilar and mediastinal lymph nodes with Tc-99m depreotide in lung cancer: detection of micrometastases. J Nucl Med 2003;44:Suppl, abstract 440.
Kahn D, Menda Y, Kernstine K, Bushnell D, McLaughlin K, Miller S, et al. The utility of 99mTc depreotide compared with F-18 fluorodeoxyglucose positron emission tomography and surgical staging in patients with suspected non-small cell lung cancer. Chest 2004;125:494–501.
Menda Y, Khan D. Somatostatin receptor imaging of non-small cell lung cancer with 99m-Tc depreotide. Semin Nucl Med 2002;XXXII:92–6.
DeVita VT, Hellman S, Rosemberg SA. Cancer. Principles and practice of oncology. Philadelphia: J.B. Lippincott; 1982.
Van Hagen PM, Krenning EP, Kwekkeboom DJ, Reubi JC, Anker-Lugtenburg PJ, Löwenberg B, et al. Somatostatin and the immune and haematopoietic system; a review. Eur J Clin Investig 1994;24:91–9.
Shih W-J, Samayoa L. Tc-99m depreotide detecting malignant pulmonary nodules. Histopathologic correlation with semiquantitative tumour-to-normal lung ratio. Clin Nucl Med 2004;29:171–6.
Bushnell D, Menda Y, Madsen M, Link B, Kahn D, Truhlar S, et al. 99m-Tc-depreotide tumour uptake in patients with non-Hodgkin’s lymphoma. Nucl Med Commun 2004;25:839–43.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Danielsson, R., Bååth, M., Svensson, L. et al. Imaging of regional lymph node metastases with 99mTc-depreotide in patients with lung cancer. Eur J Nucl Med Mol Imaging 32, 925–931 (2005). https://doi.org/10.1007/s00259-005-1800-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-1800-5