Abstract
Objective
To determine current trends in postgraduate musculoskeletal ultrasound education across various medical specialties in the United States.
Materials and methods
A survey regarding musculoskeletal ultrasound education was sent to all program directors for diagnostic radiology and physical medicine rehabilitation residency programs, as well as adult rheumatology and sports medicine fellowship programs in the United States. The survey, sent in July 2015, queried the presence of formal musculoskeletal ultrasound training, the components of such training and case volume for trainees.
Results
Response rates were 23, 25, 28 and 33 % for physical medicine and rehabilitation, radiology, rheumatology and sports medicine programs, respectively. Among respondents, musculoskeletal ultrasound training was present in 65 % of radiology programs, 88 % of sports medicine programs, 90 % of rheumatology programs, and 100 % of physical medicine and rehabilitation programs. Most programs utilized didactic lectures, followed by hands-on scanning. The majority of programs without current training intend to implement such training within 5 years, although radiology programs reported the lowest likelihood of this happening. Most program directors believed that musculoskeletal ultrasound education is important for their trainees, and is of greater importance than it was 10 years ago. Case volume was lowest for radiology trainees and highest for sports medicine trainees.
Conclusion
Among respondents, the majority of diagnostic radiology programs offer musculoskeletal ultrasound training. However, this experience is even more widespread in other medical specialties, and hands-on training and experience tend to be greater in other specialties than in radiology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasound is a versatile method of diagnosing musculoskeletal pathology, and is useful in the assessment of a wide range of conditions [1]. The absence of radiation, relatively low cost, widespread availability, and dynamic capabilities of this modality have led to increased use of ultrasound in the evaluation of musculoskeletal complaints [2]. Given the increasingly cost-conscious healthcare environment in the United States, it is likely that musculoskeletal ultrasound use will continue to rise in the future.
In a recent survey of Society of Skeletal Radiology members, 49 % of respondents reported receiving musculoskeletal ultrasound training during their musculoskeletal radiology fellowship training [3]. However, subspecialty-trained musculoskeletal radiologists account for an extremely small percentage of all radiologists, with fewer than 200 fellowship positions per year in the United States compared to 4,735 positions for radiology residency [4, 5]. It is therefore likely that in many practice settings none of the radiologists will have subspecialty training in musculoskeletal radiology. In these practice settings, musculoskeletal imaging, including musculoskeletal ultrasound, would be interpreted by a radiologist using the skills and knowledge obtained during radiology residency. While training in ultrasound is a significant component of diagnostic radiology residency education, exposure to musculoskeletal ultrasound is currently not a mandated part of radiology residency [6].
Use of musculoskeletal ultrasound by non-radiology specialties has increased in recent years [2], particularly among physiatrists, rheumatologists, and sports medicine specialists. In fact, musculoskeletal ultrasound training has become a required component of training for physical medicine and rehabilitation (PM&R) residency programs [7], and exposure to musculoskeletal ultrasound is also a requirement for adult rheumatology fellowship programs [8]. Similarly, a standardized musculoskeletal ultrasound training curriculum has been proposed for sports medicine fellowship training programs [9].
The purpose of this study was to determine current trends in musculoskeletal ultrasound education among specialties likely to incorporate this imaging modality into their clinical practice. We focused on the postgraduate training level at which physicians were most likely to obtain this training in each specialty. We therefore surveyed diagnostic radiology and PM&R residency program directors, as well as adult rheumatology and sports medicine fellowship program directors.
Materials and methods
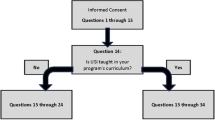
The study was exempted from review by the Institutional Review Board. We composed an online twelve question survey using Google Forms. The survey included a question regarding whether the program currently had formal musculoskeletal ultrasound training (yes/no question), as well as multiple choice questions regarding the type of training and number of cases interpreted and performed by trainees. Additionally, there were statements with 5-point Likert scale responses addressing trainee competence in musculoskeletal ultrasound, importance of musculoskeletal ultrasound training (including its relative importance now compared with 10 years ago), and likelihood of implementing such training for programs that currently do not have formal musculoskeletal ultrasound training. Demographic information was collected, and a free-text comment section was also present. (The full survey is available in Table 1.)
The survey was distributed in July 2015 to the program directors for all 184 Accreditation Council for Graduate Medical Education (ACGME)-accredited diagnostic radiology residency programs, 80 PM&R residency programs, 112 rheumatology (internal medicine subspecialty) fellowship programs, and 24 sports medicine (PM&R and emergency medicine subspecialty) fellowship programs. A link to the survey, along with a cover letter, was e-mailed directly to the program directors for rheumatology, PM&R and sports medicine programs using contact information obtained from the American Medical Association’s FREIDA online database of training programs (http://www.ama-assn.org/ama/pub/education-careers/graduate-medical-education/freida-online.page). The survey link and cover letter were distributed to radiology program directors through the Association of Program Directors in Radiology (APDR) electronic mailing list. A follow-up email with the survey link and cover letter was sent to all program directors in September 2015. Responses were tabulated by specialty, and descriptive statistics were performed. Pearson’s chi-squared test was used to compare response rates, with a P-value <0.05 indicating statistical significance.
Results
Response rates and demographics
The response rate was 23 % (18/80 programs) for PM&R, 25 % (46 respondents out of 184 programs) for radiology, 28 % (31/112 programs) for rheumatology and 33 % (8/24 programs) for sports medicine. These was no significant difference in response rate among the different specialties (P = 0.70). Responses were received from radiology, rheumatology and PM&R programs in 24, 14 and 12 different states, respectively, representing all regions of the United States. Additionally, responses were received from sports medicine programs in five different states (Table 2).
Formal musculoskeletal ultrasound training
Among respondents, formal musculoskeletal ultrasound training was present in 65 % (30 out of 46 respondents) of radiology residency programs, 88 % (7/8) of sports medicine fellowship programs, 90 % (28/31) of rheumatology fellowship programs, and 100 % of PM&R residency programs (Fig. 1).
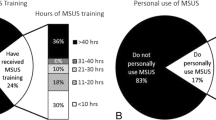
Components of musculoskeletal ultrasound training most commonly included didactic lectures (75, 93, 100 and 100 % of rheumatology, radiology, and PM&R and sports medicine programs, respectively), followed by hands-on scanning sessions using live models (47, 83, 86 and 96 % of radiology, PM&R, sports medicine and rheumatology programs, respectively) or cadavers (7, 25, 44 and 86 % of radiology, rheumatology, PM&R and sports medicine programs, respectively). Many programs also utilized hands-on interventional training sessions (20, 50, 72 and 100 % of radiology, rheumatology, PM&R and sports medicine programs, respectively). Electronic or web-based modules were least commonly employed (3, 22, 29 and 43 % of radiology, PM&R, rheumatology and sports medicine programs, respectively; Fig. 2).
Plans for implementation of musculoskeletal ultrasound training
Of the 16 radiology programs without current formal musculoskeletal ultrasound training, 50 % reported low or very low likelihood of introducing such training within the next 5 year, while 38 % (6/16) indicated a very high likelihood of providing such training within this time period. The three rheumatology programs and one sports medicine program without current musculoskeletal ultrasound training reported a very high likelihood of introducing such training within the next 5 years.
Trainee experience and perceived competence in musculoskeletal ultrasound
Radiology trainees on average performed and interpreted fewer diagnostic and interventional musculoskeletal ultrasound examinations than trainees in the other surveyed specialties (Figs. 3, 4 and 5). In addition, program directors in radiology perceived their trainees as having relatively low competence in the interpretation and performance of musculoskeletal ultrasound studies (mean response 2.3), while rheumatology, PM&R and sports medicine programs reported higher perceived levels of confidence in the ability of their trainees to perform and interpret musculoskeletal ultrasound studies (mean responses of 3.2, 3.6 and 4.4 for rheumatology, PM&R and sports medicine, respectively).
Perceived importance of musculoskeletal ultrasound training
Program directors from all specialties believed that musculoskeletal ultrasound is an important part of training; however, this was less strongly felt among radiology programs (mean response 3.7) than in sports medicine, rheumatology and PM&R programs (mean responses of 4.4, 4.4 and 4.6, respectively). Similarly, while programs directors in all specialties believed that musculoskeletal ultrasound training is more important now than it was 10 years ago, this was less strongly felt among radiology programs (mean response 3.9) than in rheumatology, PM&R and sports medicine programs (mean responses of 4.6, 4.8 and 5, respectively).
Respondents’ comments
A number of respondents submitted comments in the free-text section of the survey. Among radiology program directors, comments included limited number of musculoskeletal ultrasound cases referred to radiology as a result of these examinations being performed by physicians in the potential referring clinician’s service; lack of faculty experience in musculoskeletal ultrasound; difficulty in finding time for musculoskeletal ultrasound education; and relatively low use of this modality in the United States compared with other parts of the world. Several rheumatology program directors commented that their trainees attend musculoskeletal ultrasound courses outside of their institution in order to become competent in this modality, while others have courses fully integrated into their curriculum.
Discussion
Among respondents, formal musculoskeletal ultrasound training is currently present in the majority of diagnostic radiology, PM&R, rheumatology and sports medicine training programs in the United States. Various educational methods are utilized, including didactic lectures, hands-on scanning sessions using models or cadavers, hands-on interventional sessions, and electronic or web-based modules.
Among respondents, radiology programs have the lowest prevalence of formal musculoskeletal ultrasound education. Additionally, among programs with such training, radiology programs also demonstrate the lowest frequency of hands-on musculoskeletal ultrasound training, with training primarily based on didactic lectures. The average number of musculoskeletal ultrasound cases performed and interpreted by radiology trainees also was less than that for trainees in other specialties. As such, it is not surprising that radiology program directors are least confident in the ability of their trainees to perform and interpret musculoskeletal ultrasound examinations.
Program directors across all surveyed specialties agreed that musculoskeletal ultrasound is an important aspect of training, and that it is more important now than it was 10 years ago. While most programs without formal musculoskeletal ultrasound training intend to implement such training within the next 5 years, radiology program directors indicate a lower likelihood of this occurring than other programs.
There are a number of potential barriers to implementation of musculoskeletal ultrasound training, as indicated by survey respondents. Of particular relevance to radiology, several programs indicated a low number of referred musculoskeletal ultrasound cases, which may result from potential referring clinicians performing these examinations on their own or the preference of referring physicians to have musculoskeletal pathology evaluated by other imaging modalities. An additional barrier to implementation is lack of faculty knowledgeable in this imaging modality, which mirrors the findings of the recent survey of Society of Skeletal Radiology members in which only 49 % of respondents had received ultrasound training during musculoskeletal radiology fellowship [3].
There are a variety of continuing medical education musculoskeletal ultrasound courses offered by professional societies, academic medical centers and private companies. These courses typically include hands-on ultrasound training, and could be of benefit for departments which lack faculty proficient in musculoskeletal ultrasound. Attending these courses could serve as the basis for musculoskeletal ultrasound training, or to supplement and reinforce current faculty knowledge. Additionally, the use of “peer teachers,” residents or fellows who receive brief, focused training in musculoskeletal ultrasound prior to workshops for other trainees, may allow implementation of hands-on ultrasound training more easily. Peer teaching has been successfully utilized in a number of programs [10–12].
A significant limitation of this study is the relatively low response rate, although we considered a number of factors which have been shown to affect the response rate when designing this survey. These factors include maintaining consistency in design elements throughout the survey (for example, italics should have the same meaning throughout the survey), articulating questions and response options clearly, and minimizing the use of graphics and animations in the survey [13]. Additionally, shorter surveys have higher response rates than longer ones [14], and the use of financial incentives and paper surveys (as opposed to electronic surveys) also improve response rates [15]. Finally, follow-up reminders improve survey response rates, particularly with mail surveys (as opposed to web surveys) [16]. Another limitation of this study is potential responder bias which is inherent to surveys, although it has been suggested that nonresponse bias is less of a concern in surveys of physicians [14].
In summary, acknowledging the low response rate, we found that didactic musculoskeletal ultrasound education is currently present in the majority of respondent radiology residency programs in the United States. However, it is even more widespread in PM&R, rheumatology and sports medicine training programs, and trainees in those specialties tend to have more hands-on experience. Barriers to implementation of musculoskeletal ultrasound training in radiology residency programs include lack of cases and limited faculty experience in this modality. Various training models such as the use of peer teachers, may help address some of these concerns and allow programs to integrate musculoskeletal ultrasound education into their curricula more easily. In order to maintain a strong presence in this field, it is crucial for radiology residency programs to develop formal musculoskeletal ultrasound training and demonstrate competence of their trainees in this modality.
References
Klauser AS, Tagliafico A, Allen GM, et al. Clinical indications for musculoskeletal ultrasound: a Delphi-based consensus paper of the European Society of Musculoskeletal Radiology. Eur Radiol. 2012;22:1140–8.
Sharpe RE, Nazarian LN, Parker L, Rao VM, Levin DC. Dramatically increased musculoskeletal ultrasound utilization from 2000 to 2009, especially by podiatrists in private offices. J Am Coll Radiol. 2012;9:141–6.
Yablon CM, Wu JS, Newman LR, Downie BK, Hochman MG, Eisenberg RL. A needs assessment of musculoskeletal fellowship training: a survey of practicing musculoskeletal radiologists. AJR Am J Roentgenol. 2013;200:732–40.
Society of Skeletal Radiology website. MSK fellowships. https://skeletalrad.org/msk-fellowships. Accessed November 22, 2015.
ACGME website. Number of accredited programs, academic year 2015–2016, United States. https://apps.acgme.org/ads/Public/Reports/ReportRun?ReportId=3&CurrentYear=2015&AcademicYearId=2015. Accessed August 3, 2015
ACGME program requirements for graduate medical education in diagnostic radiology. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/420_diagnostic_radiology_07012015.pdf. Accessed August 3, 2015.
ACGME program requirements for graduate medical education in physical medicine and rehabilitation. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/340_physical_medicine_rehabilitation_07012015.pdf. Accessed August 3, 2015.
ACGME program requirements for graduate medical education in rheumatology (internal medicine). Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/150_rheumatology_int_med_07132015.pdf. Accessed August 3, 2015.
Finnoff JT, Berkoff D, Brennan F, et al. American medical society for sports medicine recommended sports ultrasound curriculum for sports medicine fellowships. Br J Sports Med. 2015;49:145–50.
Luz J, Siddiqui I, Jain NB, et al. Resident-perceived benefit of a diagnostic and interventional musculoskeletal ultrasound curriculum: a multifaceted approach using independent study, peer teaching, and interdisciplinary collaboration. Am J Phys Med Rehabil. 2015;94:1095–103.
Ahn JS, French AJ, Thiessen ME, Kendall JL. Training peer instructors for a combined ultrasound/physical exam curriculum. Teach Learn Med. 2014;26:292–5.
Knobe M, Münker R, Sellei RM, et al. Peer teaching: a randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44:148–55.
Klabunde CN, Willis GB, McLeod CC, et al. Improving the quality of surveys of physicians and medical groups: a research agenda. Eval Health Prof. 2012;35:477–506.
Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20:61–7.
Martins Y, Lederman RI, Lowenstein CL, et al. Increasing response rates from physicians in oncology research: a structured literature review and data from a recent physician survey. Br J Cancer. 2012;106:1021–6.
Shih TH, Fan X. Comparing response rates from web and mail surveys: a meta-analysis. Field Methods. 2008;20:249–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
This articles does not contain patient data.
Rights and permissions
About this article
Cite this article
Berko, N.S., Goldberg-Stein, S., Thornhill, B.A. et al. Survey of current trends in postgraduate musculoskeletal ultrasound education in the United States. Skeletal Radiol 45, 475–482 (2016). https://doi.org/10.1007/s00256-015-2324-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2324-0