Abstract
Purpose
To verify the hypothesis that depth of the low-intensity band on T1-weighted MR image is useful for distinguishing subchondral insufficiency fracture (SIF) from osteonecrosis of the collapsed femoral head (ON).
Patients and methods
We reviewed 35 consecutive hips in 35 patients with radiological evidence of subchondral collapse of the femoral head and available MR images and histology between May 2013 and January 2016. Both clinical and radiological appearances were investigated. The ratios of distance from articular surface of the femoral head to the T1 low-intensity band to femoral head diameter (band depth ratio: BDR) on (1) mid-coronal slice of MR images and that on (2) coronal slice of MR images in which the highest BDR was observed, were calculated.
Results
The mean age in SIF group was significantly higher than that in ON group (SIF: 68 years, ON: 49 years, P = 0.0017). The rates of history of steroid intake or alcohol consumption in SIF group were significantly lower than those in ON group (P = 0.0022 and P = 0.0408, respectively). The mean BDRs in SIF group were (1) 0.16 and (2) 0.23, which were significantly lower than those in ON group [(1) 0.42 and (2) 0.59] (P < 0.0001 for both). The cut-off BDR values to differentiate SIF from ON were (1) 0.22 and (2) 0.38, respectively.
Conclusion
The results of the study suggest that depth of the low-intensity band on T1-weighted MR image is useful for distinguishing SIF from ON in cases with collapsed femoral heads.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Subchondral insufficiency fracture of the femoral head (SIF) is one of the important diseases reflecting an aged society, since a SIF has so far been mainly reported in elderly women with osteoporosis [1,2,3]. It is necessary to differentiate SIF from osteonecrosis of the femoral head (ON), as these two conditions have several overlapping characteristics in both imaging and clinical appearances [1, 2].
A number of studies have reported useful clinical and imaging features for distinguishing SIF from ON, since some cases of SIF have been reported to heal after conservative therapy [4]. One of the characteristic findings in SIF has been reported to be the shape of the low-intensity band on the T1-weighted image: it is generally irregular, serpiginous, convex to the articular surface, and often discontinuous [1,2,3]. Conversely, in ON, it is generally smooth and circumscribes all of the necrotic segments, as the low-intensity band represents repaired tissue [1, 2]. However, a recent paper reported a SIF case with concave-shaped low-intensity band, such as in ON [5].
The aim of this study was to test the hypothesis that SIF can be differentiated from ON according to the depth of the low-intensity band on T1-weighted MR image in cases with collapsed femoral heads.
Patients and methods
The institutional review board (IRB) approved the study. This study reviewed 35 consecutive hips in 35 patients with radiological evidence of a subchondral collapse of the femoral head, where both MRI and histology were available, between May 2013 and January 2016. The patients included 15 males and 20 females with a mean age of 59 years (range 25–86 years). All hips underwent prosthetic replacement. Regarding the clinical factors, the history of corticosteroid intake or alcohol abuse was investigated. Alcohol abuse was defined as the consumption of more than 400 ml of ethanol per week, which is known to result in a significant risk for ON [6]. The body mass index (BMI; kg/m2) was calculated and obesity was defined as a BMI of 26.4 or greater [7].
Histopathological diagnoses
The histopathological diagnosis of SIF was made according to the following reported characteristics [1, 2]: macroscopically, a liner fracture with a whitish-gray appearance paralleling the subchondral bone endplate was observed: microscopically, the whitish-gray area consisted of irregularly arranged fracture callus, reactive cartilage, and granulation tissue. It should be noted that small areas of necrotic bone trabeculae and bone marrow may be observed in SIF; however, such necrosis is confined to the area around the fracture line without any evidence of antecedent bone infarction [8, 9]. The histopathological diagnosis of ON was made when the femoral head showed a zonal pattern comprising an area of bone infarction, reparative granulation tissue, and viable tissue [10].
Radiological evaluations
Radiographically, the presence of demarcating sclerosis, a subchondral fracture, and the degree of collapse of the femoral head were investigated on both the anteroposterior (AP) and lateral views [11, 12].
MRI evaluations
The MR examinations were performed by using a 1.5-T system (Siemens; Erlangen, Germany) under 5 mm slice thickness. The matrix sizes were 192–256 × 256–512 for both coronal and axial images. The fields of view were 330–350 mm for coronal images and 300–330 mm for axial images. The T1-weighted spin-echo (SE) images (repetition time/echo time [TR/TE] = 430–616/10–14 ms), fat-saturated T2-weighted SE images (TR/TE = 3500–5000/82–90) in the coronal and axial (and/or oblique-axial: paralleling the femoral neck axis) planes were available in all 35 cases.
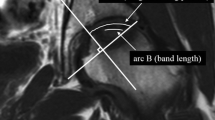
The band depths were calculated as the band depth ratios (BDRs) using the NIH Image freeware (Bethesda, MD, USA) (Fig. 1). The BDRs were calculated using following formula: (distance from the articular surface of the femoral head to the T1 low-intensity band)/femoral head diameter on the (1) mid-coronal slice of MR images and that on the (2) coronal slice of MR images in which the deepest low-intensity band (the highest BDR) was observed. When two low-intensity bands were observed in a femoral head, the BDRs were calculated using the distal band [13]. In addition, the location (center, anterior or posterior) of the highest BDR was investigated. The calculations were made by two observers (S.I. and G.M.), who are orthopedic surgeons and have extensive experience with making imaging diagnoses. To evaluate the inter-observer reproducibility of the measurements of the BDRs and the locations of the highest BDRs, the reliability of the measurements was evaluated using Spearman’s correlation coefficient and kappa statistics, respectively. The correlations between the measurements were considered to be in good agreement (> 0.7) [14]. A kappa value of 0.21–0.4 corresponds to a fair agreement. A value of 0.41–0.6 represents moderate agreement, and values of 0.61–0.8 indicate substantial agreement. A value of > 0.81 is considered to be almost perfect [15].
Diagram showing the method used to calculate the ratios of the band depth ratio of the femoral head using the NIH Image freeware (Bethesda, MD, USA). The left panel is a mid-coronal slice of the T1-weighted MR image. a is the diameter of the femoral head and b is the longest distance from the articular surface to the low-intensity band. Then, the lengths of a and b were automatically calculated, where b/a is the band depth ratio (BDR) on the mid-coronal slice of the T1-weighted MR image. The right panel is a coronal slice (anterior slice in this case) of MR images in which the highest BDR is observed. b′/a′ indicate the highest BDR of all coronal slices
Statistical analyses were carried out using the Chi square test or Fisher’s exact probability to compare sex, history of steroid intake or alcohol consumption, presence of radiological demarcating sclerosis or subchondral fracture and location of the highest BDR between the two groups. The age, BMI, bone mineral density (T score), degree of femoral head collapse, and BDRs were compared between the SIF and ON groups using the unpaired t test. The cut-off BDR values to differentiate SIF from ON were calculated using receiver operating characteristic (ROC) curves. In the ROC curves, the area under the curve (AUC) was used to test the useful BDRs, in which an area of 1 represented a perfect test and an area of 0.5 represented a worthless test. The statistical analyses were performed using the JMP Ver. 9.0.1 software program (SAS Institute Inc., Cary, NC). p values of less than 0.05 were considered to be statistically significant.
Results
According to the histopathological findings, 18 patients (18 hips) were diagnosed as having SIF (Fig. 2) and 17 patients (17 hips) as having ON (Fig. 3). The detailed clinical findings of all patients are shown in Table 1. The patients in the SIF group included 5 males and 13 females with a mean age of 68 years (range 41–85 years) and ten males and seven females with a mean age of 49 years (range 25–86 years) in the ON group. There was a significant difference in the age between the two groups (P = 0.0017). The proportion of females was higher in the SIF group than that in the ON group. However, there was no significant difference in the sex between the two groups (P = 0.0636). All of the patients with ON had a history of corticosteroid intake or alcohol abuse, or both. On the other hand, only 4 of 18 patients (22%) with SIF had a history of corticosteroid intake, and one patient (6%) had a history of alcohol abuse. The rates of history of steroid intake or alcohol consumption in the SIF group were significantly lower than those in the ON group (P = 0.0022 and P = 0.0408, respectively).
An 81-year-old female with a history of corticosteroid intake (SIF). Her body mass index (BMI) was 21.1 kg/m2. a An anteroposterior (AP) radiograph of the right hip at the onset of pain. A collapse is not observed at the femoral head. b An AP radiograph 3 months after the onset of pain. Both a collapse of the femoral head and osteoarthritic change (joint-space narrowing) are observed at the superolateral portion of the femoral head, although she underwent the conservative treatment (the avoidance of weight bearing activities for 4 weeks). c The low-intensity band on the mid-coronal slice of the T1-weighted MR image (repetition time/echo time [TR/TE] = 616/10 ms) is parallel to the subchondral bone end-plate. The BDR was 0.10. d The highest BDR (0.17) of all coronal slices is observed at the posterior portion on the femoral head. e The band region histopathologically corresponds to the fracture callus, reactive cartilage, and granulation tissue (H&E, ×40)
A 38-year-old male with a history of corticosteroid intake (ON). a An AP radiograph of the left hip just before prosthetic replacement (Stage 3A and Type C2). b The low-intensity band on the mid-coronal slice of the T1-weighted MR image (TR/TE = 430/14) is concave to the articular surface. The BDR is 0.58. c The highest BDR (0.71) is observed at the anterior portion on the femoral head. d The histopathological appearance of the necrotic region, which demonstrates the accumulation of bone marrow cell debris, and bone trabeculae with empty lacunae beneath the fracture line (H&E, ×40). e There is repair tissue in the reparative zone, including vascular granulation tissue and fibrous tissue (H&E, ×40)
Radiologically, in ON, nine hips were classified as stage 3A, which indicates the collapse of the femoral head to be less than 3 mm, five hips were classified as stage 3B (3 mm or more), and three were classified as stage 4 (osteoarthritic changes) according to the classification of the Japanese Investigation Committee of Health and Welfare [16]. Localization of the affected necrotic lesion was type C1 (the necrotic area occupies more than two-thirds of the region but does not extend to the acetabular edge) in 6 hips and type C2 (the necrotic area occupies more than two-thirds of the region and extends to the acetabular edge) in 11 [16]. Demarcating sclerosis in the femoral head was observed radiographically in 9 of 18 hips (50.0%) in SIF group and in 11 of 17 hips (64.7%) in ON group. A subchondral fracture was seen in 11 of 18 hips (61.1%) in SIF group and in 9 of 17 hips (52.9%) in ON group. There were no significant differences in the rates of either demarcating sclerosis or subchondral fracture between SIF and ON groups (P = 0.3784 and P = 0.6253, respectively). Among positive radiological subchondral fracture cases (SIF: 11, ON: 9), all 11 cases with SIF showed the T1 low-intensity band on MR images at the subchondral portion of the femoral head, while only two cases with ON (22.2%) showed this findings, a significant difference between the groups (P = 0.0005). A previous report showed the proximal band at the subchondral portion in case with ON corresponded to the fracture line with aggregation of bone debris, while the distal band corresponded to the reparative tissue formed around the osteonecrosis [13]. The mean degree of collapse of the femoral head was 2.1 mm (range 1–4 mm) in SIF group and 2.5 mm (range 1–5 mm) in ON group. There was no significant difference in the degree of collapse of the femoral head between SIF and ON groups (P = 0.3122).
The results of MRI evaluations are also shown in Table 1. The mean BDR on the (1) mid-coronal slice of MR images in the SIF group was 0.16, while that in the ON group was 0.42. There was a significant difference in the BDR on the mid-coronal slice of MR images between the two groups (P < 0.0001). In the SIF group, the mean BDR on the (2) coronal slice of MR images in which the highest BDR was observed, was 0.23, while that in the ON group was 0.59. There was a significant difference in the highest BDR of all coronal MR images between the two groups (P < 0.0001). The mean difference between (1) the highest BDR of all coronal slices and (2) the BDR on the mid-coronal slice in the ON group was significantly larger than that in the SIF group (P = 0.0084). The cut-off BDR values to differentiate SIF from ON were (1) 0.22 (sensitivity: 94%, specificity: 94%) and (2) 0.38 (sensitivity: 100%, specificity: 94%), respectively (Fig. 4). Regarding the locations of the deepest low-intensity band (the highest BDR), in the SIF group, 7 of 18 cases (39%) were seen in the mid-coronal slice (center), 7 (39%) in the anterior portion and 4 (22%) in the posterior portion. In contrast, in the ON group, 4 of 17 cases (24%) were seen in the mid-coronal slice (center), 12 (71%) in the anterior portion and 1 (5%) in the posterior portion. A higher proportion of cases in the ON group demonstrated the highest BDR in the anterior portion than that in the SIF group; however, there was no significant difference between the two groups (P = 0.1314).
Receiver operating characteristic (ROC) curve analysis of band depth ratio (BDR) on the mid-coronal slice (a) and the highest BDR of all coronal slices (b) for diagnosis of SIF compared to ON shown by ROC curves. Schematic diagrams of MRI (right femoral head) created according to the cut-off values to differentiate SIF from ON are shown in the graphs. a The area under the curve (AUC) values was 0.9853 in the BDR on the mid-coronal slice. The cut-off BDR value on the mid-coronal slice to differentiate SIF from ON is 0.22 (sensitivity: 94%, specificity: 94%). b The AUC value was 0.9935 in the highest BDR of all coronal slices. The cut-off BDR value of all coronal slices to differentiate SIF form ON is 0.38 (sensitivity: 100%, specificity: 94%)
The inter-observer reproducibility of the BDR calculations on the mid-coronal section was 0.831 and those of the highest BDR calculations on all coronal slices was 0.781, which were in good agreement. The inter-observer reproducibility of the definition of location (center, anterior or posterior) of the highest BDR was 0.903 (almost perfect).
Discussion
The findings of this study indicated that the depth of the low-intensity band on the T1-weighted image is a useful imaging tool for the differentiation of SIF from ON according to the histopathological diagnoses of cases with SIF or ON. Radiologically, there were no significant differences in the frequency of the demarcating sclerosis or subchondral fracture between the SIF and ON groups, indicating that these findings are not sufficient to distinguish between the two conditions. We, therefore, recommend assessing not only the shape of the low-intensity band on T1-weighted imaging but also the depth of the low-intensity band when examining patients with radiological collapse of the femoral head [1,2,3,4, 11, 14].
Several reports have focused on useful clinical features for the differentiation of SIF from ON [1, 2]. The authors concluded that osteoporotic elderly women without any history of corticosteroid intake or alcohol abuse may have a high likelihood of suffering from SIF rather than ON when radiographs show a collapse of the femoral head [2], which were consistent with the majority of our cases (Table 1).
In the current study, both the mean BDR on the mid-coronal slice and the mean highest BDR (the deepest low-intensity band of the femoral head) of all coronal slices in the SIF group were significantly lower than those in the ON group (P < 0.0001 for both). Although there have been no reports focused on the depth of the low-intensity band on the T1-weighted images for differentiation of SIF from ON, the results of our study are considered to be reasonable because of the following factors: in SIF, the low-intensity band corresponds to a subchondral fracture. Therefore, it is generally observed at the shallow portion of the femoral head. In contrast, in ON, the low-intensity band represents a reactive interface between live and necrotic bone. Therefore, the low-intensity band can be observed at the deep portion of the femoral head.
All cases are well supported by histopathological evidence, which is a strength of the paper. However, this may also represent a major limitation, as the results of our study are specific to patients who have undergone prosthetic replacement. Another major limitation is the small number of cases examined (SIF: 18 cases, ON: 17 cases). Further studies with a large number of cases with or without subchondral collapse in order to evaluate the correlation between the depth of the T1 low-intensity band on MR images and the histopathological findings are, therefore, necessary. The final limitation is that a radiologist was not included in this study.
In conclusion, the depth of the low-intensity band (BDR) on the coronal slice of T1-weighted MR images is useful for distinguishing SIF from ON in cases with collapsed femoral heads.
References
Yamamoto T, Iwamoto Y, Schneider R, Bullough PG (2008) Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis 67:150–153
Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y (2013) The utility of clinical features for distinguishing subchondral insufficiency fracture from osteonecrosis of the femoral head. Arch Orthop Trauma Surg 133:1623–1627
Kim SM, Oh SM, Cho CH et al (2016) Fate of subchondral fatigue fractures of femoral head in young adults differs from general outcome of fracture healing. Injury 47:2789–2794
Vande Berg BC, Malghem J, Lecouvet FE, Jamart J, Maldague BE (1999) Idiopathic bone marrow edema lesions of the femoral head: predictive value of MR imaging findings. Radiology 212:527–535
Zhao G, Yamamoto T, Ikemura S et al (2010) A histopathological evaluation of a concave-shaped low-intensity band on T1-weighted MR images in a subchondral insufficiency fracture of the femoral head. Skeletal Radiol 39:185–188
Matsuo K, Hirohata T, Sugioka Y, Ikeda M, Fukuda A (1988) Influence of alcohol intake, cigarette smoking, and occupational status on idiopathic osteonecrosis of the femoral head. Clin Orthop 234:115–123
Yoshiike N, Matsumura Y, Zaman MM, Yamaguchi M (1998) Descriptive epidemiology of body mass index in Japanese adults in a representative sample from the National Nutrition Survey 1990–1994. Int J Obes Relat Metab Disord 22:684–687
Bullough PG, DiCarlo EF (1990) Subchondral avascular necrosis: a common cause of arthritis. Ann Rheum Dis 49:412–420
Todd RC, Freeman MAR, Pirie CJ (1972) Isolated trabecular fatigue fractures in the femoral head. J Bone Joint Surg Br 54:723–728
Yamamoto T, DiCarlo EF, Bullough PG (1999) The prevalence and clinicopathological appearance of extension of osteonecrosis in the femoral head. J Bone Joint Surg Br 81:328–332
Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y (2010) MRI evaluation of collapsed femoral head in patients 60 years old or older: differentiation of subchondral insufficiency fracture from osteonecrosis of the femoral head. AJR Am J Roentgenol 195:W63–W68
Kubo Y, Motomura G, Ikemura S, Sonoda K, Yamamoto T, Nakashima Y (2017) Factors influencing progressive collapse of the transposed necrotic lesion after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. Orthop Traumatol Surg Res 103:217–222
Yamaguchi R, Yamamoto T, Motomura G, Ikemura S, Iwamoto Y (2011) MRI-detected double low-intensity bands in osteonecrosis of the femoral head. J Orthop Sci 16:471–475
Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y (2013) Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fracture of the femoral head. AJR 201:W97–W103
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K (2002) The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci 7:601–605
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ikemura, S., Mawatari, T., Matsui, G. et al. The depth of the low-intensity band on the T1-weighted MR image is useful for distinguishing subchondral insufficiency fracture from osteonecrosis of the collapsed femoral head. Arch Orthop Trauma Surg 138, 1053–1058 (2018). https://doi.org/10.1007/s00402-018-2948-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2948-3