Abstract
Background
Synovial hemangioma is a benign intra-articular tumor. This condition is rare and unfamiliar soft tissue tumor to most orthopedic surgeons. Delayed diagnosis causes osteoarthritic damage and the destruction of joint structures due to infiltrating tumor growth. We discuss the patterns of tumor location and the appropriate surgical procedure for this condition.
Methods
Ten patients were treated surgically in our department. These comprised five males and five females ranging in age from 0 to 17 years (average age 12.4 years). Preoperative diagnosis was made using clinical findings, plain radiographs and magnetic resonance imaging. The follow-up time after surgery was at least 3 years.
Results
The main symptom was pain. Three cases revealed hemarthrosis. The range of motion of the affected knee joint was limited in five cases. The average time between onset of pain and diagnosis was 3 years. Tumor location was classified into three patterns: (1) anterior patellofemoral joint type in five, (2) posterior popliteal type in two and (3) diffuse proliferation type in two. Open arthrotomy with synovectomy was performed in all cases. No tumor recurrences were experienced after a minimum follow-up of 3 years.
Conclusion
Clinical symptom and magnetic resonance imaging are helpful to obtain the diagnosis and determine the extent of the lesion. Depending on the tumor location, synovial hemangioma in the knee joint can be classified into patellofemoral, popliteal and diffuse types. Open arthrotomy with sufficient tumor and synovectomy is important to prevent tumor recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Synovial hemangioma is a benign vascular tumor of soft tissue. Since Bouchut first reported this rare entity in 1856 [1], only a small number of pediatric patients have so far been reported [2,3,4].
Synovial hemangioma can occur at many sites including tendon sheaths, elbows, ankles and interphalangeal and temporomandibular joints. However, the highest incidence is found at the knee joint, accounting for 60% of all cases [5]. The symptoms usually appear in childhood and persist for several years prior to diagnosis. Because synovial hemangioma is a rare and unfamiliar soft tissue tumor to orthopedic surgeons, diagnosis can sometimes be delayed by more than 10 years [2, 5]. The main goal of treatment is early and radical surgical resection [6]. It remains controversial as to whether an open approach to the joint is preferred over arthroscopic surgery, especially in young children [7,8,9].
In this study, we reviewed ten cases with synovial hemangioma of the knee joint that were treated surgically in our department. We discuss the patterns of tumor location and the appropriate surgical procedure for this condition.
Patients and methods
Since 2010, ten patients with synovial hemangioma were treated surgically in our department. These comprised five males and five females ranging in age from 0 to 17 years (average age 12.4 years). Nine of the patients were teenagers.
Preoperative diagnosis was made using clinical findings, plain radiographs and magnetic resonance imaging (MRI). All patients underwent surgical excision by one surgeon (K.M.). Diagnostic arthroscopy was performed in three cases, followed by open resection immediately thereafter in two of these. Open tumor resection was performed in all cases. The diagnosis of synovial hemangioma was confirmed by histopathology. The follow-up time after surgery was at least 3 years (summarized in Table 1).
Results
Clinical symptoms
The main symptom associated with synovial hemangioma arising in the knee joint was pain. This was sometimes uncontrolled by pain killers. Three cases revealed hemarthrosis at the first visit to our hospital. The range of motion of the affected knee joint was limited in five cases. Only one case had a history of trauma, while four cases had a sports history of tennis, baseball and basketball.
Diagnosis and tumor location
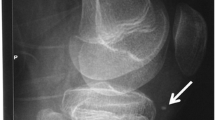
The average time between onset of pain and diagnosis of synovial hemangioma was 2.5 years (range 1–48 weeks). Patients frequently visited different clinics due to unknown diagnosis. Plain radiographs showed the presence of phleboliths in case 8 only. Diagnosis of synovial hemangioma was obtained by MRI showing a heterogeneous lesion with low signal on T1-weighted image and high signal on T2-weighted image. Tumor location was classified into three patterns: (1) anterior patellofemoral joint type (PF), (2) posterior popliteal type (popliteal) and (3) diffuse proliferative type (diffuse) (Fig. 1, Table 2). Six cases were PF type, comprised of three lateral PF, two medial PF and one Hoffa fad pad. Of the remaining four cases, two were popliteal type and two were diffuse. Some cases needed years until diagnosis, but the tumor remained in the popliteal area and did not extend to the anterior side.
Operative outcomes
In PF type synovial hemangioma, resection was relatively straightforward because the tumor formed a simple nodule. In contrast, diffuse and popliteal type synovial hemangioma invaded the posterior cruciate ligament and the posterior attachment of the meniscus and was therefore difficult to resect completely. No tumor recurrences were experienced after a minimum follow-up of 1 year, while the clinical symptoms showed good improvement in all cases (Table 1).
Case presentation
A 4-month-old female patient was presented at a pediatric clinic with swelling and loss of extension of the left knee joint and was subsequently referred to our university hospital. Range of motion was limited with extension of − 40° and flexion of 130°. Hemarthrosis was confirmed by aspiration of the joint. Skin hemangioma or other abnormalities were not found on the body. Radiographs showed mild swelling around the knee joint. MRI revealed joint effusion and an intra-articular diffuse lesion located in both the anterior and posterior knee joints. The intensity of the diffuse lesion was heterogeneous, with low signal on T1-weighted image and high signal on T2-weighted image. The preoperative diagnosis was intra-articular diffuse synovitis with suspected synovial hemangioma. To obtain a definitive diagnosis, we planned arthroscopic synovectomy (Fig. 2). Histological examination revealed a benign synovial hemangioma (Figs. 3, 4). Hemarthrosis and joint contracture did not improve even with physical therapy. Six months later, open surgery was performed from both the anterior and posterior sides. As much as possible, the synovial hemangioma was excised. The femur condyle was not smooth due to hemarthrosis. Six months after open surgery, the knee joint showed an almost full range of motion and no sign of hemarthrosis.
Discussion
Incidence and clinical symptoms
Synovial hemangioma of the knee joint is rare and therefore mostly unfamiliar to orthopedic surgeons. The first peak incidence is seen in the second decade of life. Moon reported the average age of onset was 10.9 years in girls and 12.5 years in boys, with 75% of patients being symptomatic prior to the age of 16 [5, 10]. There have been case reports of a 1-year-old patient [11] and of a 10-month-old boy [12]. Case 1 in our study (4 months old) may be the youngest patient reported to date with synovial hemangioma of the knee joint. De Gori et al. [13] described the oldest case of synovial hemangioma reported to date, a 67-year-old male with severe osteoarthritis who was treated by total knee arthroplasty. There are no reports in the literature of a familial occurrence for this disease.
The most common symptoms are limited range of motion, painful swelling, recurrent joint effusion and spontaneous atraumatic hemarthrosis [2, 5]. Similar to hemophilia, recurrent hemarthrosis leads to osteoarthritic changes and finally to the destruction of joint-articular structures [4]. Delayed diagnosis after the onset of symptoms can cause osteoarthritis [14]. Several authors have described cases with described a precedent trauma, suggesting that synovial hemangioma may represent a reactive lesion [15]. However, in our series only one case had a history of trauma. Four cases had experienced the opportunity for trauma due to a high level of sports activity.
Pathogenesis and classification
There is no agreement concerning the pathogenesis of synovial hemangioma. It can arise from any synovium-lined surface and can therefore be found in the course of tendons or in a joint space. The young age of patients raises the question of whether these lesions are more likely to be hamartomas, congenital malformations or true neoplasms [16,17,18].
Macroscopically, synovial hemangioma appears as a blue-red tuberous tumor. Hemangiomas are soft tissue tumors which are derived from endothelial cells. Devaney et al. [19] classified synovial hemangioma into four pathological categories based on their microscopic appearance: capillary, cavernous, mixed and venous. However, this classification does not appear to be useful when considering the therapeutic approach to use.
Based on anatomical site, articular hemangiomas are grouped into synovial, juxta-articular and intermediate [20]. The synovial type is located within the joint capsule and the juxta-articular type outside the joint. Based on a series of 29 cases, Bennett distinguished two types of synovial hemangioma: circumscribed, and diffuse with infiltration into other tissues [21]. The latter usually consisted of cavernous hemangioma, while the circumscribed type included capillary hemangioma. We propose a novel classification based on three patterns: PF, popliteal and diffuse type. The PF type is circumscribed [22], the popliteal type is juxta-articular, while the diffuse type is invasive to the PCL.
Diagnosis
Moon emphasized the difficulty in making a preoperative diagnosis [5]. The occurrence of non-specific symptoms means this diagnosis is often delayed [23]. Akgun et al. [24] reported the average persistence of symptoms was 4.5 years. Our cases showed 2.5 years in average between onset of pain and diagnosis. Okahashi et al. [2] reported a patient who had a 20-year previous history for her symptom. Case 8 in our study had a delayed diagnosis of 14 years. The presence of skin hemangioma can help with early diagnosis [19], although they were not observed in any of our patients. Differential diagnosis can include trauma, hematoma, hemophilia, ganglion, pigmented villonodular synovitis and synovial osteochondromatosis [5].
Plain radiographs usually show no specific findings for synovial hemangioma, but reveal more non-specific findings such as hemophilic arthropathy, bone erosion and soft tissue swelling [25]. The observation of intra-articular phleboliths is an important indicator of this condition, but was found in only one case in our study. MRI is helpful in determining the extent of the lesion and is the first choice of diagnostic procedure to use [26]. Synovial hemangiomas show low to intermediate signal intensity on T1-weighted image and high signal on T2-weighted image. Gadolinium always enhances the tumor due to the rich vascularity and is helpful in separating the tumor from fluid effusion. Doppler sonography can also be used to estimate the vascularization of hemangiomas [27].
Treatment
The main goal of treatment is early and radical surgical resection. Previous studies described several different therapy options, including embolization, open surgical excision with partial or complete synovectomy, arthroscopic excision or radiotherapy [6,7,8,9, 23, 28]. Radiotherapy has no clearly defined outcome and is not recommended for pediatric patients. Embolization seems useful if the tumor is of diffuse type and is fed by a large artery, although we have no experience with this treatment.
To date, several authors have recommended open surgery. We also recommend arthrotomy and sufficient excision of the tumor with good macroscopic view. Arthroscopic resection may be indicated only if the tumor is localized in the PF joint and its exact location identified by MRI. Even with the PF localized type, synovial hemangioma can invade into the Hoffa’s fad pad and arthroscopic excision would therefore not be indicated because tumor is invisible from joint space.
Bruns et al. [29] stated that recurrence should be avoidable with complete resection of the tumor. Recurrence due to insufficient tumor resection has been reported, but its rate is unknown. We suggest that recurrence represents the persistence of tumor following inadequate excision.
Conclusion
Synovial hemangioma is a rare and unfamiliar soft tissue tumor to most surgeons. It causes osteoarthritic damage and the destruction of joint structures due to infiltrating tumor growth. Awareness of the existence of synovial hemangioma is important in order to prevent late diagnosis. Depending on the tumor location, synovial hemangioma in the knee joint can be classified into PF, popliteal and diffuse types. As recommended already by several authors, open arthrotomy with sufficient tumor and synovectomy is important to prevent tumor recurrence. We successfully followed this procedure for our reported cases.
References
Bouchut E (1856) Tumeur erectile de l’articulation du genou. Gaz Hop 29:379–381
Okahashi K, Sugimoto K, Iwai M, Tanaka M, Fujisawa Y, Takakura Y (2004) Intra-articular synovial hemangioma; a rare cause of knee pain and swelling. Arch Orthop Trauma Surg 124:571–573
Aalberg JR (1990) Synovial hemangioma of the knee. A case report. Acta Orthop Scand 61:88–89
Holzapfel BM, Geitner U, Diebold J, Glaser C, Jansson V, Dürr HR (2009) Synovial hemangioma of the knee joint with cystic invasion of the femur: a case report and review of the literature. Arch Orthop Trauma Surg 129:143–148
Moon NF (1973) Synovial hemangioma of the knee joint. A review of previously reported cases and inclusion of two new cases. Clin Orthop Relat Res 90:183–190
Price NJ, Cundy PJ (1997) Synovial hemangioma of the knee. J Pediatr Orthop 17:74–77
Suh JT, Cheon SJ, Choi SJ (2003) Synovial hemangioma of the knee. Arthroscopy 19:27–30
Meislin RJ, Parisien JS (1990) Arthroscopic excision of synovial hemangioma of the knee. Arthroscopy 6:64–67
Shapiro GS, Fanton GS (1993) Intraarticular hemangioma of the knee. Arthroscopy 9:464–466
Watanabe S, Takahashi T, Fujibuchi T, Komori H, Kamada K, Nose M, Yamamoto H (2010) Synovial hemangioma of the knee joint in a 3-year-old girl. J Pediatr Orthop B 19:515–520
Abe T, Tomatsu T, Tazaki K (2002) Synovial hemangioma of the knee in young children. J Pediatr Orthop B 11:293–297
Ares-Rodriguez O, Soldado-Carrera F, Fontecha CG, Aguirre Canyadell M (2008) Synovial hemangioma in the knee of a 10-month-old boy. Arch Orthop Trauma Surg 128:583–584
De Gori M, Galasso O, Gasparini G (2014) Synovial hemangioma and osteoarthritis of the knee: a case report. Acta Orthop Traumatol Turc 48:607–610
Cotten A, Flipo RM, Herbaux B, Gougeon F, Lecomte-Houcke M, Chastanet P (1995) Synovial haemangioma of the knee. A frequently misdiagnosed lesion. Skeletal Radiol 24:257–261
Del Notaro C, Hug T (2003) Intra-articular hemangioma of the knee as a cause of knee pain. Arthroscopy 19:12–14
Dalmonte P, Granata C, Fulcheri E, Vercellino N, Gregorio S, Magnano G (2012) Intra-articular venous malformations of the knee. J Pediatr Orthop 32:394–398
Gould ES, Potter HG, Huvos A, Furie R, Crystal KS (1991) Case report 671: arteriovenous malformation of the right lower extremity with associated intraosseous hemangiomatosis. Skeletal Radiol 20:303–305
Krøner K, Fruensgaard S (1989) Synovial venous hemangioma of the knee joint. Arch Orthop Trauma Surg 108:253–254
Devaney K, Vinh TN, Sweet DE (1993) Synovial hemangioma: a report of 20 cases with differential diagnostic considerations. Hum Pathol 24:737–745
De Palma AF, Manler GG (1964) Haemangioma of synovial membrane. Clin Orthop Relat Res 32:93–99
Bennet GE, Cobey MC (1939) Hemangioma of joints; report of five cases. Arch Surg 38:487–500
Maeyama A, Saeki K, Hamasaki M, Kato Y, Naito M (2014) Deformation of the patellofemoral joint caused by synovial hemangioma: a case report. J Pediatr Orthop B 23:346–349
Lopez-Oliva CL, Wang EH, Cañal JP (2015) Synovial haemangioma of the knee: an under recognised condition. Int Orthop 39:2037–2040
Akgun I, Kesmezacar H, Ogut T, Dervisoglu S (2003) Intra-articular hemangioma of the knee. Arthroscopy 19:17
Greenspan A, Azouz EM, Matthews J, Decarie JC (1995) Synovial hemangioma: imaging features in eight histologically proven cases, review of the literature, and differential diagnosis. Skeletal Radiol 24:583–590
Llauger J, Monill JM, Palmer J, Clotet M (1995) Synovial hemangioma of the knee: MRI findings in two cases. Skeletal Radiol 24:579–581
Wen DW, Tan TJ, Rasheed S (2016) Synovial haemangioma of the knee joint: an unusual cause of knee pain in a 14-month old girl. Skeletal Radiol 45:827–831
Farkas C, Morocz I, Szappanos L, Szepesi K (1998) The importance of arthroscopy in diagnosing synovial haemangioma of the knee joint. Acta Chir Hung 37:17–22
Bruns J, Eggers-Stroeder G, von Torklus D (1994) Synovial hemangioma—a rare benign synovial tumor. Report of four cases. Knee Surg Sports Traumatol Arthrosc 2:186–189
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muramatsu, K., Iwanaga, R. & Sakai, T. Synovial hemangioma of the knee joint in pediatrics: our case series and review of literature. Eur J Orthop Surg Traumatol 29, 1291–1296 (2019). https://doi.org/10.1007/s00590-019-02431-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02431-5