Abstract
Neurofibromatosis type 1 (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis (SWN) are three clinically distinct tumor predisposition syndromes with a shared tendency to develop peripheral and central nervous system neoplasms. Disease expression and complications of NF1, NF2, and SWN are highly variable, necessitating a multidisciplinary approach to care in order to optimize outcomes. This review will discuss the imaging appearance of NF1, NF2, and SWN and highlight the important role that imaging plays in informing management decisions in people with tumors associated with these syndromes. Recent technological advances, including the role of both whole-body and localized imaging strategies, routine anatomic and advanced magnetic resonance (MR) imaging sequences such as diffusion-weighted imaging (DWI) with quantitative apparent diffusion coefficient (ADC) mapping, and metabolic imaging techniques (MR spectroscopy and positron emission testing) are discussed in the context of the diagnosis and management of people with NF1, NF2, and SWN based on the most up-to-date clinical imaging studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neurofibromatosis type 1 (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis (SWN) are three tumor predisposition syndromes that share a tendency to develop multiple peripheral and central nervous system (CNS) neoplasms (benign and malignant). Radiology plays a vital role in the diagnosis and management of people with these syndromes. Imaging is part of the diagnostic criteria in some way for all three syndromes (its role is most explicit for NF2 for the detection of bilateral vestibular schwannomas (VS), but implied in NF1 and SWN diagnostic criteria). Imaging is also emerging as a backbone of longitudinal surveillance strategies, and although its exact role is yet to be defined and at this time, there are no evidence-based guidelines for imaging applied to screening in NF1, NF2, or SWN.
There is currently limited evidence to support standard use of an imaging algorithm for the management of this patient population (people with NF1, NF2, or SWN), but there is an ever-increasing body of literature to guide imaging use. In this review, we present a systematic review of the literature and summarize current practices for magnetic resonance (MR) imaging for the evaluation of people with NF1, NF2, and SWN and when possible, provide guidelines for clinical practice based on the best available data. The review includes the role of both whole-body and localized imaging, standard anatomical imaging, as well as quantitative MR sequences such as diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) mapping, and metabolic imaging (MR spectroscopy (MRS) and positron emission testing). A discussion of existing data for potential imaging-based biomarkers (such as tumor burden and ADC values) in patients with NF1 for the early diagnosis of malignancy are presented and as are potential strategies for integration of WBMRI longitudinal findings with clinical and genetic characteristics.
Overview of NF1, NF2, and SWN
There are well-established clinical diagnostic criteria for NF1, NF2 and SWN (Table 1) [1,2,3,4]. Although, as more genetic discoveries are made and clinical experience is gained, there may be further refinement of these criteria.
The hallmark peripheral nerve sheath tumor (PNST) in NF1 is neurofibroma. Neurofibromas can be deep, involving single or multiple nerves. These are termed plexiform neurofibromas (pNF). There are also cutaneous neurofibromas (cNF) that involve the skin thickness and cases in which neurofibromas are diffuse and involve both the skin thickness and the deep nerves. pNF are estimated to occur in up to 50% of people with NF1. cNF impact up to 99% of adults with NF1. More rarely, there are atypical neurofibromas and malignant peripheral nerve sheath tumors.
The hallmark PNST in NF2 and SWN is schwannoma. Specifically, the presence of bilateral vestibular schwannomas (VS) is central to the diagnosis of NF2 and its absence in a patient with multiple schwannomas is suggestive of SWN or possibly mosaic NF2 [4,5,6]. In addition to schwannomas, patients with NF2 also tend to develop meningiomas and spinal ependymomas while patients with SWN rarely develop intracranial meningiomas and can develop cranial nerve schwannomas including unilateral VS, but do not develop bilateral VS [7].
On MR imaging, schwannomas tend to be fusiform masses with a “tail sign” suggesting its neurogenic origin and a “target sign” on fluid-sensitive and contrast-enhanced MR sequences related to their underlying cellular architecture (with myxoid Antoni B periphery and cellular Antoni A center accounting for the peripheral rim of hyperintensity and central hypointensity) [8,9,10]. Similarly, neurofibromas are also fusiform masses with a “tail sign” suggesting its neurogenic origin and a “target sign” on fluid-sensitive and contrast-enhanced sequences related to their underlying cellular architecture (due to dense collagenous center) [9, 10]. Larger schwannomas tend to be more heterogeneous with internal cystic degeneration, mineralization, hemorrhage, and fibrosis [10]. Solitary and syndromic schwannomas cannot be distinguished from one another by imaging or by histology, though SWN-associated schwannomas tend to exhibit greater perilesional edema, intralesional myxoid changes manifested as T2-hyperintensity and intraneural growth pattern compared with solitary schwannomas [11, 12]. In addition, people with NF2 and SWN tend to have multiple lesions throughout the body.
Table 2 summarizes the imaging appearance of syndromic PNSTs. Although each syndrome tends to have a different hallmark PNST, the MR appearance of both solitary and plexiform neurofibromas and schwannomas can overlap; therefore, the distribution and location of PNSTs in addition to presence or absence of CNS tumors such as spinal ependymomas, unilateral versus bilateral VS, or meningiomas, can inform the likelihood of an underlying PNST tumor syndrome. For example, intradermal schwannomas and spinal ependymomas appear to be unique to NF2 and help distinguish it from SWN. Similarly, an optic pathway glioma or thickening of the optic pathway paired with PNST is suggestive of NF1.
Technical considerations
The role of imaging in the management of patients with NF1, NF2, and SWN can be broadly conceptualized as directed towards the symptomatic or asymptomatic patient. The symptomatic patient typically undergoes localized imaging while the asymptomatic patient typically undergoes a detailed clinical assessment, preferably at an experienced NF clinic and in certain cases, may undergo whole-body imaging [13,14,15,16,17,18,19,20,21,22,23,24].
Localized imaging (including imaging of the extremities and CNS) can enable detection of PNST as the cause of underlying symptoms, characterization of PNST (as benign or malignant) and assessment of its anatomic extent (to assist with consideration of surgical approaches). Of course, people with NF1, NF2, and SWN can have non-PNST etiologies causing symptoms detected by localized MRI. Depending on the localization of the symptom and the total body tumor burden, localized imaging can also serve as a baseline exam to assess change in size and imaging characteristics for target, symptomatic PNSTs that are managed non-operatively. The imaging protocols for localized imaging can vary depending on the clinical suspicion. For example, in patients under consideration for NF2 and SWN, imaging of the CNS, specifically the internal auditory canals, using high-resolution post-contrast imaging, is routinely used for the detection of vestibular schwannomas (VS) as specified in the diagnostic criteria for this syndrome [1,2,3,4,5,6, 25]. In patients with NF1 with clinical suspicion for optic pathway glioma (OPG), MR imaging of the brain including orbits with and without intravenous contrast materials is the protocol of choice. For peripheral symptoms, localized MR imaging of the area of interest is performed with and without intravenous contrast for evaluation of anatomic extent. In addition, we perform a tailored localized MR imaging protocol using advanced sequences (DWI/ADC mapping and dynamic contrast-enhanced sequences) for simultaneous characterization of PNSTs as benign or malignant [26,27,28,29,30,31,32].
Whole-body imaging, typically whole-body magnetic resonance imaging (WB-MRI), can be utilized as a screening tool for internal tumor detection and when combined with DWI/ADC mapping can enable simultaneous tumor characterization [13]. The use of imaging for screening, particularly for asymptomatic people with NF1, is re-emerging as an important topic for several reasons including: the wider availability and speed of whole-body imaging techniques, the recognition that tumor growth and development of tumor-associated morbidity is most rapid in childhood and adolescence, the development of an increasing number of therapeutic agents that may have efficacy in stopping growth of neurofibromas and the documented development of MPNST in asymptomatic NF1 patients [17, 22, 33, 34]. Both whole-body MRI and 18F-fluorodeoxyglucose positron-emission tomography/ computed tomography (18F-FDG PET/CT) can detect whole-body internal tumor burden in a single imaging session. However, WB-MRI, due to its inherent contrast resolution, has been exploited as a method of choice for the detection of schwannomas and neurofibromas in patients with NF1, NF2, and SWN. WB-MRI is a feasible method of quantifying internal tumor burden in patients with NF1, NF2, and SWN, and therefore increasingly being utilized in clinical practice [13,14,15,16,17,18,19,20,21,22,23,24]. 18F-FDG PET/CT, an established technique for imaging oncological patients, is part of the imaging paradigm in patients with NF1 (no role in NF2 or SWN), particularly for the characterization of PNSTs as benign or malignant [26]. In our clinical practice, qualitative image interpretation of images acquired 60 min (rather than delayed imaging at 4 h) after the intravenous administration of 18F-FDG provides good clinical utility for distinguishing benign from malignant PNSTs (91% sensitivity and 84% specificity) in NF1 patients [26].
WB-MRI typically requires a 75-min time slot (although we budget 90 min) and can be performed with either 1.5- or 3-Tesla magnet systems [13]. The performance of WB-MRI at 3.0 Tesla has several theoretical advantages including higher signal-to-noise ratio and increased acquisition speed and disadvantages including B1 field inhomogeneities and susceptibility artifacts [13]. Although diverse methods of WB-MRI acquisition have been described, a two-dimensional (2D) short tau inversion recovery sequence (STIR) sequence, due to its robust fat suppression, is most commonly performed in the axial or coronal plane [13,14,15,16,17,18,19,20,21,22,23,24]. An alternative strategy includes performance of an isotropic volumetric three-dimensional (3D) STIR sequence in the coronal plane that enables multiplanar reformations in any plane of choice [13, 23, 24]. At this time, the proposed clinical indications for the performance of WB-MRI include the detection or quantification of internal peripheral nerve sheath tumors (PNSTs) burden in patients with NF1 (a potential marker for disease severity and risk for malignant transformation) and the detection (and distribution) of non-intradermal schwannomas in patients with a possible NF2 or SWN to establish the diagnostic criteria as well as surveillance of known PNST over time to determine the optimal time for treatment (many clinical trials have > 20% increase in tumor volume over 12–18 months as eligibility criteria) or surveillance while on treatment [13, 17, 22, 34, 35]. In a small subset of patients with NF1, NF2, or SWN, PNST burden is anatomically localized to a few adjacent spinal segments, single limb or even half of the body and referred to as a segmental phenotype. It is hypothesized that genetic mosaicism (when a postzygotic somatic mutation presents only in certain subset of cells), rather than a generalized phenotype due to a germline mutation, accounts for this segmental phenotype. By detecting the pattern and distribution of PNSTs, WB-MRI can be helpful in distinguishing a germline from segmental or mosaic presentation.
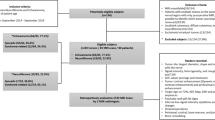
In our clinical practice, we perform WB-MRI with DWI/ADC mapping; Table 3 describes our 3.0-Tesla WB-MRI protocol. DWI is a fast, non-contrast, physiologic imaging technique that is readily available and easy to integrate into an existing localized or whole-body MR protocol [29, 31, 32]. DWI with ADC mapping offers a quantitative metric for the degree of cellularity of a region of interest [27,28,29,30,31,32]. Tissues with increased cellularity and resultant increased cell membranes lead to decreased Brownian motion or restricted diffusion, while tissues with decreased cellularity tend to have unrestricted or increased diffusion. The ADC value, representing a combination of both true diffusion and perfusion, is a numerical value assigned to this degree of motion in a tissue, and has been used as a marker for cellularity in soft tissue imaging [27,28,29,30,31,32]; regions of high ADC value correspond to hypocellular tissues and low ADC value are visible in hypercellular tissues. As such, the ADC value can serve as a useful biomarker for cellularity, often signifying malignancy, particularly useful tool for patients with NF1 who are at risk of developing MPNST [28, 29]. A comprehensive localized and whole-body imaging protocol with the inclusion of DWI/ADC mapping for the evaluation of PNSTs has been previously described [24, 28, 29]. The diagrams in Fig. 1 highlight the established and potential role of localized and whole-body imaging in patients with NF1, NF2, and SWN, emphasizing the nuanced alterations in imaging protocols based on clinical symptoms.
Neurofibromatosis type 1
NF1 is an autosomal dominant genetic syndrome caused by mutations in the NF1 gene, located at chromosome 17q11.2 [36] with an incidence of approximately 1 in 3000 individuals [37]. Approximately half of the cases are familial (inherited) while the other half are due to de novo (sporadic) mutations [37, 38]. The clinical manifestations of NF1 can be variable as there is extremely heterogeneous disease expression even within families with a shared mutation. Non-neoplastic manifestations (Fig. 1) of NF1 can affect the skin, CNS, cardiovascular system and the musculoskeletal system. The neoplastic manifestations of NF1 can be benign (including infiltrative (Fig. 2), solitary (Figs. 3 and 4), plexiform PNSTs), pheochromocytoma (Figs. 5), optic pathway glioma, pilocytic astrocytoma, gastrointestinal stromal tumors (GISTs) (Fig. 6), and glomus tumors (Fig. 7)) or malignant (including malignant peripheral nerve sheath tumors (MPNSTs), rhabdomyosarcomas, breast cancer, malignant glioma, and juvenile myelomonocytic leukemia (JMML)) [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59].
A 19-year-old woman with NF1. Axial T2-fat suppressed image (a) through the right calf shows skin thickening and reticular elevated signal in the subcutaneous tissues that extend along the superficial fascia with hypertrophy of the subcutaneous tissues consistent with cutaneous plexiform neurofibroma. On axial DWI images (b–d) through the calf with progressively increasing b-values and axial ADC map (e), this signal intensity does not exhibit restricted diffusion. Referral to multidisciplinary centers for the treatment of NF1-related symptoms and complications is recommended. Surgical treatment of such plexiform neurofibromas is often unsatisfactory and complete excision is not possible. Therefore, debulking alone of disfiguring or uncomfortable discrete cutaneous or subcutaneous neurofibromas is performed for improved cosmesis and symptom relief
A 12-year-old girl with NF1 and asymptomatic left pelvic mass. Axial T2-fat suppressed (FS) image through the pelvis (a) shows a left pelvic mass (arrow) with a target sign (low central and elevated peripheral signal) compatible with PNST. The target sign is commonly observed in benign PNSTs but rarely in malignancy. Axial ADC map (b) shows ADC values greater than 1.0 × 10–3 mm2/s. The post-contrast axial T1-FS image (c) through the pelvis shows heterogeneous targetoid pattern of enhancement. In localized MR imaging of PNSTs, ADC < 1.0 × 10–3 mm2/s and an average diameter of > 4.2 cm have been found to be useful cut-off values for diagnosing malignancy with 100% sensitivity and negative predictive value, thereby making the ADC value a useful, exploratory biomarker in the assessment of MPNST
An 18-year-old woman with NF1 and new left retropharyngeal mass (arrow) noted on axial T2-weighted image through the brain (a). Plexiform neurofibromas can increase in size dramatically per year in children with NF1, but have a slower growth rate at the end of adolescence; therefore, rapid growth of PNST in an adult can be a concerning clinical and imaging feature. Therefore, 18F-FDG-PET/CT imaging (b) was performed, which showed elevated FDG uptake (arrow). As such, the mass was biopsied and found to be neurofibroma with degenerative atypia but no necrosis, increased mitotic activity or other histological findings of malignant transformation. 18F-FDG-PET/CT has high sensitivity for the detection of malignant transformation in people with NF1 but lower specificity, potentially requiring unnecessary biopsies in patients with NF1
A 28-year-old man with NF1 and hyper-enhancing, submucosal masses (arrows) in the duodenum noted on an axial contrast-enhanced CT image through the abdomen compatible with malignant gastrointestinal stromal tumors. Note the several cutaneous neurofibromas and skin thickening in this patient with NF1
A 51-year-old man with neurofibromatosis type 1, who has progressive painful nodule on the radial and distal aspect of the right thumb. He had preoperative evaluation with an MRI, which showed a 3 × 3-mm nodule at the radial aspect of the thumb just distal to the interphalangeal joint (arrow) visible on axial T2 fat-suppressed (FS) (a), axial T1-FS (b), DWI using progressively increasing b-values (c–e) and ADC map (f). The lesion (arrow) is diffusely enhancing on the coronal MR angiogram (g) and static post-contrast T1-FS (h) through the thumb. The patient underwent surgical excision and final pathology was glomus tumor
A population-based series of 1404 Finnish patients with NF1 linked to incident cancers recorded in the Finnish Cancer Registry and deaths recorded in the national Population Register Centre from 1987 and 2012 estimated the overall lifetime cancer risk calculated to be as high as 59.6% [44]. In addition, patients with NF1 suffer from a lower life expectancy when compared with age-matched peers predominantly due to a relative increased likelihood of malignancies [44, 45], notably MPNST and breast cancer. Of these malignancies, MPNST has been identified as the most common cause of death in people with NF1 between the ages of 10 and 40 years with an estimated lifetime prevalence of 4–8% [44, 45, 53, 54]. The only treatment likely to result in cure is complete resection, which requires early detection. However, early detection of MPNST remains a clinical challenge in this patient population as the MPNSTs tend to be deep seated, limiting assessment by physical exam alone and often represent a needle in a haystack of myriad additional neurofibromas.
Current imaging strategies for NF1
The current approach to managing patients with NF1 is comprised of a comprehensive annual evaluation to detect and then treat symptomatic manifestations [8]. An important recent addition to formal imaging recommendations for people with NF1 is the recommendation for screening mammography to start at age 30 in women with NF1. Women with NF1 have a moderately elevated risk (17.2% lifetime risk) for breast cancer, especially under the age of 50 years [48,49,50,51]. Such data has resulted in modification of screening guidelines with the National Comprehensive Cancer Network recommending screening mammograms or MR imaging at the age of 30 years in this population [56, 57].
In addition to breast cancer, hypertension is a frequent finding in both adults and children with NF1 [58]. Therefore, monitoring blood pressure on a yearly basis is indicated. In children and young adults, or adults who do not achieve normalization of blood pressure with standard measures, evaluation for secondary causes of hypertension including pheochromocytoma or renovascular lesions including renal artery stenosis should be initiated [8, 55]. Other screening recommendations include annual ophthalmological examinations for symptomatic optic pathway glioma and review of growth and sexual development for hypothalamic dysfunction [60, 61]. When a symptomatic OPG is suspected, MR imaging of the brain with high-resolution sequences of the optic nerves and chiasm is the imaging technique of choice to detect OPG, assess its anatomic extent and eventually evaluate response to treatment or progression of disease. Because OPGs can exhibit variable contrast enhancement patterns, T2-weighted sequences are typically used but can pose a challenge for assessment of anatomic extent [61]. However, after baseline imaging for a symptomatic lesion, the optimal interval for surveillance is not established due to lack of evidence. OPG are only a clinical threat in childhood and if there is no progression based on imaging, visual or neuroendocrine symptoms by adolescence, imaging surveillance for OPG can likely be omitted in the absence of a specific clinical concern [62].
Routine baseline MR imaging of the entire CNS, and routine imaging of the chest, abdomen/pelvis and extremities to identify asymptomatic tumors are not recommended at this time [8]. Imaging studies of the CNS are generally reserved for NF1 patients with unexplained or progressive symptoms or new vision changes on ophthalmology evaluation. For the evaluation of symptoms (such as new pain, growth or severe/progressive polyneuropathy), typically localized MR imaging with advanced sequences including DWI/ADC mapping and DCE, is performed as above.
Whole-body imaging in NF1: Utility or futility?
The recommendations for the ongoing assessment and periodic surveillance of asymptomatic NF1 patients are narrow, with no consensus on how to evaluate for new or progressive PNSTs due to lack of evidence. Screening for MPNST that is comprised of physical exams alone is limited and challenging for deep or internal PNSTs which can manifest later, potentially with malignant conversion into MPNST which have high metastatic potential. NF1 patients that develop MPNSTs tend to be younger with a higher proportion of deep-seated or internal tumors and locally advanced disease at diagnosis [16, 17, 22, 63, 64]. Because both benign and malignant NF1-related PNSTs can be large both in individual size and number and often cross anatomic planes, whole-body imaging is an efficient method of tumor detection in a single session [13]. There are two whole-body imaging approaches in people with NF1: WB-MRI or 18F- FDG PET/CT. A major limitation to both WB-MRI and 18F- FDG PET/CT is the limited assessment of intraspinal neoplasms [65]. As such, depending on the clinical exam findings, performing whole-spine in addition to targeted MR imaging of the affected limb or body part may be an alternative diagnostic strategy, although the imaging time required to perform separate exams is greater than an optimized whole-body exam. Also, determining a target site to image based on physical exam alone may be challenging for deep internal PNSTs or in people with multiple symptoms. Whole-spine MR imaging alone can also miss a significant number of peripheral lesions that would otherwise be detected and quantified on whole-body imaging [65].
As such, if the neurologic examination does not suggest myelopathy and if there is a desire to assess the total body burden to establish a long-term surveillance plan for a given patient, WB-MRI is the preferred method in this patient population and enables detection and quantification of internal PNST burden [13,14,15,16,17,18,19,20,21,22,23,24]. One cross-sectional study with WB-MRI demonstrated internal PNSTs in 50% of NF1 patients [16], with the most common PNSTs being nodular and plexiform neurofibromas (pNF) [21]. The relationship between pNF size, total PNST burden, and the risk for MPNST is poorly understood. However, current clinical data suggest that patients who ultimately were diagnosed with MPNST had a higher baseline burden of pNF [21, 22], and anecdotally, MPNSTs commonly arise within a pNF (Fig. 8). Importantly, both higher numbers of PNSTs and larger whole-body tumor volume as detected by WB-MRI have been implicated as important risk factors for the development of MPNST [16, 21, 22]; hence, in the future, WB-MRI determined pNF burden may serve as a personalized MR-based biomarker for risk stratification and prognostication of patients with NF1.
WB-MRI in two asymptomatic patients with NF1. The first patient is a 14-year-old girl with NF1 with coronal short tau inversion recovery (STIR) sequences (a and b) showing superficial PNSTs (short arrows) in the posterior right upper back subcutaneous tissues. In people with NF1, the most common PNSTs are nodular and plexiform neurofibromas. A distinct growing nodular PNST located in the right infraclavicular region (long arrow on b) in the background of plexiform tumor and raised concern for malignant degeneration. Therefore, the lesion was excised and found to be neurofibroma with degenerative atypica. The PNST demonstrated areas of increased cellularity with scattered degenerative atypia and chronic inflammation. On histology, there was no increased mitotic activity, necrosis, significant crowding, or other features to suggest malignant transformation. An S100 immunostain showed diffuse labeling in the lesional cells. A second patient was a 12-year-old boy with NF1 with diffuse plexiform PNSTs visible on coronal STIR (c), ADC map (d), and static post contrast T1 fat-suppression (e) sequences. The relationship between plexiform neurofibroma size, total tumor burden, and the risk for MPNST is poorly understood. However, limited clinical data suggest that patients with MPNST have a higher baseline burden of plexiform neurofibroma
In addition to general internal pNF burden, there is emerging interest in atypical neurofibromas (aNFs) or “atypical neurofibromatous neoplasms of uncertain biologic potential (ANNUBP)”, which may represent precursor lesions to MPNSTs, and have been reported to have overlapping anatomic MR and metabolic imaging features with malignant PNSTs [64]. Recent work has recognized distinct nodular lesions (or DNLs) within pre-existing pNFs on standard anatomic MRI as potential precursor lesions to MPNST that may represent aNF/ANNUBP [64]. These DNLs tend to be greater than 3 cm in largest diameter, well demarcated, distinct from their underlying pNF, and lacking the typical histological, zonal architecture or target sign visible in PNSTs (defined as a central hypointense region on T2-weighted images) [64]. In a recent retrospective review of 76 histologically confirmed aNFs, all aNFs fulfilled the criteria for DNLs on MRI and 50 of 56 aNFs with available FDG-PET demonstrated elevated maximum standardized uptake value (SUVmax) (> 3.5), supporting the hypothesis that DNLs may be the imaging correlate of pre-malignant PNSTs [66]. Due to limited experience and available data, there are no specific or sensitive imaging features that aide in the distinction of atypical from malignant PNSTs, hence, the early identification of malignancy remains an important clinically relevant gap in the management of patients with NF1 [8].
When comparing the diagnostic performance of the two whole-body imaging strategies (18F-FDG-PET/CT versus WB-MRI using anatomic STIR sequences alone) for the detection of MPNST, metabolic imaging had superior sensitivity but lower specificity for the characterization of PNSTs as malignant [67]. Quantitative 18F-FDG -PET/CT scan characterizes NF1-related MPNSTs with high sensitivity (ranging from 89 to 95%) but relatively lower specificity (72–95%) [66,67,68,69,70,71,72,73,74,75]. At this time, a routine 18F-FDG -PET/CT protocol (without delayed imaging) has been recommended for patients with NF1 for the detection of suspected MPNST in a symptomatic patient [68]. In addition, PNST-to-liver ratio > 2.6, rather than the previously used SUVmax > 3.5, is recommended for diagnostic intervention planning as a more specific imaging indicator of MPNST 36). The performance of WB-MRI with the addition of DWI/ADC mapping has not been specifically compared to PET/CT in this population (Fig. 9). However, in localized imaging of solitary and syndromic PNSTs, ADC < 1.0 × 10−3 mm2/s and an average diameter of > 4.2 cm were useful cut-off values for diagnosing malignancy with 100% sensitivity and negative predictive value, thereby making the ADC value a valuable biomarker in the assessment of MPNST [29]. Importantly, in this study, all neurofibromas had ADC values greater than 1.0 × 10−3 mm2/s, making the ADC value highly specific and useful in the clinical context of NF1, as false-positive cases were only identified in schwannomas (n = 4) and ganglioneuromas (n = 1), but not in the setting of NF1-related neurofibromas, the tumors that are highest risk for malignant conversion [29]. As such, WB-MRI is increasingly being performed with the inclusion of DWI/ADC mapping in multiple clinical centers across the United States and Europe.
A 16-year-old boy with NF1 and pelvic MPNST visible on axial contrast-enhanced CT through the pelvis (a), axial T2 fat-suppressed (FS) (b), and static post-contrast T1-FS (c) imaging as a large left pelvic mass (arrow) just proximal to the sciatic foramen. Axial DWI using 3 b-values (d–f) and ADC maps (g) show ADC values < 1.0 × 10–3 mm2/s and size > 4.2 cm. In addition, 18F-FDG-PET/CT imaging (h) was performed which showed elevated FDG uptake. Therefore, the mass was biopsied and found to be MPNST. To date, there are no investigations exploring the interplay between cellularity (ADC values) and metabolic activity (SUVmax) in this population and if these may provide insight into the biologic behavior of PNSTs
Other advanced sequences such as MRS and MR angiography have also been applied to PNSTs for the purpose of characterization [31, 76]. Because altered cellular metabolism is typical of almost all malignancies, MRS, with its ability to noninvasively detect and characterize metabolites in a tissue of interest seems theoretically of interest for the early detection of MPNST. With respect to PNSTs, qualitative MRS has a high sensitivity (100%), but low specificity (50%) [76]. Quantitative MRS, a cumbersome technique with extensive post-processing time, has a slightly higher specificity (72.2%) for distinguishing benign from malignant disease for a perfect sensitivity of 100% [31, 76]. Due to technical requirements that would limit widespread applicability in the clinical centers around the world where patients with NF1 are cared for, neither MRS nor MR perfusion sequences have become part of a routine clinical care.
In summary, typically localized MR imaging of a pNF is performed based on clinical judgment (change in pain pattern or growth) to evaluate the anatomic extent and to serve as a baseline line exam to judge future growth and/or development of a “distinct nodular lesion,” which are suspected to undergo malignant degeneration. The optimal use, timing, or utility of a screening WB-MRI are not known. One group has recommended the performance of serial whole-body 18F-FDG-PET/CT imaging [63] for surveillance of MPNST. In our clinical practice at a high-volume NF1 center, we perform WB-MRI using DWI/ADC mapping in “high-risk” patients (NF1 gene microdeletion, family or personal history of aNF or MPNST, prior radiation therapy, high internal PNST burden) to detect and characterize internal PNST burden. Based on PNST size, preservation of zonal architecture “target sign” and ADC values, PNSTs are characterized as likely benign, suspicious but indeterminate (requiring localized imaging or close clinical/imaging follow-up) and highly suspicious for malignancy (requiring biopsy). Although this approach requires prospective validation, we anticipate that it may eventually lead to the development of a multi-parametric imaging reporting and data system (analogous to breast, prostate, and liver lesions) to determine the risk of malignancy associated with each PNST in a tumor syndrome. In addition, we also utilize WB-MRI in adolescents prior to transfer to adult care to establish baseline internal PNST burden as somatic growth maybe complete at this time.
Neurofibromatosis type 2
NF2 is an autosomal dominant genetic syndrome that is due to mutations in the NF2 gene, located at chromosome 22q12.2, and occurs in approximately 1 in 25,000 individuals [37]. Approximately half of the cases are familial (inherited) while the other half occur due to de novo (sporadic) mutations. Although clinically and genetically distinct from NF1, NF2 also suffers from an overall lower life expectancy when compared with non-affected peers [43]. It is characterized by bilateral vestibular schwannomas (VS) (Fig. 10) in addition to central and peripheral schwannomas. Although dermatologic involvement includes intradermal schwannomas, they are less common than the cutaneous neurofibromas in NF1. Most patients with NF2 eventually develop spinal tumors (paraspinal schwannomas, meningiomas, or intramedullary ependymomas) that can result in debilitating neurologic symptoms. Similar to NF1, patients with NF2 can also suffer from both mononeuropathy (often involving the facial nerve, which can precede the development of other NF2 manifestations) and severe and progressive polyneuropathy that is unrelated to PNSTs [77,78,79].
Current imaging strategies for NF2
Similar to NF1, patients with NF2 undergo routine ophthalmologic exam, thorough neurologic assessment for myelopathy as well as mononeuropathy, and audiology testing given their predisposition to bilateral VS [3, 5, 77,78,79,80]. Unlike NF1, imaging has a well-established role in the diagnosis and management of patients with NF2 [81]. Notably, MR imaging of the CNS is performed at baseline. MR imaging of the brain should include the administration of intravenous contrast material and axial and coronal thin-section imaging of the internal auditory canal (IAC) to assess for VS. Brain MRI with thin cuts through the IAC is recommended annually for almost all patients with NF2 and in many cases it is needed in a 3 to 6-month interval for people at high risk for brainstem compression or compromise of the facial or vestibular nerves [12]. MR imaging of the spine with contrast should also be performed given the predisposition to spinal ependymomas, schwannomas, and meningiomas, which are part of the National Institutes of Health (NIH) diagnostic criteria (Fig. 11) [6, 12, 78,79,80,81,82,83], however, the frequency of this imaging depends on the tumor burden and clinical exam findings. After establishing a diagnosis, patients with NF2 are closely monitored clinically and with imaging to assess for stability of the lesions as above [80]. After initial evaluation, surveillance with contrast-enhanced MR imaging of the brain and IACs (± spine if there are spinal lesions present) is performed in addition to every 6 to 12-month audiology testing and ophthalmological evaluation [12].
A 37-year-old woman with NF2. Coronal short tau inversion recover sequence (STIR) (a) and post contrast T1 fat-suppressed (FS) (b) images through the chest show two left brachial plexus peripheral neurogenic lesions and enhancing, intramedullary intraspinal lesions (short arrow on b) compatible with ependymoma. Most patients with NF2 eventually develop spinal tumors, which can result in debilitating neurologic symptoms. Intradermal schwannomas and spinal ependymomas are unique to NF2 and help distinguish the condition from schwannomatosis
Whole-body imaging in NF2: Utility or futility?
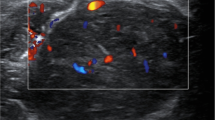
The potential WB-MRI uses in NF2 include detection and surveillance of non-intradermal schwannomas. There are two existing WB-MRI investigations in people with NF2 [9, 10]. The first such study in 55 patients with NF2 quantitatively assessed internal PNST burden and noted relatively lower internal PNST burden and volume in people with NF2 compared with NF1 and SWN [14]. Similar to NF1, patients with NF2 had scoliosis, likely due to spinal tumors but no other musculoskeletal abnormalities [14]. Interestingly, the presence of internal PNSTs correlated with scoliosis but not to established markers of disease severity including spinal tumors or meningiomas [14]. In addition, WB-PNST volume in NF2 patients inversely correlated with intradermal PNSTs, implying the importance of the tissue micro-environment in tumor formation [14]. The second smaller investigation on ten people with NF2 incorporated DWI/ADC mapping and described the imaging features of NF2 related PNSTs [23]. NF2-related PNSTs exhibited heterogeneous signal characteristics on routine anatomic and fluid-sensitive sequences as well as enhancement characteristics with a wide range of ADC values, suggesting heterogeneous tumor biology, differences in cellularity, and distribution of Antoni A and B patterns within each tumor (Fig. 12) [23].
A 50-year-old woman with NF2 and large right lumbosacral mass (long arrow) that is heterogeneous on coronal (a) and axial (b) T2 fat-suppressed (FS) and ADC map in addition to several intraspinal enhancing lesions (short arrows on b and c). Solitary and syndromic schwannomas in people with SWN or NF2 cannot be distinguished on imaging or histologically, though SWN-associated schwannomas tend to exhibit greater perilesional edema, intralesional myxoid change manifested as T2-hyperintensity, and intraneural growth pattern when compared with solitary schwannomas. MR imaging of the spine with contrast should be performed given the predisposition to spinal ependymomas, schwannomas, and meningiomas, which are also part of the National Institutes of Health (NIH) diagnostic criteria. Sagittal T1-FS post-contrast imaging through the lumbar spine (d) and axial T2- and T1-weighted images through the L5 level show two intraspinal lesions (short arrows on d) in addition to partially imaged peripheral mass (long arrow on e)
Both WB-MRI studies corroborate the variable disease expression among individuals with NF2 resulting in PNSTs of variable size, distribution, signal characteristics, and cellularity. Although NF2-related PNSTs tend to be benign, their anatomic location and multiplicity may contribute to both morbidity and mortality. Although there are no studies evaluating the imaging features predictive of lesions likely to be progressive or symptomatic, there is a correlation between internal tumor burden and quality of life [14]. As such, the early detection of high internal PNST burden using WB-MRI in people with NF2 may lead to active modification of treatment or closer surveillance for early intervention.
Notably, there are available data on the genotype–phenotype correlation, suggesting some markers of disease severity such as truncating mutations (frameshift and nonsense) of the NF2 gene predispose patients to greater disease-related mortality [80,81,82]. Conversely, people with constitutional NF2 missense mutations tend to have a lower risk of mortality than do those with other types of mutations [80]. Hence, a sub-population of patients with NF2 based on genetic testing may benefit from WB-MRI using DWI/ADC mapping for prediction of disease severity, or potentially, response to treatment. Unlike NF1, there is no reported predisposition to malignancy in NF2, and surveillance imaging for diagnosing malignant degeneration is not a clinical dilemma.
Schwannomatosis
Schwannomatosis, the third major form of PNST predisposition syndrome, is associated with mutations in the SMARCB1 and LZTR1 genes located on chromosome 22, and is therefore clinically and genetically distinct from both NF1 and NF2 [6, 83,84,85]. Although there is some diagnostic overlap between NF2 and SWN, SWN is characterized by the notable absence of bilateral VS or ependymoma and presence of multiple non-intradermal schwannomas, and less commonly, meningiomas [62]. Relative to NF1 and NF2, SWN is uncommon, with an estimated incidence of 1/40,000 births [86], but this number may be an underestimation, as the clinical presentation is nonspecific, resulting in a delay in diagnosis [86]. Although patients with SWN develop symptoms in the second or third decade of life, the median age of diagnosis is approximately 40 years [86]. SWN is most frequently sporadic, but approximately 20% of cases appear to be inherited, as defined by one or more closely related family members with at least one schwannoma [86].
In the largest case series to date that included 87 patients meeting criteria for SWN, pain, typically not associated with a mass, was the most common presenting symptom followed by a palpable abnormality [83]. A family history of SWN was present in only a small proportion of the patients [83]. Other symptoms reported at presentation varied depending on the anatomic location of the tumors, but included paresthesia, weakness, and atrophy [83]. The natural history of SWN is slowly being characterized, as it is a more recently recognized syndrome, and the limited available data do not suggest a decreased life expectancy; however there is a considerable decrease in the quality of life due to pain.
Current imaging strategies for SWN
Radiologists play a central role in the diagnosis of SWN, with high-resolution MR imaging of the brain, which is required to be performed with and without contrast, with thin cuts (< 3 mm and no interslice gap) through the IACs, to exclude bilateral VS and distinguish this entity form NF2 [12, 83]. On imaging, peripheral and CNS tumors are visualized, typically without bilateral VS, (although germline SMARCB1 and LZTR mutation associated SWN can present with a unilateral VS and multiple other cranial nerve schwannomas) [6]. The presence of multiple non-intradermal schwannomas in the absence of bilateral VS and ependymoma meets criteria for both NF2 and SWN and hence, in some cases the diagnosis cannot be made without detailed molecular testing of both tumor tissue and blood [86]. Localized MR imaging of the brain and spine are utilized routinely. MR imaging of the brain can detect non-vestibular cranial schwannomas and meningiomas and the absence of bilateral VS. In addition, MR imaging of the spine can reveal spinal schwannomas frequently, most commonly observed in the lumbar spine, followed by the thoracic spine, and cervical spine, and the notable absence of ependymoma.
Whole-body imaging in SWN: Utility or futility?
WB-MRI can play an important role in the diagnosis of patients with SWN for the detection of internal tumor burden [13,14,15, 24]. Both localized and WB-MRI can fulfill the presumptive diagnosis of SWN based on the NIH criteria by detection of a soft tissue mass with imaging appearance suggestive of PNST (Fig. 13) [15]. In the largest clinical study of patients with SWN, peripheral PNSTs, presumably schwannomas, were present in most patients, most commonly located in the extremities [15]. In these patients, WB-MRI enabled characterization of the anatomic extent or segmental distribution of disease [15]. In addition, WB-MRI data suggest that increased tumor volume in patients with SWN correlates with increasing age [15]. While intraspinal tumors are better assessed by localized MR imaging, other spinal manifestations have been described by WB-MRI, suggesting a small proportion of patients with SWN exhibit scoliosis without other skeletal complications such as pseudoarthrosis, sphenoid wing dysplasia, or bone cysts [15].
A 43-year-old woman with plexiform PNSTs in the left thigh (arrow) and left pelvis (arrow) visible on WB-MRI. The patient had no evidence of vestibular schwannoma (VS) on high-resolution imaging through the internal auditory canals and declined genetic testing. The presence of multiple non-intradermal schwannomas in the absence of bilateral VS and ependymoma meets diagnostic criteria for both mosaic NF2 and SWN, a limitation of the current diagnostic criteria
In a single WB-MRI investigation including DWI/ADC mapping in people with SWN, internal PNSTs exhibited similar imaging characteristics with heterogeneity on both non-contrast and contrast-enhanced sequences and variable ADC values ranging from 0.3 to 2.2 × 10−3 mm2/s [24]. Although a comparison between ADC values and SUVmax values was not performed, the SWN-related PNSTs ranged in SUV from 2.1 to 11.7, suggesting heterogeneity in the tumor micro-environment [24]. Given the high metabolic activity in benign PNSTs by 18F-FDG -PET/CT in SWN, WB-MRI with functional sequences is likely a more suitable technique for the assessment of disease burden, tumor characterization, and surveillance [24, 87, 88].
Unlike NF2, MPNSTs have been reported in patients with SWN; but, the overall lifetime risk is not well understood. In the largest cohort of SWN patients described to date, three out of 87 patients (3%) were misdiagnosed with MPNST (which were all reclassified on subsequent neuropathologic review as schwannoma or melanoma) [83]. Although the risk of SWN-related malignancy is not clear yet, there is a perceived increased risk in people with SWN associated with SMARCB1 mutations, and these patients may benefit form serial imaging using WB-MRI for the monitoring of peripheral lesions [24]. Importantly, the incorporation of DWI/ADC mapping in a WB-MRI protocol can be used to characterize PNSTS as benign or malignant in SWN [24].
Conclusions and future directions
In NF1, NF2, and SWN, emerging technical advances, particularly WB-MRI as well as DWI/ADC mapping, in conjunction with clinical and genetic data, can potentially provide insight into both disease severity as well as tumor behavior. In the future, these multi-parametric imaging tools may improve the diagnostic algorithm for disease surveillance and management based on the unique expression of an individual rather than the entire patient population. At this time, WB-MRI incorporating both anatomic sequences and DWI/ADC mapping is feasible and regularly utilized clinically in some centers for the assessment of people with NF1, NF2, and SWN, enabling simultaneous detection and characterization of peripheral lesions. The potential qualitative and quantitative biomarkers derived from WB-MRI, including WB PNST burden and ADC values, may also play an important role for prognostication of patients with these tumor predisposition syndromes in the future as additional data about the positive and negative predictive values of these techniques relative to various clinically meaningful endpoints (such as prevention of malignant conversion or neurologic disability) is determined. Future investigations, including the correlation of these imaging biomarkers with other clinical and genetic metrics to inform surveillance strategies, predict risk and outcomes and better prognosticate patients for more precise management. In the present, these approaches play a critical role in identifying these rare tumor syndromes and as a part of a multi-disciplinary surveillance program.
References
National Institutes of Health consensus development conference. Neurofibromatosis. Conference statement. Arch Neurol. 1988;45(05):575–8.
Mulvihill JJ, Parry DM, Sherman JL, Pikus A, Kaiser-Kupfer MI, Eldridge R. NIH conference. Neurofibromatosis 1 (Recklinghausen disease) and neurofibromatosis 2 (bilateral acoustic neurofibromatosis). An update. Ann Intern Med. 1990;113(01):39–52.
Baser ME, Friedman JM, Wallace AJ, Ramsden RT, Joe H, Evans DG. Evaluation of clinical diagnostic criteria for neurofibromatosis 2. Neurology. 2002;59(11):1759–65.
Plotkin SR, Blakeley JO, Evans DG, Hanemann CO, Hulsebos TJ, Hunter-Schaedle K, et al. Update from the 2011 International Schwannomatosis Workshop: from genetics to diagnostic criteria. Am J Med Genet A. 2013;161A(3):405–16.
Evans DG, King AT, Bowers NL, Tobi S, Wallace AJ, Perry M, et al. Identifying the deficiencies of current diagnostic criteria for neurofibromatosis 2 using databases of 2777 individuals with molecular testing. Genet Med. 2018.
Smith MJ, Bowers NL, Bulman M, Gokhale C, Wallace AJ, King AT, et al. Revisiting neurofibromatosis type 2 diagnostic criteria to exclude LZTR1-related schwannomatosis. Neurology. 2017;88(1):87–92.
Smith MJ, Kulkarni A, Rustad C, Bowers NL, Wallace AJ, Holder SE, et al. Vestibular schwannomas occur in schwannomatosis and should not be considered an exclusion criterion for clinical diagnosis. Am J Med Genet. 2012;158A(1):215–9.
Stewart DR, Korf BR, Nathanson KL, Stevenson DA, Yohay K. Care of adults with neurofibromatosis type 1: a clinical practice resource of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2018;20(7):671–82. https://doi.org/10.1038/gim.2018.28.
Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999;19(5):1253–80.
Bhargava R, Parham DM, Lasater OE, Chari RS, Chen G, Fletcher BD. MR imaging differentiation of benign and malignant peripheral nerve sheath tumors: use of the target sign. Pediatr Radiol. 1997;27(2):124–9.
Caltabiano R, Magro G, Polizzi A, Praticò AD, Ortensi A, D’Orazi V, et al. A mosaic pattern of INI1/SMARCB1 protein expression distinguishes schwannomatosis and NF2-associated peripheral schwannomas from solitary peripheral schwannomas and NF2-associated vestibular schwannomas. Childs Nerv Syst. 2017;33(6):933–40.
Plotkin SR, Wick A. Neurofibromatosis and schwannomatosis. Semin Neurol. 2018;38(1):73–85. https://doi.org/10.1055/s-0038-1627471.
Ahlawat S, Fayad LM, Khan MS, Bredella MA, Harris GJ, Evans DG, et al. Current whole-body MRI applications in the neurofibromatoses: NF1, NF2, and schwannomatosis. Neurology. 2016;87(7 Suppl 1):S31–9.
Merker VL, Bredella MA, Cai W, Kassarjian A, Harris GJ, Muzikansky A, et al. Relationship between whole-body tumor burden, clinical phenotype, and quality of life in patients with neurofibromatosis. Am J Med Genet A. 2014;164A(6):1431–7.
Plotkin SR, Bredella MA, Cai W, et al. Quantitative assessment of whole-body tumor burden in adult patients with neurofibromatosis. PLoS One. 2012;7:e35711.
Kluwe L, Nguyen R, Vogt J, et al. Internal tumor burden in neurofibromatosis type I patients with large NF1 deletions. Genes Chromosom Cancer. 2012;51:447–51.
Nguyen R, Kluwe L, Fuensterer C, Kentsch M, Friedrich RE, Mautner VF. Plexiform neurofibromas in children with neurofibromatosis type 1: frequency and associated clinical deficits. J Pediatr. 2011;159:652–655.e2.
Cai W, Kassarjian A, Bredella MA, et al. Tumor burden in patients with neurofibromatosis types 1 and 2 and schwannomatosis: determination on whole-body MR images. Radiology. 2009;250:665–73.
Van Meerbeeck SF, Verstraete KL, Janssens S, Mortier G. Whole-body MR imaging in neurofibromatosis type 1. Eur J Radiol. 2009;69:236–42.
Jaremko JL, MacMahon PJ, Torriani M, et al. Whole-body MRI in neurofibromatosis: incidental findings and prevalence of scoliosis. Skelet Radiol. 2012;41:917–23.
Mautner VF, Asuagbor FA, Dombi E, Fünsterer C, Kluwe L, Wenzel R, et al. Assessment of benign tumor burden by whole-body MRI in patients with neurofibromatosis 1. Neuro-Oncology. 2008;10(4):593–8.
Nguyen R, Jett K, Harris GJ, et al. Benign whole-body tumor volume is a risk factor malignant peripheral nerve sheath tumors in neurofibromatosis type 1. J Neuro-Oncol. 2014;116:307–13.
Fayad LM, Blakeley J, Plotkin S, Widemann B, Jacobs MA. Whole body MRI at 3T with quantitative diffusion-weighted imaging and contrast-enhanced sequences for the characterization of peripheral lesions in patients with neurofibromatosis type 2 and schwannomatosis. ISRN Radiol. 2013;2013:627932.
Ahlawat S, Baig A, Blakeley JO, Jacobs MA, Fayad LM. Multiparametric whole-body anatomic, functional, and metabolic imaging characteristics of peripheral lesions in patients with schwannomatosis. J Magn Reson Imaging. 2016;44(4):794–803.
Plotkin SR, Halpin C, Blakeley JO, Slattery WH 3rd, Welling DB, Chang SM, et al. Suggested response criteria for phase II antitumor drug studies for neurofibromatosis type 2 related vestibular schwannoma. J Neuro-Oncol. 2009;93(1):61–77.
Ahlawat S, Khandheria P, Del Grande F, Morelli J, Subhawong TK, Demehri S, et al. Interobserver variability of selective region-of-interest measurement protocols for quantitative diffusion-weighted imaging in soft tissue masses: comparison with whole tumor volume measurements. J Magn Reson Imaging. 2016;43(2):446–54.
Soldatos T, Ahlawat S, Montgomery E, Chalian M, Jacobs MA, Fayad LM. Multiparametric assessment of treatment response in high-grade soft-tissue sarcomas with anatomic and functional MR imaging sequences. Radiology. 2016;278(3):831–40.
Ahlawat S, Fayad LM. Imaging cellularity in benign and malignant peripheral nerve sheath tumors: utility of the “target sign” by diffusion-weighted imaging. Eur J Radiol. 2018;102:195–201. https://doi.org/10.1016/j.ejrad.2018.03.018.
Demehri S, Belzberg A, Blakeley J, Fayad LM. Conventional and functional MR imaging of peripheral nerve sheath tumors: initial experience. AJNR Am J Neuroradiol. 2014;35(8):1615–20.
Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology. 1988;168:497–505.
Fayad LM, Jacobs MA, Wang X, Carrino JA, Bluemke DA. Musculoskeletal tumors: how to use anatomic, functional, and metabolic MR techniques. Radiology. 2012;265(2):340–56.
Subhawong TK, Jacobs MA, Fayad LM. Diffusion-weighted MR imaging for characterizing musculoskeletal lesions. Radiographics. 2014;34(5):1163–77.
Gross AM, Singh G, Akshintala S, Baldwin A, Dombi E, Ukwuani S, et al. Association of plexiform neurofibroma volume changes and development of clinical morbidities in neurofibromatosis 1. Neuro-Oncology. 2018;20(12):1643–51.
Weiss B, Widemann BC, Wolters P, Dombi E, Vinks A, Cantor A, et al. Sirolimus for progressive neurofibromatosis type 1-associated plexiform neurofibromas: a neurofibromatosis clinical trials consortium phase II study. Neuro-Oncology. 2015;17(4):596–603. https://doi.org/10.1093/neuonc/nou235 Erratum in: Neuro Oncol. 2015 Jun;17(6):905.
Belasco JB, Schorry E, Brofferio A, Starosta AJ, Gillespie A, Doyle AL, et al. Activity of selumetinib in neurofibromatosis type 1-related plexiform neurofibromas. N Engl J Med. 2016;375(26):2550–60. https://doi.org/10.1056/NEJMoa1605943.
Fountain JW, Wallace MR, Bruce MA, Seizinger BR, Menon AG, Gusella JF, et al. Physical mapping of a translocation breakpoint in neurofibromatosis. Science. 1989;244(4908):1085–7.
Evans DG, Howard E, Giblin C, Clancy T, Spencer H, Huson SM, et al. Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family geneticregister service. Am J Med Genet A. 2010;152A(2):327.
Stephens K, Kayes L, Riccardi VM, Rising M, Sybert VP, Pagon RA. Preferential mutation of the neurofibromatosis type 1 gene in paternally derived chromosomes. Hum Genet. 1992;88(3):279–82.
Ruggieri M. Huson SM the clinical and diagnostic implications of mosaicism in the neurofibromatoses. Neurology. 2001;56(11):1433.
Seminog OO, Goldacre MJ. Risk of benign tumours of nervous system, and of malignant neoplasms, in people with neurofibromatosis: population-based record-linkage study. Br J Cancer. 2013;108(1):193–8.
Laycock-van Spyk S, Thomas N, Cooper DN, Upadhyaya M. Neurofibromatosis type 1-associated tumours: their somatic mutational spectrum and pathogenesis. Hum Genomics. 2011;5(6):623–90.
Miles DK, Freedman MH, Stephens K, Pallavicini M, Sievers EL, Weaver M, et al. Patterns of hematopoietic lineage involvement in children with neurofibromatosis type 1 and malignant myeloid disorders. Blood. 1996;88(11):4314–20.
Wilding A, Ingham SL, Lalloo F, et al. Life expectancy in hereditary cancer predisposing diseases: an observational study. J Med Genet. 2012;49(04):264–9.
Uusitalo E, Rantanen M, Kallionpää RA, Pöyhönen M, Leppävirta J, Ylä-Outinen H, et al. Distinctive cancer associations in patients with neurofibromatosis type 1. J Clin Oncol. 2016;34(17):1978–86.
Evans DG, Baser ME, McGaughran J, Sharif S, Howard E, Moran A. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39(5):311–4.
Sørensen SA, Mulvihill JJ, Nielsen A. Long-term follow-up of von Recklinghausen neurofibromatosis. Survival and malignant neoplasms. N Engl J Med. 1986;314(16):1010–5.
Walker L, Thompson D, Easton D, Ponder B, Ponder M, Frayling I, et al. A prospective study of neurofibromatosis type 1 cancer incidence in the UK. Br J Cancer. 2006;95(2):233–8.
Yap YS, Munusamy P, Lim C, Chan CHT, Prawira A, Loke SY, et al. Breast cancer in women with neurofibromatosis type 1 (NF1): a comprehensive case series with molecular insights into its aggressive phenotype. Breast Cancer Res Treat. 2018. https://doi.org/10.1007/s10549-018-4851-6.
Wang X, Teer JK, Tousignant RN, Levin AM, Boulware D, Chitale DA, et al. Breast cancer risk and germline genomic profiling of women with neurofibromatosis type 1 who developed breast cancer. Genes Chromosom Cancer. 2018;57(1):19–27. https://doi.org/10.1002/gcc.22503.E.
Howell SJ, Hockenhull K, Salih Z, Evans DG. Increased risk of breast cancer in neurofibromatosis type 1: current insights. Breast Cancer (Dove Med Press). 2017;9:531–6.
Seminog OO, Goldacre MJ. Age-specific risk of breast cancer in women with neurofibromatosis type 1. Br J Cancer. 2015;112(9):1546–8. https://doi.org/10.1038/bjc.2015.78.
Duong TA, Sbidian E, Valeyrie-Allanore L, et al. Mortality associated with neurofibromatosis 1: a cohort study of 1895 patients in 1980-2006 in France. Orphanet J Rare Dis. 2011;6:18.
Poyhonen M, Niemela S, Herva R. Risk of malignancy and death in neurofibromatosis. Arch Pathol Lab Med. 1997;121(2):139–43.
Kumar MG, Emnett RJ, Bayliss SJ, Gutmann DH. Glomus tumors in individuals with neurofibromatosis type 1. J Am Acad Dermatol. 2014;71(1):44–8. https://doi.org/10.1016/j.jaad.2014.01.913.
Shinall MC, Solórzano CC. Pheochromocytoma in Neurofibromatosis type 1: when should it be suspected? Endocr Pract. 2014;20(8):792–6. https://doi.org/10.4158/EP13417.
Evans DG. Are we ready for targeted early breast cancer detection strategies in women with NF1 aged 30-49 years? Am J Med Genet A. 2012;158a:3054–5.
Daly MB, Pilarski R, Berry M, Buys SS, Farmer M, Friedman S, et al. NCCN guidelines insights: genetic/familial high-risk assessment: breast and ovarian, version 2.2017. J Natl Compr Cancer Netw. 2017;15(1):9–20.
Dubov T, Toledano-Alhadef H, Chernin G, Constantini S, Cleper R, Ben-Shachar S. High prevalence of elevated blood pressure among children with neurofibromatosis type 1. Pediatr Nephrol. 2016;31(1):131–6. https://doi.org/10.1007/s00467-015-3191-6.
Valentin T, Le Cesne A, Ray-Coquard I, et al. Management and prognosis of malignant peripheral nerve sheath tumors: the experience of the French Sarcoma Group (GSF-GETO). Eur J Cancer. 2016;56:77–84.
Sani I, Albanese A. Endocrine long-term follow-up of children with neurofibromatosis type 1 and optic pathway glioma. Horm Res Paediatr. 2017;87(3):179–88. https://doi.org/10.1159/000458525.
Gaudino S, Quaglio F, Schiarelli C, Martucci M, Tartaglione T, Gualano MR, et al. Spontaneous modifications of contrast enhancement in childhood non-cerebellar pilocytic astrocytomas. Neuroradiology. 2012;54:989–95.
de Blank PMK, Fisher MJ, Liu GT, Gutmann DH, Listernick R, Ferner RE, et al. Optic pathway gliomas in Neurofibromatosis type 1: an update: surveillance, treatment indications, and biomarkers of vision. J Neuroophthalmol. 2017;37(Suppl 1):S23–32. https://doi.org/10.1097/WNO.0000000000000550 Review.
Azizi AA, Slavc I, Theisen BE, Rausch I, Weber M, Happak W, et al. Monitoring of plexiform neurofibroma in children and adolescents with neurofibromatosis type 1 by [(18) F]FDG-PET imaging. Is it of value in asymptomatic patients? Pediatr Blood Cancer. 2018;65(1). https://doi.org/10.1002/pbc.26733.
Meany H, Dombi E, Reynolds J, Whatley M, Kurwa A, Tsokos M, et al. 18-fluorodeoxyglucose-positron emission tomography (FDG-PET) evaluation of nodular lesions in patients with neurofibromatosis type 1 and plexiform neurofibromas (PN) or malignant peripheral nerve sheath tumors (MPNST). Pediatr Blood Cancer. 2013;60(1):59–64.
Zhang L, Dessouky R, Xi Y, Chhabra A, Le LQ. Clinical value of multiparametric whole-body magnetic resonance imaging over whole-spine magnetic resonance imaging in patients with neurofibromatosis type I. World Neurosurg. 2017;108:729–37.
Higham CS, Dombi E, Rogiers A, Bhaumik S, Pans S, Connor SEJ, et al. The characteristics of 76 atypical neurofibromas as precursors to neurofibromatosis 1-associated malignant peripheral nerve sheath tumors. Neuro-Oncology. 2018;20(6):818–25.
Derlin T, Tornquist K, Münster S, Apostolova I, Hagel C, Friedrich RE, et al. Comparative effectiveness of 18F-FDG PET/CT versus whole-body MRI for detection of malignant peripheral nerve sheath tumors in neurofibromatosis type 1. Clin Nucl Med. 2013;38(1):e19–25.
Chirindel A, Chaudhry M, Blakeley JO, Wahl R. 18F-FDG PET/CT qualitative and quantitative evaluation in neurofibromatosis type 1 patients for detection of malignant transformation: comparison of early to delayed imaging with and without liver activity normalization. J Nucl Med. 2015;56(3):379–85. https://doi.org/10.2967/jnumed.114.142372.
Ferner RE, Lucas JD, O’Doherty MJ, et al. Evaluation of 18fluorodeoxyglucose positron emission tomography (18FDGPET) in the detection of malignant peripheral nerve sheath tumours arising from within plexiform neurofibromas in neurofibromatosis 1. J Neurol Neurosurg Psychiatry. 2000;68:353–7.
Cardona S, Schwarzbach M, Hinz U, Dimitrakopoulou-Strauss A, Attigah N, Mechtersheimer G, et al. Evaluation of F18-deoxyglucose positron emission tomography (FDG-PET) to assess the nature of neurogenic tumours. Eur J Surg Oncol. 2003;29:536–41.
Bredella MA, Torriani M, Hornicek F, Ouellette HA, Palmer WE, Williams Z, et al. Value of PET in the assessment of patients with neurofibromatosis type 1. AJR Am J Roentgenol. 2007;189:928–35.
Ferner RE, Golding JF, Smith M, Calonje E, Jan W, Sanjayanathan V, et al. [18F]2-fluoro-2-deoxy-d-glucose positron emission tomography (FDG PET) as a diagnostic tool for neurofibromatosis 1 (NF1) associated malignant peripheral nerve sheath tumours (MPNSTs): a long-term clinical study. Ann Oncol. 2008;19(2):390–4.
Warbey VS, Ferner RE, Dunn JT, Calonje E, O’Doherty MJ. [18F]FDG PET/CT in the diagnosis of malignant peripheral nerve sheath tumours in neurofibromatosis type-1. Eur J Nucl Med Mol Imaging. 2009;36(5):751–7.
Salamon J, Veldhoen S, Apostolova I, et al. 18F-FDG PET/CT for detection of malignant peripheral nerve sheath tumours in neurofibromatosis type 1:tumour-to-liver ratio is superior to an SUVmax cut-off. Eur Radiol. 2014;24:405–12.
Urban T, Lim R, Merker VL, et al. Anatomic and metabolic evaluation of peripheral nerve sheath tumors in patients with neurofibromatosis 1 using whole-body MRI and (18)F-FDG PET fusion. Clin Nucl Med. 2014;39:e301–7.
Fayad LM, Wang X, Blakeley JO, Durand DJ, Jacobs MA, Demehri S, et al. Characterization of peripheral nerve sheath tumors with 3T proton MR spectroscopy. AJNR Am J Neuroradiol. 2014;35(5):1035–41.
Friedman JM. Neurofibromatosis 1. 1998 Oct 2 [updated 2018 May 17]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, LJH B, Stephens K, Amemiya A, editors. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2018. Available from http://www.ncbi.nlm.nih.gov/books/NBK1109/PubMed.
Evans DG. Neurofibromatosis 2 [bilateral acoustic neurofibromatosis, central neurofibromatosis, NF2, neurofibromatosis type II]. Genet Med. 2009;11(9):599–610.
Evans DG. Neurofibromatosis 2. 1998 Oct 14 [updated 2018 mar 15]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, LJH B, Stephens K, Amemiya A, editors. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2018.
Baser ME, Friedman JM, Aeschilman D, et al. Predictors of the risk of mortality in neurofibromatosis 2. Am J Hum Genet. 2002;71:715–23.
Patronas NJ, Courcoutsakis N, Bromley CM, Katzman GL, MacCollin M, Parry DM. Intramedullary and spinal canal tumors in patients with neurofibromatosis 2: MR imaging findings and correlation with genotype. Radiology. 2001;218:434–42.
Dow G, Biggs N, Evans G, Gillespie J, Ramsden RT, King A. Spinal tumors in neurofibromatosis type 2: is emerging knowledge of genotype predictive of natural history? J Neurosurg Spine. 2005;2:574–9.
Merker VL, Esparza S, Smith MJ, Stemmer-Rachamimov A, Plotkin SR. Clinical features of schwannomatosis: a retrospective analysis of 87 patients. Oncologist. 2012;17(10):1317–22.
MacCollin M, Chiocca EA, Evans DG, Friedman JM, Horvitz R, Jaramillo D, et al. Diagnostic criteria for schwannomatosis. Neurology. 2005;64(11):1838–45.
Kehrer-Sawatzki H, Kluwe L, Friedrich RE, Summerer A, Schäfer E, Wahlländer U, et al. Phenotypic and genotypic overlap between mosaic NF2 and schwannomatosis in patients with multiple non-intradermal schwannomas. Hum Genet. 2018. https://doi.org/10.1007/s00439-018-1909-9.
Evans DG, Bowers NL, Tobi S, Hartley C, Wallace AJ, King AT, et al. Schwannomatosis: a genetic and epidemiological study. J Neurol Neurosurg Psychiatry. 2018;89:1215–9.
Lieber B, Han B, Allen J, Fatterpekar G, Agarwal N, Kazemi N, et al. Utility of positron emission tomography in schwannomatosis. J Clin Neurosci. 2016;30:138–40. https://doi.org/10.1016/j.jocn.2016.01.027.
Beylergil V, Haque S, Carver A, Bilsky MH, Carrasquillo JA. Schwannomatosis/ neurofibromatosis type 2 associated multiple schwannomas visualized on FDG-PET/CT. Rev Esp Med Nucl Imagen Mol. 2013;32(4):275–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahlawat, S., Blakeley, J.O., Langmead, S. et al. Current status and recommendations for imaging in neurofibromatosis type 1, neurofibromatosis type 2, and schwannomatosis. Skeletal Radiol 49, 199–219 (2020). https://doi.org/10.1007/s00256-019-03290-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03290-1