Abstract
Objective
To develop clinical guidelines for musculoskeletal ultrasound (MSKUS) referral in Europe.
Methods
Sixteen musculoskeletal radiologists from seven European countries participated in a consensus-based interactive process (Delphi method) using consecutive questionnaires and consensus procedure meetings at several European radiology meetings. The evaluation of musculoskeletal diseases was established by literature reviews, followed by consensus on clinical utility in three consensus meetings. This involved a thorough, transparent, iterative approach which including interview, questionnaire, Delphi and standard setting methodologies. European MSK radiologists with a special interest in MSKUS formed two different expert groups who worked on reaching a consensus in the first two meetings. The third meeting resolved questions that did not achieve a consensus level of 67% using the first two questionnaires.
Results
On expert consensus, the use of MSKUS is indicated to detect joint synovitis, fluid and septic effusion for potential aspiration, and poorly indicated to detect loose bodies. Recommendations for most appropriate use of musculoskeletal ultrasound are reported in six areas relevant to musculoskeletal ultrasound: hand/wrist, elbow, shoulder, hip, knee and ankle/foot.
Conclusion
A comprehensive evidence-based, expert consensus-defined educational framework on clinical ultrsound is presented. This should facilitate referrals for this important imaging technique throughout Europe.
Key Points
• Musculoskeletal ultrasound is indicated for detecting joint synovitis, effusions and fluid collections.
• Musculoskeletal ultrasound is poor at detecting loose bodies.
• Musculoskeletal ultrasound is relevant for most joints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In clinical practice, the use of musculoskeletal ultrasonography is increasing among radiologists and non-radiologists. In the United States, musculoskeletal ultrasound usage nearly quadrupled between 2000 and 2008, driven primarily by increased utilisation by non-radiologists [1]. Musculoskeletal ultrasonography is also an expanding area in Europe.
In busy daily clinical practice, indications for this imaging technique are frequently based on the experience of the referring physician and sonographer. Moreover, recent refinements in ultrasound technology, such as broadband transducers, allow the evaluation of both superficial and deep tissues [2]. The wide availability of ultrasound equipment, the non-invasiveness and improved technology has placed ultrasound as one of the preferred first-line imaging techniques for investigating musculoskeletal disorders. However, the technique lacks clear evidence of its effectiveness in many clinical settings. Therefore, it is difficult to make strong “evidence-based” recommendations to guide a referring physician as to what is appropriate to be evaluated by US in clinical practice. The need for stronger evidence is illustrated by the lack of published meta-analyses on musculoskeletal ultrasound clinical indications in the radiological literature.
Appropriate use of imaging is essential for accurate patient diagnosis and management as well as optimising the use of healthcare resources. The European Society of Musculoskeletal Radiology (ESSR) evaluated the evidence currently available on the clinical value and indications for musculoskeletal ultrasound. The purpose of this study is to report the result of the Delphi process made by ESSR experts and to present clinical guidelines for musculoskeletal ultrasound in Europe.
Methods and materials
Study design
A 4-step consensus defining approach utilising the Delphi method [3, 4] and a panel of European experts in musculoskeletal ultrasound were used. The Delphi method is based on the premise that collective beliefs are generally more trustworthy than the beliefs of a single person, representing an efficient procedure to generate knowledge [4]. With this method, opinions, expertise and critical thinking are systematised. Individual feedback on a topic, judgment of the group’s work, opportunities to change opinion are warranted and anonymous [4].
The first step consisted of three parts: expert selection, anatomical area selection and questionnaire preparation. The subsequent three steps included a Delphi round each.
Step 1
Identification of musculoskeletal ultrasound experts
Experts were chosen by the European Society of Musculoskeletal Radiology on the basis of proven experience in practice, research and teaching in musculoskeletal ultrasound. MSKUS experts with more than 7 years of experience, regularly performing US examinations and belonging to the teaching group of the ESSR were suitable for the role. Experts were divided into two groups to reinforce independent expert opinions.
A total of 16 musculoskeletal radiologists representing 7 European countries (Austria, Belgium, Denmark, France, Italy, The Netherlands and United Kingdom) were chosen.
Anatomical areas selection
The chosen areas were: hand/wrist, elbow, shoulder, hip, knee and ankle/foot. These areas correspond to those previously identified by the ESSR to develop technical guidelines. An expert panel for each area carried out a systematic search for and analysis of the literature on the six topics.
Content validity was achieved by literature research on 6 anatomical areas/topics relevant to musculoskeletal ultrasound. Moreover, the experts identified the most important clinical conditions to be evaluated for each anatomical area. Literature research was performed before December 2010 and updated to August 2011 considering only papers with higher (from A to C) levels of evidence (EL). Clinical indications for ultrasound were first identified by Medline/PubMed reviews and The Oxford Centre for Evidence-based Medicine [5]; suggested EL were then used to evaluate each clinical indication according to study design and critical appraisal of prevention, diagnosis, prognosis, therapy and harm studies with the following definitions:
-
Level A: Consistent randomised controlled clinical trial, cohort study, all or none clinical decision rules validated in different populations.
-
Level B: Consistent retrospective cohort, exploratory cohort, outcomes research, case–control study; or extrapolations from level A studies.
-
Level C: Case-series study or extrapolations from level B studies.
-
Level D: Expert opinion without explicit critical appraisal, or based on physiology, bench research of first principles.
Each clinical indication was graded according to the Oxford Centre for Evidence-Based Medicine, based on the level of evidence (EL).
A grading system to be used in scoring sheets for each of the clinical conditions was prepared. This grading was used to achieve expert consensus on clinical conditions with lower levels of literature evidence.
The following grading was established in consensus:
-
Grade 0: US not indicated
-
Grade 1: US indicated if other imaging techniques are not appropriate
-
Grade 2: US indication equivalent to other imaging investigations (other investigations might provide significant information)
-
Grade 3: US is first choice level technique (other investigations rarely provide more information)
This grading was also used during the consensus meetings for implementation of expert opinions in cases, where literature evidence was missing or anecdotal. Several consensus procedures were evaluated regarding clinical utility of the sonographic evaluation of musculoskeletal diseases.
Steps 2–4
The first consensus was obtained between 2008 and 2009 by the first expert group with incorporation of the results from literature research in four meetings which took place at the European Congress of Radiology (ECR) and European Society of Musculoskeletal Radiology (ESSR)
The second consensus was obtained by the second expert group as an independent result. The first two consensuses used a modified Delphi method until a minimum agreement level as high as 67% was achieved.
The third and final consensus obtained at the ECR 2010, included all experts. The third consensus meeting resolved questions that achieved a consensus lower than 67%. The Delphi process allowed a change of view from a previously held position without any influence on the individual vote. Moreover, anonymity reduced the effects of group interaction and leaders influence. All relevant stakeholders attributed a grade (strength) of recommendation (RG) from 0 to 3 for each clinical indication.
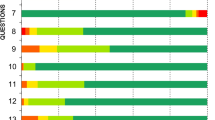
Statistical analysis
Group agreement with the clinical condition under consideration was defined as total cumulative agreement >67% after the second or third Delphi round. Group consensus was defined if the consensus level of agreement (CLA) was >90% for each anatomical area/topic. The results have been presented as the total cumulative agreement after the last Delphi round on the basis of a four-point simplified Likert scale (agree; agree with minor reservation; agree with major reservation; disagree). Statistical analysis was performed by the authors under the supervision of a biostatistician specialised in medical research.
The format of recommendations for clinical indication comprised the clinical condition, its level of evidence (EL), the strength of recommendation (RG) and the percent agreement (CLA).
Funding sources
With respect to the voting process, 100% of participants agreed that no sponsor influenced their vote. The study did not receive any financial support.
Results
Upper limb
Hand/wrist
Before December 2010, 67 published articles had been evaluated [5–68]. Before August 2011, 16 published articles (case reports excluded) were added [25, 69–83]. No level A studies were found.
Thirty-six clinical conditions were identified and group consensus was reached. Joint synovitis obtained an EL of B with a RG of 3 on expert consensus. For ulnar side wrist pain, FCU/FCR and Abutment syndrome obtained an EL of D with RGs of 3 and 0, respectively. After the second round, the CLA was 42%, which was below the threshold value of 67%; after the third meeting, the overall CLA was 83%.
Detailed results for EL and RG after the third round are reported in Table 1 .
In the hand/wrist area, the result of the concensus was that use of musculoskeletal ultrasound is not indicated for haemate fractures, triangular fibrocartilage complexes, capitate fractures, Kienbock’s disease or haemato-lunate impingements. Volar plate avulsions, scaphoid fractures and scapholunate ligament injuries had a GR of 1. An EL of A has not been reported for the hand/wrist area.
Elbow
Before December 2010, 56 published articles had been evaluated [83–139]. Before August 2011, 13 published articles (case reports excluded) were added [140–153]. 21 clinical conditions were identified and group consensus was reached. Joint synovitis and septic arthritis/effusion obtained an EL of B with a RG of 3 from expert consensus. For seven clinical conditions no EL was assigned. An EL of C was assigned to triceps tendon problems after the second round of literature research. Ulnar nerve neuropathy and supracondylar elbow fracture/postoperative positioning obtained an EL of B with a RG of 3 and 0, respectively. After the second round, the CLA was 90%, which was above the threshold value of 67%; after the third meeting, the overall CLA was 90% as well.
Detailed results for EL and RG after the third round are reported in Table 2.
At the level of the elbow, the use of musculoskeletal ultrasound was deemed not indicated for lateral collateral ligament, lateral condyle fracture in children/ fractures and supracondylar elbow fracture/postoperative positioning with a RG of 0, and for radial head subluxation/fracture and loose bodies with RG of 1. An EL of A has been reported for lateral epicondylitis with a RG of 3.
Shoulder
Before December 2010, 96 papers had been evaluated [154–249]. Before August 2011, 10 published articles were added (case reports excluded) [250–259]. 23 clinical conditions were identified and group consensus was reached.
Septic arthritis/effusion obtained an EL of C with a RG of 3 upon expert consensus. After the second round, the CLA was 88%, which is above the threshold value of 67%; after the third meeting, the overall CLA was 100%. Detailed results for EL and RG after the third round are reported in Table 3.
At the level of shoulder, the use of musculoskeletal ultrasound is not indicated for adhesive capsulitis, gleno-humeral joint traumatic and dynamic instability, and Parsonage-Turner syndrome with a RG of 0 and for rotator cuff muscle atrophy, loose bodies, quadrilateral space syndrome and thoracic outlet syndrome with RG of 1. An EL of A was reported for full thickness and partial thickness cuff tears with a RG of 3 and 2, respectively.
Lower limb
Ankle/foot
Before December 2010, 42 original papers have been evaluated [260–301]. Before August 2011, 13 papers have been added and only papers with elevated EL were evaluated [302–314]. 28 clinical conditions were identified and group consensus was reached.
Joint effusion and synovitis obtained an EL of C–D and A with a RG of 3 upon expert consensus. After the second round, the CLA was 96%, which was above the threshold value of 67%; after the third meeting, the overall CLA was 96% and the RG for bony avulsion turned from 0 to 1. Detailed results for EL and RG after the third round are reported in Table 4.
At the level of the ankle/foot, the result of the concenus was that use of musculoskeletal ultrasound is not indicated for posterior talo-fibular ligaments, intraarticular diseases, cartilage lesions and fractures of the distal tibia or talus and tarsal coalition with a RG of 0, and for deltoid and spring ligament injuries and bony avulsion with an RG of 1. An EL of A has been reported for tendon tears, tendon sheath effusions, peroneal dislocations, calcific tendinitis, retrocalcaneal bursitis, anterior talo-fibular ligaments, calcaneo-fibular ligaments, ganglion cysts, nerve entrapments and Morton’s neuromas with a RG of 3.
Knee
Before December 2010, 187 relevant original papers had been included [84, 85, 208, 211, 314–487]. Between January 2011 and August 2011, ten papers were added and evaluated [488–497]. 29 clinical conditions were identified and group consensus was reached.
Joint effusion, synovitis and septic arthritis obtained an EL of A or B with a RG of 3 on consensus. Synovial tumors obtained an EL of B with a RG of 0 on expert consensus.
After the second round, the CLA was 96%, above the threshold value of 67%; after the third meeting, the overall CLA was 96% as well, and RG for meniscal tears turned from 1 to 0.
Detailed results for EL and RG after the third round are reported in Table 5.
At the level of the knee, the use of musculoskeletal ultrasound is not indicated for osteochondritits dissecans, plica syndrome, cruciate ligaments or meniscal tears, and fractures with a RG of 0. Musculoskeletal ultrasound was considered not indicated for posterolateral corner lesions (biceps femoris tendon, lateral collateral ligament, popliteus tendon), intraarticular ganglion, Hoffa’s fat pad syndrome and loose bodies with RG of 1. An EL of A with RG of 3 has been reported for patellar tendinopathy/tear, quadriceps tendinosis/tear, Baker’s cyst, periarticular bursitis and ganglion, Osgood-Schlatter, Sinding-Larsen and nerve abnormalities.
Hip
Before December 2010, 52 original papers had been evaluated [498–549]. Between January 2011 and August 2011, five papers were evaluated [550–553]. 21 clinical conditions were identified and group consensus was reached. 4/21 clinical conditions were added in the third consensus (psoas tendon problems, hamstrings, trochanteric pain, growing pain).
Synovitis, effusion and synovial cysts obtained an EL of A with a RG of 2 on expert consensus. Septic effusion obtained an EL of D with a RG of 3 because of the possibility to perform US-guided aspiration on expert consensus.
After the second round, the CLA was 88%, above the threshold value of 67%; after the third meeting, the overall CLA was 90%.
Detailed results for EL and RG after the third round are reported in Table 6.
At the level of the hip, musculoskeletal ultrasound was deemed not indicated for intra-articular snapping hip, osteoarthritis, and labral tears with a RG of 0. Musculoskeletal ultrasound was not indicated also for low-grade muscle injuries, psoas tendon problems, trochanteric pain, sciatica and growing pain.
An EL of A with RG of 3 has been reported for fluid detection and extraarticualr snapping hip.
In summary:
-
Joint synovitis obtained a RG of 3 for all joints wrist, fingers, elbow, ankle and foot, knee (except the subtalar joint with grade 2).
-
Septic effusion obtained a RG of 3 for all joints because of its potential for diagnostic aspiration.
-
Loose bodies obtained a RG of 1 for all joints.
-
Fluid detection obtained a RG of 3 all joints (except the subtalar joint with grade 2).
Clinical conditions in which the use of musculoskeletal ultrasound was concluded to be highly indicated (with an RG of 3) are reported in Table 7.
Discussion
This paper represents a comprehensive and practical approach to the appropriate use of musculoskeletal ultrasound. Guidelines for musculoskeletal ultrasound, including training, have been developed among rheumatologists [554–560]. Differences among radiologists and rheumatologists regarding clinical indications and anatomic areas have been highlighted [560]. In the radiological literature, clinical indications for the use of musculoskeletal ultrasound are currently based on insufficient published data. The purpose of this study was to develop clinical guidelines for musculoskeletal ultrasound referral in Europe. The ESSR identified the field of clinical indications for musculoskeletal ultrasound as an area where a classical “evidence-based” approach may be supported by expert knowledge. For this reason, a Delphi method was considered appropriate.
The group of experts chose the six anatomical areas where musculoskeletal ultrasound is commonly employed. These areas correspond to those already identified by ESSR and for which clinical guidelines on how to perform the examination have been developed [561]. For each area, relevant pathological conditions or clinical conditions amenable to US examination have been selected on the basis of existing literature and expert opinion. The stakeholders who participated were all European radiologists who practice with a particular interest in musculoskeletal ultrasound. This kind of process ensured that the final results were evidence-driven and clinically relevant.
After the third round, group agreement (total cumulative agreement > 67%) was reached for every anatomical area, reflecting a substantial homogeneous belief among experts. At the level of the wrist/hand, the third round improved the total cumulative agreement from 42% to 83%. This data is mainly related to the disagreement (RG of 2 vs 3) among soft-tissue structures amenable under ultrasound examination at the level of the wrist and hand. In this area, a substantial agreement for the bony structures in which ultrasound may be used was present. Indeed, the use of musculoskeletal ultrasound is not indicated for hamates, triangulat fibrocartilage complexes, capitates, Kienbock, hamato-lunate impingements, volar plate avulsions, scaphoid and scapholunate ligaments with a GR of 1. At the level of the wrist, no clinical condition yielded an EL of A, reflecting a lack in the scientific literature. This highlights the need for research in this area.
At the level of the elbow, group consensus was reached reflecting a high level of agreement between experts, however, for seven clinical conditions no EL was assigned before December 2010. Triceps tendon problems received an EL of C after the second round of literature research. Not surprisingly, for evaluation of bony structures (lateral condyle fractures in children/ fractures and supracondylar elbow fracture), musculoskeletal ultrasound was considered not indicated.
At the level of the shoulder, group consensus was reached with a perfect (100%) agreement after the third round. For adhesive capsulitis, gleno-humeral joint traumatic and dynamic instability, and Parsonage-Turner syndrome, musculoskeletal ultrasound was not considered the technique of choice and magnetic resonance imaging should be preferred. Conversely, musculoskeletal ultrasound is highly indicated when full and partial thickness rotator cuff tears are suspected, with an EL of A.
In the lower limb, group consensus was reached for every anatomical area defined if the consensus level of agreement was > 90% for each anatomical area/topic.
In the lower limb, agreement scores between Delphi rounds changed only slightly, reflecting a homogeneous and well-established opinion among experts. A relatively high number of clinical conditions obtained a RG of 0, especially at the knee. This data indicated a higher level of agreement for lower limb indications than upper limb. In summary, musculoskeletal ultrasound is highly indicated for detecting joint synovitis, effusions and fluid collections. Musculoskeletal ultrasound is poor at detecting loose bodies.
We believe that the clinical guidelines developed in this consensus are a useful tool for a rational use of musculoskeletal ultrasound in the clinical setting. The interactive and thorough process used strongly supports their use. The pre-evaluation evidence base was shown to be poor and clearly suggests that further high-quality research is needed for a better definition of evidence levels in this area. Moreover, we agree that ultrasound is a strategic issue for radiology and that radiological leaders have to support increased quality and visibility of US within the radiological community [562].
Author information
Authors and Affiliations
Corresponding author
Additional information
Due to the extensive amount of important references of this article, the list of references can be found in the online version of this article as supplementary material.
Electronic supplementary material
Below is the link to the electronic supplementary material.
References
(PDF 206 kb)
Rights and permissions
About this article
Cite this article
Klauser, A.S., Tagliafico, A., Allen, G.M. et al. Clinical indications for musculoskeletal ultrasound: A Delphi-based consensus paper of the European society of musculoskeletal radiology. Eur Radiol 22, 1140–1148 (2012). https://doi.org/10.1007/s00330-011-2356-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2356-3