Abstract
We report a histologically proven case of synovial haemangioma of the knee in a 14-month old girl who presented to the emergency department with an acute 1-day history of refusing to weight-bear on the right leg and a preceding 3-week history of a right knee lump. Physical examination revealed a non-tender, soft lump over the lateral infrapatellar region. Radiographs revealed a poorly defined soft tissue density over the infrapatellar fat pad and a suprapatellar joint effusion. Ultrasound was used to confirm the presence of a vascular soft tissue mass compatible with a synovial haemangioma within the infrapatellar fat pad which showed both intra-articular and extra-articular extension. There was good correlation of the ultrasound findings with magnetic resonance imaging (MRI), highlighting the potential clinical utility of ultrasound as an alternative imaging modality in establishing the pre-operative diagnosis and extent of a synovial haemangioma about the knee joint.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Synovial hemangiomas, first described by Bouchut in 1856, are rare benign vascular lesions which occur most frequently about the knee joint, but have also been reported in the elbow, wrist, ankle, synovial tendon sheaths and temporo-mandibular joint [1–7]. The average age of onset is in adolescence, with Moon reporting an average age of onset of 10.9 years in girls and 12.5 years in boys, and approximately 75 % of cases become symptomatic prior to the age of 16 years [8]. The presenting symptoms are often non-specific, which often leads to a delay in diagnosis of many years and can result in arthropathy if left undetected [9–13]. We describe the clinical presentation and imaging findings of a histologically proven case in a 14-month old girl, which to our knowledge is the youngest case of a synovial haemangioma to be reported in the literature, and discuss the relevant differential diagnoses. The importance of how multimodality imaging in particular ultrasound may be used to establish the pre-operative diagnosis of a synovial haemangioma and aid in surgical planning is also emphasized.
Case report
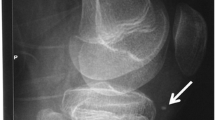
A 14-month old girl presented to the emergency department with an acute 1-day history of refusing to weight-bear on the right leg and a preceding 3-week history of a right knee lump. There was no antecedent trauma to the affected knee. Physical examination revealed a non-tender, soft lump measuring approximately 1.0 cm in diameter over the lateral infrapatellar region. Radiographs revealed a poorly defined soft tissue density over the infrapatellar fat pad, but no phlebolith or underlying bony erosion was evident (Fig. 1). There was also suggestion of a suprapatellar joint effusion on the radiographs (Fig. 1), which was subsequently proven to be a haemarthrosis by aspiration.
Further imaging with ultrasound showed a circumscribed soft tissue mass lying deep to the patellar tendon as well as lateral patellar retinaculum, which was slightly hyperechoic to the overlying subcutaneous fat and demonstrated thin echogenic internal septations with intralesional vascular channels demonstrating arterial flow (Fig. 2). There was no central nidus of tangled vessels, nor were there enlarged feeding or draining vessels to suggest the presence of an arteriovenous malformation. There was a small focal protrusion of the mass through the lateral patellar retinaculum into the subcutaneous fat (Fig. 2), which corresponded to the clinically palpable component of the mass. Intra-articular extension of the mass into the anterior aspect of the intercondylar notch was also demonstrated (Fig. 2).
Ultrasound reveals a a circumscribed soft tissue mass (white asterisk) lying deep to the patellar tendon as well as the lateral patellar retinaculum within the infrapatellar fat pad, which is slightly hyperechoic to the overlying subcutaneous fat and demonstrates thin echogenic internal septations. b A small focal protrusion of the mass (white asterisk) through the lateral patellar retinaculum (white arrow) into the subcutaneous fat is also noted, corresponding to the clinically palpable lump. c Intra-articular extension of the mass (white asterisk) to the anterior aspect of the intercondylar notch is noted (dashed white arrow; P patella, F distal femur; T proximal tibia). d Arterial flow is detected within vascular channels seen coursing within the lesion with Doppler interrogation
MRI demonstrated a soft tissue mass with lobulated margins within the infrapatellar fat pad which extended intra-articularly into the anterior aspect of the intercondylar notch. MRI also confirmed the ultrasound finding of a small focal protrusion of the infrapatellar mass through the lateral patellar retinaculum into the overlying subcutaneous fat. The mass was isointense to skeletal muscle on T1-weighted spin-echo images, heterogeneously hyperintense on T2-weighted fat-saturated fast spin-echo images and demonstrated avid heterogeneous enhancement on multiplanar post-gadolinium T1-weighted fat-saturated spin echo sequences. Thin internal septations and intra-lesional fluid-fluid levels were visualized (Fig. 3). Blooming susceptibility artifacts on gradient-echo recalled images in the infero-lateral aspect of the mass were suggestive of haemosiderin deposition from previous haemorrhage. Coronal time resolved imaging of contrast kinetics (TRICKS) magnetic resonance angiography (MRA) images demonstrated arterial supply of the mass from the popliteal artery, as well as a few small caliber vascular channels at the site of the mass in the delayed phase (Fig. 3)
Axial MRI images of the knee showing an infrapatellar mass with focal protrusion into the subcutaneous fat that is a isointense to skeletal muscle on T1-weighted spin echo images (white asterisk), and b heterogeneously hyperintense on T2-weighted fat saturated fast spin echo images with thin hypointense internal septations (white arrows). c Sagittal post contrast T1-weighted fat saturated images demonstrates avid heterogeneous enhancement and extension into the anterior aspect of the intercondylar notch (white arrow). d Coronal gradient-echo recalled images in the infero-lateral aspect of the mass (dashed white arrow) showed blooming susceptibility artefacts which were suggestive of haemosiderin deposition from previous haemorrhage. Coronal TRICKS MRA of the knee demonstrates e a non-enlarged feeding vessel (white arrow) arising from the popliteal artery in the early arterial phase, and f a cluster of small calibre vascular channels (short dashed white arrows) at the expected location of the infrapatellar mass in the delayed phase
The presumptive pre-operative diagnosis of a synovial haemangioma was made from the ultrasound and MRI findings. The differential diagnostic considerations for our case included localized nodular synovitis and pigmented villonodular synovitis (PVNS). The patient subsequently underwent open arthrotomy via an anterolateral approach based on the pre-operative imaging findings, with surgical excision of first the extra-articular portion of the mass, followed by the deeper components of the mass within the infrapatellar fat pad and anterior aspect of the intercondylar notch. The excised gross specimen comprised of a soft, brownish mass which measured approximately 2.0 × 0.8 × 1.0 cm. Microscopic examination revealed predominant large, thin-walled, erythrocyte-containing vascular spaces lined by flattened endothelial cells within the subsynovial mesenchyme (Fig. 4). There was also evidence of synovial hyperplasia with deposits of haemosiderin in keeping with a haemosiderotic synovitis (not shown). A post-operative diagnosis of a synovial haemangioma (cavernous subtype) was made based on the histologic findings.
Discussion
Soft tissue haemangiomas can be classified histologically according to the nature and size of the vessels predominant within the lesion into cavernous (50 %), lobular capillary (25 %), arteriovenous (20 %) and venous (5 %) subtypes [14]. Another classification system is based on the anatomical relationship of the haemangioma to the joint: juxta-articular haemangiomas which are situated external to the joint capsule, intra-articular haemangiomas situated within the joint capsule, and an intermediate type of haemangioma with both intra- and extra-articular components [9]. The intra-articular and the intermediate types of haemangiomas arise from the synovium, and are termed synovial haemangiomas [6, 9].
The gross macroscopic appearance of a synovial haemangioma has been described as a lobulated, doughy mass that is frequently stained dark red or mahogany brown by hemosiderin. On microscopic examination, the lesion demonstrates arborizing vascular channels in the subsynovial mesenchyme, which may be associated with a hyperplastic overlying synovium and haemosiderin deposition in chronic cases with repeated haemarthrosis [6, 15]. These macroscopic and microscopic features characteristic for a synovial haemangioma were identified in our case, and were further classified by the nature and size of the vascular channels predominant within the lesion as a cavernous subtype.
The presenting symptoms are non-specific and include knee pain, limitation of joint motion, a haemarthrosis resulting from tumor haemorrhage which may be recurrent, or a painless mass [8–13]. This often contributes to a diagnostic delay of several years, especially in paediatric patients where clinical evaluation may be difficult [9–13]. In our reported case, the synovial haemangioma itself accounted for the clinical finding of a painless right knee lump, while the more acute presentation of refusing to weight bear on the affected limb was likely secondary to the haemarthrosis resulting from haemorrhage of the synovial haemangioma. Arthropathy of the knee joint arising from repeated episodes of haemarthrosis similar to what is seen in haemophilia has been described as a long-term sequela in reported cases of diagnostic delay, with the treatment of choice for these uncommon lesions being surgical excision as early as possible [10–13].
Radiographs are normal in over half of patients with synovial haemangiomas of the knee joint [16], but may demonstrate non-specific features such as a joint effusion, soft tissue mass about the joint (as in our case), osteoporosis, advanced maturation of the epiphysis and arthropathy simulating haemophilia [7–13]. Phleboliths are occasionally visualised when adjacent muscles or soft tissue structures are involved [17].
MRI plays a significant role in the diagnosis of soft tissue haemangiomas of the extremities [18]. The MRI signal characteristics of the soft tissue mass and associated features of intra-lesional septations, fluid-fluid levels and haemosiderin deposition in our case were compatible with the imaging findings described in previous reports of synovial haemangiomas of the knee joint [7, 9, 19–22]. MRI also confirmed the intra- and extra-articular nature of the mass in our case. TRICKS MRA allows for highly accurate definition of the anatomy and filling dynamics of the peripheral vasculature, which may be used to overcome the limitations of reduced temporal resolution with long multiphase acquisition times, or problems with synchronization between bolus arrival and image acquisition, which are encountered with traditional contrast-enhanced bolus-chase MRA techniques [23–25]. A non-enlarged feeding vessel arising from the popliteal artery was detected in the early arterial phase, along with a few small caliber vascular channels at the site of the mass in the delayed phase, but there was no associated central nidus of tangled vessels or enlarged draining vein, and this helped to exclude the presence of an arteriovenous malformation.
While the sonographic features of soft tissue haemangiomas of the extremities have been described previously [18, 26], to the authors’ knowledge, ultrasound evaluation specifically of synovial haemangiomas of the knee joint has not been widely described in the published literature, with only one prior case report known to the authors [27]. While MRI has been described as the imaging modality of choice for establishing the pre-operative diagnosis and planning for surgical excision of synovial haemangiomas [20, 22], the use of ultrasound in our case enabled us to establish a presumptive diagnosis of a synovial haemangioma within the infrapatellar fat pad in our patient, exclude the presence of an arteriovenous malformation, as well as accurately determine the true extra-articular and intra-articular extent of the lesion. This demonstrates the potential clinical utility of using ultrasound in establishing a pre-operative diagnosis of synovial haemangioma and also to guide the surgical approach, which may be important particularly in paediatric patients who in certain scenarios may be unable to co-operate fully and/or are not suited to undergo sedation for the purpose of performing an MRI.
The differential diagnostic considerations for the synovial lesion of the knee in our case included localized nodular synovitis and PVNS, both of which are benign proliferative disorders of the synovium. Localized nodular synovitis usually presents as a small, solitary intra-articular mass which most commonly involves the infrapatellar fat pad [28]. These lesions demonstrate intermediate or hyperintense signal intensity relative to skeletal muscle on T1-weighted images, variable heterogeneously high or low signal intensity on T2-weighted images, and prominent post-contrast enhancement. Haemosiderin deposition in localized nodular synovitis is highly variable and may even be absent [28, 29]. The most characteristic finding of PVNS on MRI is the signal loss on gradient-echo and T2-weighted images due to paramagnetic effects of haemosiderin, with ‘blooming’ artefacts more evident on the gradient-echo sequences [30]. PVNS may appear heterogeneous on T1-weighted images, with areas of high signal representing aggregates of lipid laden macrophages [31]. The margins of the lesion are usually well demarcated by a low signal intensity capsule secondary to haemosiderin deposition or fibrosis. Post contrast enhancement is usually marked in areas of the lesion not heavily laden with haemosiderin [30, 31].
In conclusion, synovial haemangioma of the knee joint is an uncommon vascular lesion which should be considered in the differential diagnosis of a child who presents with knee pain, possibly manifesting clinically as refusal to weight bear on a lower limb. While MRI has been described as the imaging modality of choice, our case highlights the potential clinical utility of ultrasound as an alternative imaging modality in establishing the pre-operative diagnosis and in planning for surgical excision of a synovial haemangioma about the knee joint.
References
Bouchut ME. Tumeur érectile de l’articulation du genou. Gaz Hop Paris. 1856;29:379.
Larsen IJ, Landry RM. Hemangioma of the synovial membrane. J Bone Joint Surg Am. 1969;51:1210–12.
Lewis RC, Coventry MB, Soule EH. Hemangioma of the synovial membrane. J Bone Joint Surg Am. 1959;41:264–71.
Uotila E, Westerholm N. Hemangioma of the temporomandibular joint. Odontol Tidskr. 1966;74:202–6.
Waddell GE. A haemangioma involving tendons. J Bone Joint Surg (Br). 1967;49:138–41.
Devaney K, Vinh TN, Sweet DE. Synovial haemangioma: a report of 20 cases with differential diagnostic considerations. Hum Pathol. 1993;24:737–45.
Greenspan A, Azouz EM, Matthews II J, Decarie J-C. Synovial haemangioma: imaging features in eight histologically proven cases, review of the literature, and differential diagnosis. Skeletal Radiol. 1995;24:583–90.
Moon NF. Synovial haemangioma of the knee joint. Clin Orthop. 1969;90:183–90.
Cotton A, Flipo RM, Herbaux B, Gougeon F, Lecomte-Houcke M, Chastanet P. Synovial haemangioma of the knee: a frequently misdiagnosed lesion. Skeletal Radiol. 1995;24:257–61.
Resnick D, Oliphant M. Hemophilia-like arthropathy of the knee associated with cutaneous and synovial hemangiomas. Radiology. 1975;114:323–26.
Tomoyuki A, Taisuke T, Kenichi T. Synovial haemangioma of the knee in young children. J Pediatr Orthop B. 2002;11:293–7.
Ramseier LE, Exner GU. Arthropathy of the knee joint caused by synovial haemangioma. J Pediatr Orthop. 2004;24:83–6.
Forrest J, Staple TW. Synovial hemangioma of the knee: demonstration by arthrography and arteriography. Am J Roentgenol. 1971;112:512–6.
Stout AP. Hemangio-endothelioma: a tumor of blood vessels. Ann Surg. 1943;118:445.
Bullough PG. Atlas of orthopaedic pathology with clinical and radiologic correlations, 2nd edn. New York: Gower Medical. 1992;15:14.
Moon NF. Synovial hemangioma of the knee joint: a review of previously reported cases and inclusion of two new cases. Clin Orthop. 1973;90:183–90.
Jaffe HL. Tumors and tumorous conditions of the bones and joints. Philadelphia: Lea & Febiger; 1958. p. 512–16.
Greenspan A, McGahan JP, Vogelsang P, Szabo RM. Imaging strategies in the evaluation of soft-tissue haemangiomas of the extremities: correlation of the findings of plain radiography, angiography, CT, MRI and ultrasonography in 12 histologically proven cases. Skeletal Radiol. 1992;21:11–8.
Llaugher J, Monill JM, Palmer J, Clotet M. Synovial haemangioma of the knee: MRI findings in two cases. Skeletal Radiol. 1995;24:579–81.
Clough TM, Hill JC. Synovial haemangioma - gadolinium enhanced MRI scanning is the investigation of choice for planned surgical excision. Knee. 1999;6:239–44.
Comert RB, Aydingoz U, Atay OA, Gedikoglu G, Doral MN. Vascular malformation in the infrapatellar (Hoffa’s) fat pad. Knee. 2004;11:137–40.
Sasho T, Nakagawa K, Matsuki K, Hoshi H, Masahiko S, Naoshi I, et al. Two cases of synovial haemangioma of the knee joint: Gd-enhanced image features on MRI and arthroscopic excision. Knee. 2011;18:509–11.
Swan JS, Carroll TJ, Kennell TW, Heisey DM, Korosec FR, Frayne R, et al. Time-resolved three-dimensional contrast enhanced MR angiography of the peripheral vessels. Radiology. 2002;225:43–52.
Thornton FJ, Du J, Suleiman SA, Dieter R, Tefera G, Pillai KR, et al. High-resolution, time-resolved MRA provides superior definition of lower-extremity arterial segments compared to 2D time-of-flight imaging. J Magn Reson Imaging. 2006;24:362–70.
Blackham KA, Passalacqua MA, Sandhu GS, Gilkeson RC, Grisworld MA, Gulani V. Applications of time-resolved MR angiography. Am J Roentgenol. 2011;196:W613–620.
Derchi LE, Balconi G, De Flaviis L, Oliva A, Rosso F. Sonographic appearances of hemangiomas of skeletal muscle. J Ultrasound Med. 1989;8:263.
Barakat MJ, Hirehal K, Hopkins JR, Gosal HS. Synovial haemangioma of the knee. J Knee Surg. 2007;20:296–8.
Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997;17:675–91.
Huang GS, Lee CH, Chan WP, Chen CY, Yu JS, Resnick D. Localised nodular synovitis of the knee: MR imaging appearance and clinical correlates in 21 patients. Am J Roentgenol. 2003;181:539–43.
Bravo SM, Winalski CS, Weissman BN. Pigmented villonodular synovitis. Radiol Clin N Am. 1996;34:311–26.
Kottal RA, Vogler JB, Matamoros A, Alexander AH, Cookson JL. Pigmented villonodular synovitis: a report of imaging in two cases. Radiology. 1987;163:551–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Source of founding
None.
Conflict of interest
No conflict of interest.
Rights and permissions
About this article
Cite this article
Wen, D.W., Tan, T.J. & Rasheed, S. Synovial haemangioma of the knee joint: an unusual cause of knee pain in a 14-month old girl. Skeletal Radiol 45, 827–831 (2016). https://doi.org/10.1007/s00256-016-2356-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2356-0