Abstract
Objective
Our aims were to investigate the imaging appearance of subchondral insufficiency fracture (SIF) of the femoral head based on fat-suppressed T2-weighted MRI, and evaluate its correlation with the clinical outcomes following conservative treatment.
Materials and methods
We retrospectively evaluated 40 hips in 37 patients with SIF of the femoral head (12 males and 25 females; mean age 55.8 years, range 22–78 years). MRI examinations were performed within 3 months after the onset of hip pain. Using fat-suppressed T2-weighted imaging, we evaluated the hips for the intensity of the subchondral bone (corresponding to the area superior to the low intensity band on T1-weighted images) as well as bone marrow edema, joint effusion, and presence of the band lesion. We then correlated the intensity of the subchondral bone with clinical outcomes.
Results
The hips were classified into three types based on subchondral intensity on fat-suppressed T2-weighted images: type 1 (21 hips) showed high intensity, type 2 (eight hips) showed heterogeneous intensity, and type 3 (11 hips) showed low intensity. The mean period between pain onset and MRI examination was significantly longer for type 2 hips than for type 1. Healing rates were 86 % for type 1, 75 % for type 2, and 18 % for type 3.
Conclusion
SIF cases were classified into three types based on subchondral intensity on fat-suppressed T2-weighted imaging performed within 3 months after pain onset. Type 3 SIF tended to be intractable to conservative treatment compared to type 1 and type 2.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Subchondral insufficiency fracture (SIF) of the femoral head has been recognized as one cause of acute hip pain [1–5]. Some reported cases of SIF of the femoral head have progressed to collapse, necessitating surgery, whereas others have resolved with conservative treatment [1–3, 6]. T1-weighted magnetic resonance imaging (MRI) has been used to diagnose SIF. A subchondral low-intensity band on T1-weighted images is reported to be characteristic in SIF. This band has been described as irregular, disconnected, and parallel to the articular surface, and histopathologically it corresponds to the fracture itself [2, 3, 7, 8].
The imaging appearance of SIF in other sequences, such as fat-suppressed T2-weighted imaging, has not been described in detail. A few authors have described the varying intensity of subchondral lesions on fat-suppressed T2-weighted imaging [3, 7, 9], but no consensus on the significance of lesion intensity has been reached. Yamamoto et al. [7] reported that subchondral lesions (proximal to the low intensity band on T1-weighted images) showed high intensity in six of seven hips with SIF, whereas Davis et al. [9] reported that this area showed only low intensity in all of their five reported hips. Because the intensity of the fracture site changes over time [10], we hypothesized that these differences in intensity derive from different statuses of the fracture site and are associated with the clinical outcomes.
In this study, we investigated the imaging appearance of SIF of the femoral head on fat-suppressed T2-weighted images with special emphasis on the intensity of the subchondral lesions and their correlation with the clinical outcomes following conservative treatment.
Materials and methods
Patients
Our institutional review board approved this study. We retrospectively reviewed the records of 57 hips in 54 consecutively registered patients who were diagnosed with SIF of the femoral head at our institution between August 2009 and April 2015. The SIF diagnosis was based on the following published criteria: acute onset of hip pain with no apparent history of trauma; normal radiographic findings or radiographs showing femoral head collapse and/or a linear patchy sclerotic area in the superior portion of the femoral head; and bone marrow edema in the femoral head with a typical low intensity band (irregular, disconnected, and parallel to the articular surface) in the subchondral area on T1-weighted MRI [2, 3, 7, 11]. In some cases, gadolinium-enhanced MRI was also performed to differentiate SIF from avascular necrosis (AVN) of the femoral head [12]. We excluded four hips for which the MRI examination was performed more than 3 months after pain onset and 13 hips that already showed joint space narrowing (<2 mm) indicative of osteoarthritis [13]. MRIs obtained from 40 hips in 37 patients were included in the study. The patients included 12 males and 25 females with a mean age of 55.8 years (range 22–78 years). The mean period between the onset of hip pain and the MRI examination was 1.4 months (range 0.2–2.9 months). The mean follow-up period was 21.2 months (range 3.0–68.3 months).
MRI assessment
MRI examinations were performed on a 3-T system (Achieva 3.0T; Philips Healthcare, Best, The Netherlands). Coronal and axial turbo spin-echo T1-weighted images [repetition times/echo times (TR/TE): 400−650/10−20 ms] and coronal and axial fat-suppressed turbo spin-echo T2-weighted images (TR/TE: 3000−3600/80−100 ms) were acquired with the patient in supine position. All sequences used a 5-mm slice thickness with 1-mm interslice gap and a field of view of 360 × 360 mm.
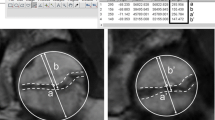
On T1-weighted images, we confirmed both bone marrow edema and a typical low intensity band (irregular, disconnected, and parallel to the articular surface) [2, 3, 7, 11]. The band lesion size was also evaluated with the band length ratio, which was measured on the coronal slice through the center of the femoral head on T1-weighted images using a previously reported method (Fig. 1) [6]. Briefly, this ratio represents the band length relative to the weight-bearing portion. The weight-bearing portion of the femoral head was defined as the area lateral to the mid-vertical line through the acetabular edge and the bottom of the teardrop.
The band length ratio on the T1-weighted image. Arcs A and B indicate the weight-bearing portion of the femoral head and the length of the low intensity band. The weight-bearing portion of the femoral head is defined as the area lateral to the mid-vertical line through the acetabular edge and the teardrop. The band length ratio is given by (B/A)
On fat-suppressed T2-weighted images, we evaluated the intensity of the subchondral bone (corresponding to the area superior to the low intensity band on T1-weighted images), bone marrow edema, joint effusion, and presence of the band lesion. Presence of the band and the intensity of the subchondral bone were evaluated on coronal slices in which a low intensity band had been detected on the T1-weighted images. Bone marrow edema and joint effusion were evaluated on the coronal slice through the center of the femoral head. Joint effusion was considered positive when it distended the joint capsule [14].
Clinical management
After diagnosis, all patients initially underwent conservative treatment comprising rest and restricted weight-bearing for 6 weeks. Radiography was performed 2, 4, 6, and 12 weeks after the start of treatment and compared with radiographs obtained at diagnosis to evaluate the progression of femoral head collapse. Based on the anteroposterior and frog-leg lateral view radiographs, radiographic femoral head collapse was evaluated using concentric circles. If collapse progressed by more than 1 mm during conservative treatment, the indication for surgical treatment was evaluated comprehensively in light of difficulty with activities of daily living resulting from loss of hip function and the patient’s preferences. Follow-up was continued until at least the time at which the hips became asymptomatic.
Twenty-six hips (65 %) showed no progression of radiographic femoral head collapse and obtained relief from pain without surgical treatment at final follow-up; these hips were categorized as the resolution group. The other 14 hips (35 %) showed progression of femoral head collapse during conservative treatment; these hips were categorized as the non-resolution group. Eight of the 14 non-resolution hips underwent surgical treatment. Four hips in three patients younger than 40 years that had an intact area in the posterior portion of the femoral head underwent transtrochanteric anterior rotational osteotomy, while the other four hips in four patients underwent total hip arthroplasty.
Histopathological assessment
In the eight hips that received surgical treatment, either bone biopsy specimens or the resected femoral heads were obtained. For these hips, histopathologic findings were correlated with findings on fat-suppressed T2-weighted images. However, two hips in which the specimen was obtained more than 3 months after MRI examination were excluded from this evaluation because the specimen would not reflect the lesion’s condition at the time of MRI examination.
Statistical analysis
We correlated the intensity of the subchondral bone on fat-suppressed T2-weighted images with clinicoradiological factors, including age, sex, body mass index, period between pain onset and MRI examination, presence of radiographic femoral head collapse at diagnosis, and the band lesion size on T1-weighted images. Regarding radiographic femoral head collapse at the time of diagnosis, we described the hips as slightly collapsed (collapse <2 mm) or severely collapsed (collapse ≥2 mm). We also examined the clinical outcome (the resolution rate) according to the intensity of the subchondral bone.
Continuous variables are expressed as means with standard deviations. Differences between groups were examined with logistic regression analysis for continuous variables and Fisher’s exact probability test for categorical variables. A value of p < 0.05 was considered to indicate significance.
To test the reproducibility of evaluating the intensity of the subchondral bone, the images were independently reviewed by two of the authors who specialize in the diagnosis and treatment of SIF and who were unaware of clinical data. In addition, one author reviewed the images a second time after an interval of 1 month. Intra- and inter-observer agreements of the intensity of the subchondral bone were analyzed with the kappa coefficient [15]. These statistical analyses were performed using JMP statistical analysis software (version 11; SAS Institute, Cary, NC, USA).
Results
Appearance of SIF on fat-suppressed T2-weighted images
On fat-suppressed T2-weighted images, all 40 hips showed bone marrow edema, and 37 hips (93 %) had joint effusion (Table 1). A low intensity band was detected in the bone marrow edema in 34 hips (85 %), which corresponded to the band that appeared on T1-weighted images (fracture line). There was no apparent band in the other six hips (15 %). The mean period between the onset of hip pain and MRI examination tended to be longer for patients with a band than in those without a band (1.5 vs. 0.7 months; p = 0.073).
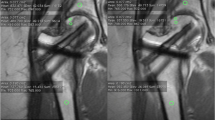
Based on the intensity of the subchondral bone on fat-suppressed T2-weighted images, the hips were classified into three types: type 1 showed high intensity, type 2 showed heterogeneous intensity, and type 3 showed low intensity. Twenty-one hips were classified as type 1, eight as type 2, and 11 as type 3 (Figs. 2, 3, and 4). The intra- and inter-observer agreements for type were 0.90 and 0.83, respectively, indicating almost perfect agreements.
Type 1 subchondral insufficiency fracture (SIF) of the femoral head in a 58-year-old female. The low intensity band (arrows) is seen on the T1-weighted image (a). The band is also seen on the fat-suppressed T2-weighted image (b). The subchondral bone (the area superior to the low intensity band on T1-weighted images: arrowheads) shows high intensity on the fat-suppressed T2-weighted image
Type 2 SIF of the femoral head in a 59-year-old male. The low intensity band (arrows) is seen on the T1-weighted image (a). The band is also seen on the fat-suppressed T2-weighted image (b). The subchondral bone (arrowheads) shows heterogeneous intensity on the fat-suppressed T2-weighted image. Histopathological findings of the subchondral bone (c: hematoxylin eosin ×40). Fracture callus formation (arrows) with associated granulation tissue (arrowheads) is observed in the area superior to the fracture line
Type 3 SIF of the femoral head in a 22-year-old male. The low intensity band (arrows) is seen on the T1-weighted image (a). The band is also seen on the fat-suppressed T2-weighted image (b). The subchondral bone (arrowheads) shows low intensity on the fat-suppressed T2-weighted image. Histopathological findings of the subchondral bone (c: hematoxylin eosin ×40). Fracture callus formation (arrows) is observed just beneath the fracture line. However, the area superior to the fracture line is almost detached from the femoral head, resulting in secondary osteonecrosis (empty lacunae: arrowheads). No evidence of antecedent bone infarction was confirmed
Correlation of subchondral bone intensity with histopathological findings
Six hips were evaluated histopathologically. Two of these were type 2 and four were type 3. All six hips showed fracture callus formation with associated granulation tissue just beneath the fracture line. No evidence of antecedent bone infarction was found in any hip.
In type 2 cases, fracture callus formation with associated granulation tissue was also observed in the area superior to the fracture line (Fig. 3). This viable bone and marrow tissue corresponded to an area of heterogeneous intensity on fat-suppressed T2-weighted images. In type 3 cases, in contrast, the area superior to the fracture line was almost detached from the femoral head, resulting in secondary osteonecrosis (Fig. 4). This area presented as low intensity on fat-suppressed T2-weighted images.
Correlation of subchondral bone intensity with clinicoradiological factors and clinical outcome
The clinicoradiological factors for each type are summarized in Table 2. The mean period between the onset of hip pain and MRI examination was significantly longer for type 2 than for type 1 (2.0 vs. 1.1 months; p = 0.017). Among hips that underwent MRI examination within 1 month after pain onset, 68 % were type 1, 7 % were type 2, and 25 % were type 3 (Fig. 5). Among hips that underwent MRI examination 2–3 months after pain onset, in contrast, 20 % were type 1, 50 % were type 2, and 30 % were type 3.
The percentage of hips with severe collapse at the time of diagnosis was significantly higher in the type 3 group than that in the type 1 group. The mean band length ratio in type 2 hips tended to be larger than in type 1 hips, although the difference did not reach statistical significance (49.6 % vs. 38.4 %; p = 0.088). There were no significant differences among the three types in regard to patient age, sex, or body mass index.
The clinical outcomes for each hip type are shown in Table 3. The resolution rate was 86 % for type 1 hips, 75 % for type 2, and 18 % for type 3, suggesting that the type 3 hips tended to resolve less often with conservative treatment than type 1 and type 2 hips.
Discussion
The subchondral portion of the femoral head showed varying intensity on fat-suppressed T2-weighted images, including high intensity, heterogeneous intensity, and low intensity. Although only six hips were available for histopathological assessment, we correlated subchondral intensity with histopathological findings in these cases. Based on these results, we speculate that the natural course of SIF of the femoral head can be broadly divided into two patterns: a normal fracture-healing pattern and an impaired fracture-healing pattern.
In the early phase of the normal fracture-healing pattern, associated bone marrow edema is generally observed not only distally but also in the proximal portion of the fracture line (type 1), indicating that bone and marrow tissue around the fracture line is viable [7, 12, 16–19]. The bone marrow edema gradually decreases over time, resulting in a heterogeneous intensity on the images (type 1 → type 2). We propose two possible explanations for the lower healing rate of type 2 hips compared with type 1. First, the band length ratio was relatively larger in type 2 hips, which might influence the clinical outcome. Second, some of the type 2 hips might be in a phase of delayed union, although most hips would be undergoing the normal fracture-healing process. In the impaired fracture-healing pattern, in contrast, almost all of the bone and marrow tissue in the proximal portion of the fracture line detached, leading to loss of blood supply and/or collapse. In these hips, the bone and marrow tissues in the proximal portion of the fracture line underwent secondary osteonecrosis histopathologically, which corresponded to the subchondral low intensity area on fat-suppressed T2-weighted images (type 3). In this study, four of 16 hips that underwent MRI examination within 1 month after pain onset were classified as type 3, suggesting that impaired fracture healing occurs even in the relatively early phase.
Previous studies have evaluated the factors affecting the clinical outcomes in SIF of the femoral head. Iwasaki et al. [6] demonstrated that lesion size and acetabular coverage were associated with outcome. Other reports noted that conservative treatment tended to be unsuccessful in older and female patients with SIF [20, 21]. In the present study, we identified the intensity of the subchondral portion of the femoral head as another possible predictor of the clinical outcome following conservative treatment. Type 1 hips tended to heal with conservative treatment (86 %), as did type 2 (75 %). In contrast, only 18 % of type 3 hips healed with conservative treatment. Therefore, it should be recognized that type 1 and type 2 hips are expected to resolve with conservative treatment, while type 3 hips seem to be difficult to resolve with conservative treatment alone.
It is important to make a differentiation between SIF and AVN, as both conditions often show similar radiographic findings. The pathogenesis of these two conditions is quite different, being fracture itself in SIF and bone infarction in AVN. Histopathologically, AVN is characterized by zone formation, comprising the necrotic bone trabeculae zone, the zone of creeping bone substitution, and the living zone [22, 23]. In contrast, SIF is characterized by an irregularly arranged fracture callus and granulation tissue around the fracture line [7, 8, 24, 25]. Zone formation is never seen in SIF, even if a small area of necrotic bone trabeculae confined to the area around the fracture line (secondary necrosis) is observed [8, 23, 25]. Previous studies demonstrated that SIF can be differentiated from AVN according to the shape of the low intensity band on T1-weighted images [2, 7, 11]. In SIF, the shape of the band is irregular, convex to the articular surface, and often discontinuous, representing the fracture line with associated repair tissue [2, 3, 7, 8, 11, 24, 25]. Conversely, in AVN, the shape of the band is well circumscribed, smooth, concave, and a mirror image of the articular surface, representing a reactive interface between live and necrotic bone [7, 8, 22, 23, 26]. In equivocal cases, gadolinium-enhanced MRI is reportedly useful for differentiating SIF from AVN [12].
Although the number of SIF patients in this study was larger than in previous reports, this study has several limitations. First, we investigated the MR images at one time point in each patient within 3 months after the onset of pain in a cross-sectional manner. MR images of SIF can potentially change during the first 3-month period. Therefore, we examined the proportion of total cases in each type classification at three different examination periods (in the first vs. the second vs. the third month after the onset of pain); interestingly, time-dependent change in the proportion of type 3 was not apparent, while the proportion of type 1 decreased with time and that of type 2 increased with time (Fig. 5). Sequential MRI studies are needed to confirm the time-dependent changes. Second, the mean follow-up period was relatively short, as we could not follow up all of the patients whose hips had become asymptomatic. Third, there was no control on the other variables that may influence fracture healing, such as bone mineral density and amount of weight-bearing. Prospective studies that carefully control these potential influencing factors and have longitudinal follow-up are needed to confirm the significance of the intensity of subchondral bone for the clinical outcome. Fourth, we did not evaluate the histopathological findings in the majority of cases, as specimens could not be obtained from the hips treated conservatively. Despite these limitations, however, we believe that the results of this study provide important information to those considering clinical management of SIF patients.
In conclusion, SIF can be classified into three types based on the intensity of the subchondral bone on fat-suppressed T2-weighted images. This variation may derive from the different conditions of the area proximal to the fracture line.
References
Bangil M, Soubrier M, Dubost JJ, et al. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed. 1996;63:859–61.
Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol. 1997;168:159–63.
Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42:2719–23.
Hagino H, Okano T, Teshima R, Nishi T, Yamamoto K. Insufficiency fracture of the femoral head in patients with severe osteoporosis: report of 2 cases. Acta Orthop Scand. 1999;70:87–9.
Legroux Gerot I, Demondion X, Louville AB, Delcambre B, Cortet B. Subchondral fractures of the femoral head: a review of seven cases. Joint Bone Spine. 2004;71:131–5.
Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fracture of the femoral head. AJR Am J Roentgenol. 2013;201:W97–103.
Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skelet Radiol. 2001;30:247–54.
Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol. 2000;24:464–8.
Davis M, Cassar-Pullicino VN, Darby AJ. Subchondral insufficiency fractures of the femoral head. Eur Radiol. 2004;14:201–7.
Slocum KA, Gorman JD, Puckett ML, Jones SB. Resolution of abnormal MR signal intensity in patients with stress fractures of the femoral neck. AJR Am J Roentgenol. 1997;168:1295–9.
Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y. MRI evaluation of collapsed femoral heads in patients 60 years old or older: differentiation of subchondral insufficiency fracture from osteonecrosis of the femoral head. AJR Am J Roentgenol. 2010;195:W63–8.
Miyanishi K, Hara T, Kaminomachi S, Maeda H, Watanabe H, Torisu T. Contrast-enhanced MR imaging of subchondral insufficiency fracture of the femoral head: a preliminary comparison with that of osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2009;129:583–9.
Chung CY, Park MS, Lee KM, et al. Hip osteoarthritis and risk factors in elderly Korean population. Osteoarthr Cart. 2010;18:312–6.
Mitchell DG, Rao V, Dalinka M, et al. MRI of joint fluid in the normal and ischemic hip. AJR Am J Roentgenol. 1986;146:1215–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Frihagen F, Nordsletten L, Tariq R, Madsen JE. MRI diagnosis of occult hip fractures. Acta Orthop. 2005;76:524–30.
Bogost GA, Lizerbram EK, Crues III JV. MR imaging in evaluation of suspected hip fracture: frequency of unsuspected bone and soft-tissue injury. Radiology. 1995;197:263–7.
Lee K, Yao L. Stress fractures: MR imaging. Radiology. 1988;169:217–20.
Deutsche AL, Mink JH, Waxman AD. Occult fractures of the proximal femur: MR imaging. Radiology. 1989;170:113–6.
Miyanishi K, Ishihara K, Jingushi S, Torisu T. Risk factors leading to total hip arthroplasty in patients with subchondral insufficiency fracture of the femoral head. J Orthop Surg (Hong Kong). 2010;18:271–5.
Yamamoto T, Karasuyama K, Iwasaki K, Doi T, Iwamoto Y. Subchondral insufficiency fracture of the femoral head in males. Arch Orthop Trauma Surg. 2014;134:1199–203.
Bullough PG, DiCarlo EF. Subchondral avascular necrosis: a common cause of arthritis. Ann Rheum Dis. 1990;49:412–20.
Yamamoto T, DiCarlo EF, Bullough PG. The prevalence and clinicopathological appearance of extension of osteonecrosis in the femoral head. J Bone Joint Surg (Br). 1999;81:328–32.
Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum. 2005;52:1293–6.
Yamamoto T, Iwamoto Y, Schneider R, Bullough PG. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis. 2008;67:150–3.
Kubo T, Yamazoe S, Sugano N, et al. Initial MRI findings of non-traumatic osteonecrosis of the femoral head in renal allograft recipients. Magn Reson Imaging. 1997;15:1017–23.
Acknowledgments
This work was supported by a research grant from the Japan Society for the Promotion of Science (15 K10479) and a Research Grant for Intractable Diseases from the Japan Agency for Medical Research and Development (H26-Itaku(Nan)-Ippan-031).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sonoda, K., Yamamoto, T., Motomura, G. et al. Fat-suppressed T2-weighted MRI appearance of subchondral insufficiency fracture of the femoral head. Skeletal Radiol 45, 1515–1521 (2016). https://doi.org/10.1007/s00256-016-2462-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2462-z