Abstract
Published data on the diagnosis of bone metastases of prostate cancer are conflicting and heterogeneous. We performed a comprehensive meta-analysis to compare the diagnostic performance of choline-PET/CT, MRI, bone SPECT, and bone scintigraphy (BS) in detecting bone metastases in parents with prostate cancer. Pooled sensitivity, specificity, and diagnostic odds ratios (DOR) were calculated both on a per-patient basis and on a per-lesion basis. Summary receiver operating characteristic (SROC) curves were also drawn to obtain the area under curve (AUC) and Q* value. Sixteen articles consisting of 27 studies were included in the analysis. On a per-patient basis, the pooled sensitivities by using choline PET/CT, MRI, and BS were 0.91 [95 % confidence interval (CI): 0.83–0.96], 0.97 (95 % CI: 0.91–0.99), 0.79 (95 % CI: 0.73–0.83), respectively. The pooled specificities for detection of bone metastases using choline PET/CT, MRI, and BS, were 0.99 (95 % CI: 0.93–1.00), 0.95 (95 % CI: 0.90–0.97), and 0.82 (95 % CI: 0.78–0.85), respectively. On a per-lesion basis, the pooled sensitivities of choline PET/CT, bone SPECT, and BS were 0.84 (95 % CI: 0.81–0.87), 0.90 (95 % CI: 0.86–0.93), 0.59 (95 % CI: 0.55–0.63), respectively. The pooled specificities were 0.93 (95 % CI: 0.89–0.96) for choline PET/CT, 0.85 (95 % CI: 0.80–0.90) for bone SPECT, and 0.75 (95 % CI: 0.71–0.79) for BS. This meta-analysis indicated that MRI was better than choline PET/CT and BS on a per-patient basis. On a per-lesion analysis, choline PET/CT with the highest DOR and Q* was better than bone SPECT and BS for detecting bone metastases from prostate cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the fourth most common cancer worldwide, the most common cancer in men, and the second most common malignant cause of death in 2011. In the USA, 241,740 new cases were diagnosed in 2012 [1]. Most frequently, metastases occur in regional lymph nodes as well as in bone; visceral metastases (e.g., lung and liver) occur usually in the late stages, and bone metastases are present in 90 % of patients who die of this disease [2, 3]. The detection of metastases has a prognostic value, significantly evaluates the accuracy for staging, and alters the approach to treatment. Therefore, the imaging of bone metastases is of paramount importance in the management of patients with prostate cancer. Patients with bone metastases may not need local treatment such as surgery or local radiotherapy, but may be eligible for hormone therapy or chemotherapy [4, 5].
Thanks largely to its sensitivity, availability, and affordability, in most institutions, bone scintigraphy (BS) with 99 m-technetium methylene bisphosphonate (99mTc-MDP) remains the mainstay investigation for bony metastases in patients with prostate cancer [6]. The main deficiency of BS is its relative low specificity, because the uptake of the radiotracer is not tumor-specific. Moreover, it is difficult to distinguish between metastases and some pathological conditions such as trauma or surgery, degenerative changes, and infection, which result in false-positive bone scans [7]. Due to three-dimensional positional information provided by bone SPECT, the addition of bone SPECT to planar acquisition maintains the sensitivity and improves the PPV of BS for the detection of bone metastases, which is reported to be equal to other tomography-based techniques such as MRI and CT [8–10].
MRI involving non-radioactive contrast media has better sensitivity and specificity for detecting bone metastases than BS [11]. With the development of new sequences such as diffusion-weighted imaging (DWI), whole-body MRI, we can also detect extraskeletal involvement, including lymph nodes and other soft-tissue metastases. In addition, MRI allows assessment of tumor response in bone. Therefore, MRI plays an important role in detecting bone metastases in patients with prostate cancer.
PET/CT offers a combination of excellent pharmacokinetic characteristics, functional information, high resolution of PET modality, and detailed, precise anatomic localization and morphological correlation of tumor lesions of CT. It has proved itself as a noninvasive, metabolic imaging modality for diagnosing malignant disease as well as for assessing new therapies by dynamic acquisition and quantitative analysis [7]. Due to low glucose metabolism in most prostate cancer cells and urinary activity, the value of 18F-fludeoxyglucose (FDG) was limited in prostate cancer work-up [12]. Recent developments of new PET tracers such as 11C- and 18F-labeled choline, 11C-acetate, and 11C-methionine have shown promising results for the evaluation of bone metastasis in prostate cancer. To date, 11C- and 18F-labeled choline are the most commonly used PET tracers in prostate cancer imaging.
Choline, as an essential component of the phospholipids, is part of the cell membrane and the increase in cell proliferation as well as the activity of the enzyme choline kinase in prostate cancer cells is associated with an increase in choline as an indispensable component [13]. The most remarkable difference between 11C-choline and 18F-choline is the difference in their half-lives (20 min for 11C-choline vs. 110 min for 18F-choline). In addition, urinary excretion of 18F-choline is comparatively higher than that of 11C-choline, but the overall imaging methods are similar between the different choline agents [14]. Because of its high accuracy in the detection of bone metastases from prostate cancer, choline PET/CT is being increasingly evaluated and applied in the staging and assessment of prognosis for prostate cancer patients with bone metastases.
Despite the increasing numbers of publications concerning choline PET/CT, bone SPECT, MRI, and BS in the diagnosis procedure for bone metastases in patients with prostate cancer, the effectiveness of these modalities still remains unknown and no consensus has been reached. Thus, the aim of our study was to perform a meta-analysis to compare the diagnostic value of choline PET/CT, bone SPECT, MRI, and BS imaging in detecting bone metastases in patients with prostate cancer to provide better evidence-based advice to physicians in this area.
Materials and methods
Literature search
We searched the PubMed, EBSCO, EMBASE, Web of Knowledge, Ovid, and the Cochrane Library for articles about the diagnostic value of MRI, BS, bone SPECT, and choline PET/CT for detecting bone metastases in patients with prostate cancer. Published year was limited between January 1990 and November 2012. The following search algorithm was used for keywords: (prostate cancer OR prostate carcinoma) AND (bony metastases OR skeletal metastases OR osseous metastases OR bone metastases) AND (bone scan OR bone scintigraphy OR ECT OR emission computed tomography OR SPECT OR single-photon emission computed tomography OR MRI OR magnetic resonance imaging OR PET/CT OR positron emission tomography/computed tomography) AND (sensitivity OR specificity OR false-negative OR false-positive OR diagnosis OR detection OR accuracy). Studies in human subjects were chosen, without language limitation. In order to minimize the leak of checked articles, we also manually searched the reference lists. Moreover, we had a secondary retrieval for the references in included articles.
Selection criteria
The included articles in our analysis had to meet the selection criteria given as follows: (a) evaluating the diagnostic value of MRI, BS, bone SPECT, and choline PET/CT in detecting bone metastases from prostate cancer; (b) bone metastases from prostate cancer confirmed by surgery or histopathological analysis, or comprehensive diagnosis of other imaging techniques, or clinical and imaging follow-up for at least 6 months; (c) absolute numbers of true-positive, true-negative, false-positive, and false-negative results were provided or derived for either patient-based analysis or lesion-based analysis compared with the standard; (d) the study at least include ten or more patients; (e) when the data appeared in more than one article, the article with most details or recently published was included; in addition, although the articles showed results about a combination of different imaging modalities, we could also include the one that the performance assessment on an individual modality could be differentiated clearly.
Exclusion criteria
We excluded the articles as the following criteria: (a) case reports, letters, comments, animal experiments, review articles, and original articles with incomplete data; (b) radiopharmaceuticals used in the study were not about 99mTc-MDP for BS and choline for PET/CT, but others such as 131I, 99mTc-MIBI for BS, and 18F-FDG for PET/CT. These articles were also excluded; (c) repeatedly published literatures or similar literatures were also excluded.
Selection of articles and data extraction
Two investigators independently assessed and included the potentially eligible studies according to the inclusion and exclusion criteria mentioned above after reading the title and abstract. For the equivocal studies, we read the full text to make a decision. If there was still a disagreement, a third investigator evaluated the results and reached a consensus.
The same observers independently extracted relevant data from the included articles based on a standardized form, with disagreement resolved through discussion and consultation. It had been proven that some information such as the journal name, authors, and publication year did not influence the last analysis of the results, so observers were not blinded during data extraction [15].
We extracted the following common characteristics: (a) information and characteristics of study design, we could use the QUADAS (quality assessment of diagnostic accuracy studies) tool to evaluate the studies from each article in details. QUADAS criteria is a systematic, comprehensive quality-assessment tool for diagnostic accuracy of a study [16, 17]; (b) publication time, authors, sample size, age and gender of patients, the type of raw data, whether blinded or not, bias level (no bias: all cases were confirmed by pathology or surgery; some bias: partially confirmed by surgery or pathology), reference standard of various tests (surgery or histopathological analysis, or comprehensive diagnosis of other imaging techniques, or clinical follow-up for at least 6 months); (c) data about images or imaging techniques such as the amount and type of tracer for BS and PET/CT, magnetic field strength, and whether contrast agent used or not for MRI.
Quality assessment of each study and statistical analysis
The same researchers independently completed the quality assessment of each literature, reaching an agreement through discussion for the differences. There are 14 items in QUADAS criteria, and for each question there are three answers: “yes” “no”, and “unclear”. Due to answers to 14 questions, we should find out the reasons for bias and variation through comprehensive analysis.
We used the 2 × 2 tables to sort the data, including the numbers of the true-positive, true-negative, false-positive, and false-negative results both on a per-patient basis and on a per-lesion basis. Raw data provided by literature were separately analyzed for various diagnostic methods. According to guidelines of meta-analysis by Deville et al., we calculated the pooled sensitivity, specificity, and DOR with 95 % confidence intervals (CI). In addition, summary receiver operating characteristic (SROC) curves and the Q* index were also obtained. Then, we found out whether the differences of all indicators (sensitivity, specificity, DOR, and Q*) between different modalities were statistically significant by using the Z test. Statistical analyses were performed by using Microsoft Excel 2003, SPSS 13.0, and Meta-Disc 1.4. All p values presented were two-sided, and the result was considered significant only if the p value was less than or equal to 0.05 [18].
Results
Literature search
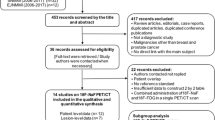
After the first computer search, there were a total of 895 articles identified. By reading the title and abstract of each article, according to the inclusion and exclusion criteria, we excluded 596 articles and then 209 articles by reading the full text. Reasons for the exclusion of the other 72 articles were as follows: not report data that could be used to construct or calculate true-positive, false-positive, true-negative, or false-negative numbers (n = 62); concerned other radiopharmacy imaging techniques such as 18F-NaF PET/CT and 99mTc-MIBI BS (n = 10). Finally, a total of 18 articles [2, 3, 11, 19–33] were included, consisting of nine studies for choline PET/CT, three studies for bone SPECT, six studies for MRI, and 12 studies for 99mTc-MDP BS (Fig. 1).
Study design characteristics
There were four retrospective studies [20, 25, 26, 30] and ten prospective studies [3, 11, 19, 21, 22, 27, 28, 31–33] in all included articles and we identified 13 studies [3, 11, 19–21, 23, 25, 26, 28–31, 33] analyzed on a per-patient basis, consisting of five studies for choline PET/CT, two for bone SPECT, six for MRI, 11 for BS, respectively, and ten studies [2, 3, 19, 20, 22, 24, 26, 27, 31–33] on a per-lesion basis, including seven studies for choline PET/CT, three for bone SPECT, one for MRI, five for BS, respectively. Patient enrollment was consecutive in seven studies and no document in the other 11 studies. A total of 12 researches were performed in Europe, three in Asia, and three in Australia. In total, there were 1,102 patients in selected researches, with the publication year ranging from 2006 to 2012. The characteristics of the included studies are presented in Table 1.
Some other relevant study characteristics about technical aspects were also available. For choline PET/CT, the amount of choline ranged from 250 to 555 MBq, especially 370 MBq was most used, and some researchers injected choline by 4.07 MBq/kg bodyweight. However, all choline PET/CT studies were acquired in a short time after injection. For MRI, all studies used 1.5-T and three used DWI sequences, two used STIR sequences, and only some with contrast agent used. As to BS, the type of tracer was 99mTc-MDP and the amount ranged from 600 to 925 MBq. Furthermore, 740 MBq was the most used in included research. In addition, bone SPECT was performed on a two or three-head rotating camera.
Quality assessment
We used the QUADAS quality assessment tool to evaluate each included study (Table 2). The table showed that we had optimal answers to questions 1, 2, 3, 4, 5, 7, 8, 9, 10, 12, 13, and 14. Due to the results of question 1, 2, and 3, patients in selected studies were included in accordance with strict criteria, which minimized the spectrum bias. There was also low risk of bias in other aspects such as disease progression (item 4), partial verification bias (item 5), incorporation bias (item 7), index test review (item 10), clinical data analysis (item 12), explanation of intermediate results (item 13) or withdrawals (item 14) and the description of the execution of index test (item 8) and the reference standard (item 9) was sufficient [16]. However, patients in most studies did not receive the same reference standard (item 6, only 24.1 % for “Yes”) and interpreters were not blind in the interpretation of reference standard results (item 11, 68.9 % for “No” or “Unclear”). Actually, it was difficult to use histopathological analysis or surgery as “the gold standard” to confirm bone metastases. Then, we chose a suboptimal reference standard: comprehensive diagnosis of other imaging techniques, or clinical and imaging follow-up for at least 6 months.
Summary of the diagnostic performance
As to per-patient, the pooled sensitivity, specificity, DOR, AUC, and Q* of those modalities are shown in Table 3. The pooled sensitivities by using choline PET/CT, MRI, and BS were 0.87 (95 % CI, 0.79–0.93), 0.95 (95 % CI, 0.90–0.98), 0.79 (95 % CI, 0.73–0.83), respectively. The pooled specificities for detection of bone metastases using choline PET/CT, MRI, and BS were 0.97 (95 % CI, 0.93–0.99), 0.96 (95 % CI, 0.92–0.98), and 0.82 (95 % CI, 0.78–0.85), respectively. The pooled DOR estimates for choline PET/CT, MRI, and BS were 150.70, 343.16, and 20.32, respectively. There were not enough data for meta-analysis of bone SPECT on a per-patient basis.
The SROC curves, AUC, and Q* index are shown in Fig. 2. We could conclude that MRI allowed for better diagnostic accuracy than choline PET/CT and BS (p < 0.05). The AUC for choline PET/CT, MRI, and BS were 0.9541, 0.9870, and 0.8876, and Q* values were 0.8961, 0.9514, and 0.8182, respectively.
The SROC curves for choline PET/CT, MRI, and BS on a per-patient basis. Each solid circle represents each study in the meta-analysis. The size of the circle indicates the study size. The AUC and Q* for choline PET/CT, MRI, and BS were 0.9541, 0.9870, and 0.8876 and 0.8961, 0.9514, and 0.8182, respectively. MRI showed better diagnostic accuracy than choline PET/CT and BS (p < 0.05). Choline PET/CT was better than BS (p < 0.05)
On a per-lesion basis, the pooled sensitivities of choline PET/CT, bone SPECT, and BS were 0.83 (95 % CI, 0.81–0.85), 0.90 (95 % CI, 0.86–0.93), and 0.59 (95 % CI, 0.55–0.63), respectively. The pooled specificities were 0.95 (95 % CI, 0.94–0.97) for choline PET/CT, 0.85 (95 % CI, 0.80–0.90) for bone SPECT, and 0.75 (95 % CI, 0.71–0.79) for BS. The pooled DOR estimates for choline PET/CT, bone SPECT, and BS were 99.78, 78.16, and 6.21, respectively. There were not enough data for meta-analysis of MRI. The AUC for choline PET/CT, bone SPECT, and BS were 0.9494, 0.9381, 0.7736, and Q* values were 0.8896, 0.8751, 0.7132, respectively. Results are shown in Table 3 and Fig. 3.
The SROC curves for choline PET/CT, bone SPECT, and BS on a per-lesion basis. The size of the circle indicates the study size. The AUC and Q* for choline PET/CT, bone SPECT, and BS were 0.9494, 0.9381, and 0.7736 and 0.8896, 0.8751, and 0.7132, respectively. The result showed that choline PET/CT and bone SPECT had better diagnostic accuracy than BS (p < 0.05)
Subgroup analysis
The result of the subgroup analysis for BS (prospective design vs. retrospective design) was also concluded in Table 3. For BS, the sensitivity, specificity, and DOR of prospective design studies were better than those of retrospective design studies on a per-patient basis.
Assessment of study heterogeneity
Because only a limited number of data points were available for bone SPECT on a per-patient basis and MRI on a per-lesion basis, we could not detect whether or heterogeneity was present in those studies. For per-patient, both sensitivity and specificity of MRI and BS were more highly heterogeneous compared to those of choline PET/CT. I2 index of choline PET/CT were 0.0 % for sensitivity, 2.8 % for specificity, of which sensitivity and specificity value were found to be homogeneous. However, for per-lesion, both sensitivity and specificity value for choline PET/CT, bone SPECT, and BS were highly heterogeneous. Results are shown in Table 4.
Discussion
In this meta-analysis, we found that MRI and choline PET/CT were more accurate than bone SPECT and BS for detecting bone metastases in patients with prostate cancer. As shown above, the sensitivity and specificity of MRI on a per-patient basis were 95 and 96 %, respectively, and those of choline PET/CT were approximately 87 and 97 %, respectively. Though choline PET/CT had the highest specificity on a per-patient basis, MRI was significantly better than choline PET/CT (p < 0.05) and BS (p < 0.05) for the detection of bone metastases from prostate cancer. The AUC estimates for MRI (0.9870) on a per-patient basis was also significantly higher than that of choline PET/CT (0.9541, p < 0.05), and that of BS (0.8876, p < 0.05). For per-lesion, choline PET/CT had higher AUC (0.9494) than bone SPECT (0.9381) and BS (0.7736).
Heterogeneity was analyzed to evaluate whether multiple studies included in this review were homogeneous, and thus to evaluate the accuracy of pooled diagnostic statistics and explore the influencing factors. According to Table 4, we found that except for the sensitivity and specificity values of choline PET/CT on a per-patient basis, other results were highly heterogeneous. In addition, some studies had different threshold settings that led to heterogeneity between studies. We therefore chose the random-effects model, which accounted not only for the heterogeneity but also for the error of estimation of these indexes for diagnostic study [34]. Because of limited data and the small sample size, we were not able to evaluate the publication bias, which proved to be a limitation of any meta-analysis. In addition, due to the subgroup analysis of BS in two aspects (retrospective design and prospective design), we concluded that diagnostic accuracy of prospective studies was higher than that of retrospective studies. There was no accepted gold standard, which may be a universal drawback to all studies for detecting bone metastases from various tumors with different modalities. In this study we had to use “comprehensive diagnosis of other imaging techniques, or clinical and imaging follow-up for at least 6 months” as the suboptimal reference standard while histopathological or surgery results could not be obtained for ethical reasons.
In prostate cancer, early detection of bone metastases is important for selecting an appropriate therapy, determining tumor staging, assessing a patient’s prognosis, and evaluating the efficacy of treatments [35–37], especially the extent of bone metastatic disease from prostate cancer is an independent prognostic factor [38]. In practice, choline PET/CT, MRI, bone SPECT, and BS are widely used for detecting bone metastases from prostate cancer. MRI offers anatomical and structural information, while BS and bone SPECT show functional imaging. They reflect the osteoblastic response to bone destruction by tumor cells in the cortex and the accompanying increase in blood flow, which is the visualization and measurement of biological processes at molecular and cellular levels using radio-labeled molecular probes [39, 40]. PET/CT provides both the anatomical description of CT and the metabolic processes and quantitative capabilities of PET, which bridges the gap between molecular imaging and systematic diagnosis.
BS has been used as a standard technique for the assessment of prostate cancer over last three decades because of its entire skeleton screening at once and widespread availability [41]. The compound (99mTc-MDP) is chemisorbed onto bone surfaces depending on local blood flow and osteoblastic activity. We can identify bone metastases as nearly all bone metastases are accompanied by an osteoblastic reaction [35]. However, it strikingly lacks diagnostic specificity, without distinguishing benign lesions (fracture, Paget’s disease, and so on) from metastatic lesions [41]. Moreover, false-negative bone scans can result from the absence of reactive changes and rapid growing of pure osteolytic metastases [42, 43]. Thus, in this meta-analysis, BS was shown to have the lowest specificity, DOR, and Q* index. It is reported that SPECT has optimized the use of planar BS, with sensitivity ranging from 87 to 92 % and specificity of about 91 % because of good morphological correlation [44, 45]. Nevertheless, bone SPECT alone sometimes can not provide adequate information for localization of bone lesions and are often insufficiently specific for diagnostic purposes [46].
MRI is an anatomical imaging modality on the basis of morphological appearance. Bone marrow metastases have longer T1- and T2-weighted relaxation times than normal marrow. Due to a high spatial resolution and high contrast between fat and metastases in the marrow, we can detect early metastases in the bones with large marrow cavities before any cortical destruction or reactive processes, while BS reflects osteoblastic response only in the cortex [47]. In the present study, MRI had better diagnostic value than choline PET/CT, BS, and bone SPECT on a per-patient basis. However, it also has a limitation in that MRI is less sensitive in detecting lesions in small curved flat bones like ribs. The reason for this is that cortical bone appears black on T1- and T2-weighted sequences [48].
In some included studies dealing with MRI and bone SPECT, the imaging protocols were deliberately limited to the entire axial skeleton or spine, which ignored the skull, ribs, and limbs in contrast to whole-body imaging. The probability of finding metastases in these locations with no metastases in the axial skeleton is indeed negligible, especially in prostate cancer, which predominantly metastasizes to the spine and pelvis [49–52]. Along with most relevant studies, any single case of isolated peripheral metastasis was hardly detected in prostate cancer patients with bone metastases. In addition, MRI detects early marrow involvement with a high spatial resolution because of the high contrast between fat and metastasis in the marrow, which allows for the early detection of metastasis in bones with large marrow cavities [41]. Bone SPECT is useful in evaluations of complex areas that are extensively surrounded by soft tissue such as the spine and pelvis. Therefore, as suggested previously, the approach did not result in any significant loss of accuracy in staging of patients with prostate cancer [3, 53]. Although whole-body MRI or bone SPECT is capable of meeting a variety of needs in a single examination, it has been questioned because of some limitations, especially the diagnosis of the skull and ribs on MRI images [47]. Additionally, the enormous increase in image data in whole-body MRI or bone SPECT not only implies an increase in evaluation time for the radiologist but also increases the potential for false-negative findings.
18F-FDG is the standard radiotracer in oncologic PET imaging; however, some results proved that FDG PET did not perform very well in prostate cancer patients, especially in well-differentiated prostate cancer. The reasons for this were probably renal excretion, bladder accumulation, and androgen ablation [54–56]. Due to elevated expression of the rate-limiting enzyme choline kinase in prostate cancer cells, many kinds of choline (11C-choline, 18F-fluorethyl-choline, or 18F-fluormethyl-choline) have been employed in studies [57]. It was demonstrated that 18F radio-labeled choline was better than FDG for detecting primary and metastatic prostate cancer. In practice, changes in metabolism occurred before a physical change or symptoms, which showed a great potential advantage in detecting metastases. However, because of its limited anatomical resolution, we could not describe bone metastases with the use of PET alone. Thus, the combination of PET and CT largely improved sensitivity, especially those false-negative PET findings [58]. In the present study, PET/CT was a better imaging modality than BS and bone SPECT on either a per-patient basis or a per-lesion basis. Moreover, PET/CT has several additional advantages: evaluation of osteolytic lesions in weight-bearing bones and particularly in the spine and pelvis [59], dynamic acquisition and quantitative assessment of choline allowing assessment of physiological bone remodeling, characterization of bone pathology and monitoring response to therapy [7].
Conclusions
In this meta-analysis, MRI was found to be better than choline PET/CT and BS on a per-patient basis, though choline PET/CT had the highest specificity. On a per-lesion analysis, choline PET/CT with the highest DOR and Q* was better than bone SPECT and BS for detecting bone metastases from prostate cancer. Among these modalities, BS had the lowest sensitivity and specificity while it is lowest in price. However, without enough eligible studies, we could not carry out available subgroup analysis. Higher-quality studies and more included articles with a large sample size are required for more available research in the future.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Beheshti M, Vali R, Waldenberger P, et al. The use of 18F-choline PET in the assessment of bone metastases in prostate cancer: correlation with morphological changes on CT. Mol Imaging Biol. 2009;11:446–54.
Giovanella L, Castellani M, Suriano S, et al. Multi-field-of-view SPECT is superior to whole-body scanning for assessing metastatic bone disease in patients with prostate cancer. Tumori. 2011;97:629–33.
Zerbib M, Zelefsky MJ, Higano CS, Carroll PR. Conventional treatments of localized prostate cancer. Urology. 2008;72:S25–35.
Berry WR. The evolving role of chemotherapy in androgen-independent (hormone-refractory) prostate cancer. Urology. 2005;65:2–7.
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003;23:341–58.
Beheshti M, Pirich C, Langsteger W. Conventional 99mTc-based bone scan versus fluoride positron emission tomography combined with computed tomography in the assessment of bone metastases in prostate cancer patients. Imaging Decisions MRI. 2009;13:88–96.
Kosuda S, Kaji T, Yokoyama H, et al. Does bone SPECT actually have lower sensitivity for detecting vertebral metastasis than MRI? J Nucl Med. 1996;37:975–8.
Nozaki T, Yasuda K, Akashi T, Fuse H. Usefulness of single-photon emission computed tomography imaging in the detection of lumbar vertebral metastases from prostate cancer. Int J Urol. 2008;15:516–9.
Ghanem N, Uhl M, Brink I, et al. Diagnostic value of MRI in comparison to scintigraphy, PET, MS-CT and PET/CT for the detection of metastases of bone. Eur J Radiol. 2005;55:41–55.
Lecouvet FE, Geukens D, Stainier A, et al. Magnetic resonance imaging of the axial skeleton for detecting bone metastases in patients with high-risk prostate cancer: diagnostic and cost-effectiveness and comparison with current detection strategies. J Clin Oncol. 2007;25:3281–7.
Effert PJ, Bares R, Handt S, Wolff JM, Bull U, Jakse G. Metabolic imaging of untreated prostate cancer by positron emission tomography with sup 18 fluorine-labeled deoxyglucose. J Urol. 1996;155:994–8.
Richter JA, Rodríguez M, Rioja J, et al. Dual tracer 11C-choline and FDG-PET in the diagnosis of biochemical prostate cancer relapse after radical treatment. Mol Imaging Biol. 2010;12:210–7.
Evangelista L, Guttilla A, Zattoni F, Muzzio PC, Zattoni F. Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate-to high-risk prostate cancer: a systematic literature review and meta-analysis. Eur Urol. 2012;63:1040–8.
Berlin JA. Does blinding of readers affect the results of meta-analyses? Lancet. 1997;350:185–6.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol. 2006;6:9.
Wu Y, Li P, Zhang H, et al. Diagnostic value of fluorine 18 fluorodeoxyglucose positron emission tomography/computed tomography for the detection of metastases in non–small–cell lung cancer patients. Int J Cancer. 2013;132:E37–47.
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-Fluoride PET/CT. J Nucl Med. 2006;47:287–97.
Fuccio C, Castellucci P, Schiavina R, et al. Role of 11C-choline PET/CT in the restaging of prostate cancer patients showing a single lesion on bone scintigraphy. Ann Nucl Med. 2010;24:485–92.
Lecouvet FE, El Mouedden J, Collette L, et al. Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace 99mTc bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur Urol. 2012;62:68–75.
McCarthy M, Siew T, Campbell A, et al. 18F-Fluoromethylcholine (FCH) PET imaging in patients with castration-resistant prostate cancer: prospective comparison with standard imaging. Eur J Nucl Med Mol Imaging. 2011;38:14–22.
Mosavi F, Johansson S, Sandberg DT, Turesson I, Sorensen J, Ahlstrom H. Whole-body diffusion-weighted MRI compared with 18F-NaF PET/CT for detection of bone metastases in patients with high-risk prostate carcinoma. AJR Am J Roentgenol. 2012;199:1114–20.
Nozaki T, Yasuda K, Akashi T, Fuse H. Usefulness of single-photon emission computed tomography imaging in the detection of lumbar vertebral metastases from prostate cancer. Int J Urol. 2008;15:516–9.
Picchio M, Fallanca F, Spinapolice E, et al. Comparison of 11C-choline PET/CT and bone scintigraphy in the detection of bone metastasis in patients with biochemical failure after primary treatment for prostate cancer. Eur J Nucl Med Mol Imaging. 2010;37:S269.
Picchio M, Spinapolice E, Fallanca F, et al. 11C-choline PET/CT detection of bone metastases in patients with PSA progression after primary treatment for prostate cancer: comparison with bone scintigraphy. Eur J Nucl Med Mol Imaging. 2012;39:13–26.
Poulsen MH, Petersen H, Hoilund-Carlsen PF, et al. Detection of bone metastases from prostate cancer: a prospective study of 99mTc-MDP bone scintigraphy, 18F-fluorocholine PET/CT, 18F-fluoride PET/CT compared with MRI. Eur Urol Suppl. 2012;11:e892.
Takesh M, Zechmann C, Haufe S, Afshar A, Haberkorn U. Diagnostic role of 18F-fluoroethylcholine-PET/CT compared with bone-scan in evaluating the prostate cancer patients referring with biochemical recurrence. Eur J Nucl Med Mol Imaging. 2011;38:S138.
Venkitaraman R, Cook GJ, Dearnaley DP, et al. Does magnetic resonance imaging of the spine have a role in the staging of prostate cancer? Clin Oncol. 2009;21:39–42.
Venkitaraman R, Cook GJ, Dearnaley DP, et al. Whole-body magnetic resonance imaging in the detection of skeletal metastases in patients with prostate cancer. J Med Imaging Radiat Oncol. 2009;53:241–7.
Wang XY, Zhang CY, Jiang XX. Prospective study of bone metastasis from prostate cancer: comparison between large field diffusion-weighted imaging and bone scintigraphy [Chinese]. Chin J Radiol. 2009;43:131–5.
Beheshti M, Vali R, Waldenberger P, et al. Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET-CT: a comparative study. Eur J Nucl Med Mol Imaging. 2008;35:1766–74.
Langsteger W, Balogova S, Huchet V, et al. Fluorocholine (18F) and sodium fluoride (18F) PET/CT in the detection of prostate cancer: prospective comparison of diagnostic performance determined by masked reading. Q J Nucl Med Mol Imaging. 2011;55:448–57.
Liu T, Xu JY, Xu W, Bai YR, Yan WL, Yang HL. 18Fluorine deoxyglucose positron emission tomography, magnetic resonance imaging and bone scintigraphy for the diagnosis of bone metastases in patients with lung cancer: which one is the best?—a meta-analysis. Clin Oncol. 2011;23:350–8.
Beheshti M, Langsteger W, Fogelman I. Prostate cancer: role of SPECT and PET in imaging bone metastases. Semin Nucl Med. 2009;39:396–407.
Fogelman I, Cook G, Israel O, Van der Wall H. Positron emission tomography and bone metastases. Semin Nucl Med. 2005;35:135–42.
Abuzallouf S, Dayes I, Lukka H. Baseline staging of newly diagnosed prostate cancer: a summary of the literature. J Urol. 2004;171:2122–7.
Rigaud J, Tiguert R, Le Normand L, et al. Prognostic value of bone scan in patients with metastatic prostate cancer treated initially with androgen deprivation therapy. J Urol. 2002;168:1423–6.
Mankoff DA. A definition of molecular imaging. J Nucl Med. 2007;48:18N–21N.
Tryciecky EW, Gottschalk A, Ludema K. Oncologic imaging: interactions of nuclear medicine with CT and MRI using the bone scan as a model. Semin Nucl Med. 1997;27:142–51.
Gosfield 3rd E, Alavi A, Kneeland B. Comparison of radionuclide bone scans and magnetic resonance imaging in detecting spinal metastases. J Nucl Med. 1993;34:2191–8.
Horiuchi-Suzuki K, Konno A, Ueda M, et al. Skeletal affinity of Tc (V)-DMS is bone cell mediated and pH dependent. Eur J Nucl Med Mol Imaging. 2004;31:388–98.
Cook GJ, Fogelman I. The role of positron emission tomography in the management of bone metastases. Cancer. 2000;88:2927–33.
Savelli G, Chiti A, Grasselli G, Maccauro M, Rodari M, Bombardieri E. The role of bone SPET study in diagnosis of single vertebral metastases. Anticancer Res. 2000;20:1115–20.
Han L, Au-Yong T, Tong W, Chu K, Szeto L, Wong C. Comparison of bone single-photon emission tomography and planar imaging in the detection of vertebral metastases in patients with back pain. Eur J Nucl Med. 1998;25:635–8.
Reinartz P, Schaffeldt J, Sabri O, et al. Benign versus malignant osseous lesions in the lumbar vertebrae: differentiation by means of bone SPET. Eur J Nucl Med. 2000;27:721–6.
Daldrup-Link HE, Franzius C, Link TM, et al. Whole-body MR imaging for detection of bone metastases in children and young adults comparison with skeletal scintigraphy and FDG PET. Am J Roentgenol. 2001;177:229–36.
Vogler III JB, Murphy WA. Bone marrow imaging. Radiology. 1988;168:679–93.
Tombal B, Rezazadeh A, Therasse P, Van Cangh PJ, Vande Berg B, Lecouvet FE. Magnetic resonance imaging of the axial skeleton enables objective measurement of tumor response on prostate cancer bone metastases. Prostate. 2005;65:178–87.
Traill Z, Talbot D, Golding S, Gleeson FV. Magnetic resonance imaging versus radionuclide scintigraphy in screening for bone metastases. Clin Radiol. 1999;54:448–51.
Cumming J, Hacking N, Fairhurst J, Ackery D, Jenkins J. Distribution of bony metastases in prostatic carcinoma. Brit J Urol. 1990;66:411–14.
Lecouvet F, Simon M, Tombal B, Jamart J, Berg BV, Simoni P. Whole-body MRI (WB-MRI) versus axial skeleton MRI (AS-MRI) to detect and measure bone metastases in prostate cancer (PCa). Eur Radiol. 2010;20:2973–82.
Freedman GM, Negendank WG, Hudes GR, Shaer AH, Hanks GE. Preliminary results of a bone marrow magnetic resonance imaging protocol for patients with high-risk prostate cancer. Urology. 1999;54:118–23.
Schöder H, Herrmann K, Gönen M, et al. 2-[18F] fluoro-2-deoxyglucose positron emission tomography for the detection of disease in patients with prostate-specific antigen relapse after radical prostatectomy. Clin Cancer Res. 2005;11:4761–9.
Liu IJ, Zafar MB, Lai Y-H, Segall GM, Terris MK. Fluorodeoxyglucose positron emission tomography studies in diagnosis and staging of clinically organ-confined prostate cancer. Urology. 2001;57:108–11.
Oyama N, Akino H, Suzuki Y, et al. FDG PET for evaluating the change of glucose metabolism in prostate cancer after androgen ablation. Nucl Med Commun. 2001;22:963–9.
Emonds K, Swinnen J, Mortelmans L, Mottaghy F. Molecular imaging of prostate cancer. Methods. 2009;48:193–9.
Liu N, Ma L, Zhou W, et al. Bone metastasis in patients with non-small cell lung cancer: the diagnostic role of F-18 FDG PET/CT. Eur J Radiol. 2010;74:231–5.
Liu T, Cheng T, Xu W, Yan W-L, Liu J, Yang H-L. A meta-analysis of 18FDG-PET, MRI and bone scintigraphy for diagnosis of bone metastases in patients with breast cancer. Skeletal Radiol. 2011;40:523–31.
Acknowledgments
This study was supported by the National Natural Science Foundation (Grant Nos., 81271532, 81171456, and 30900378).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shen, G., Deng, H., Hu, S. et al. Comparison of choline-PET/CT, MRI, SPECT, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate cancer: a meta-analysis. Skeletal Radiol 43, 1503–1513 (2014). https://doi.org/10.1007/s00256-014-1903-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-1903-9