Abstract
Purpose
The purpose of this study was to quantify the posterior horn meniscal slope and determine its contribution to the reduction in posterior tibial slope.
Methods
Patients aged between 16 and 60 years and had intact menisci with no evidence of previous injury or surgery were included. Patients with radiological evidence of osteoarthritis Grade II–IV, any acute or chronic meniscus injuries, fractures, and ligamentous injuries were excluded. The posterior bony slope (PTS) and the meniscus slope (MS) of the posterior horns were measured at 25, 50, and 75% from the medial and lateral borders of the tibial plateau.
Results
325 MR images (mean age 37.1 ± 10.9 years) were included. There were 194 males and 131 females, with 162 left and 163 right knees. The PTS in the medial compartment ranged from (−) 2.8° to 3.7° and from (−) 1.3° to 1.9° in the lateral compartment (p = 0.0001). The MS in the medial compartment ranged from 27.4° to 28.2°, and from 27.8° to 28.7° in the lateral compartment (p > 0.05). The differences between the medial and lateral knee compartment were statistically significant. At the 25% interval the p level was 0.037, at 50% p = 0.00001, and at 75% p = 0.0001. There were no significant between gender differences.
Conclusions
The results of this study demonstrated a significant reduction in posterior tibial bone slope by the posterior horns of both the medial and lateral meniscus, from a mean of (−) 1° to 2° to a more horizontal anterior slope. The posterior bone slope was larger in the medial compartment by 1°, resulting in a smaller slope reduction in the lateral compartment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over 35 years ago, Shoemaker and Markolf reported the posterior horn of the medial meniscus is an important structure in resisting against anterior tibial translation in the anterior cruciate ligament (ACL) deficient knee [23]. Allan et al. confirmed that anterior tibial translation was significantly increased at all flexion angles in ACL deficient knees that underwent a medial meniscectomy [3]. Musahl et al. demonstrated that the lateral meniscus appears to be an important restraint to anterior tibial translation during combined valgus and rotatory loads [21].
Another anatomic factor that plays a crucial role in knee stability is the posterior tibial bone slope. Dejour and Bonnin showed that every 10° increase in posterior tibial slope was associated with a 6-mm increase in anterior tibial translation, and the radiological Lachman test increased by 3 mm for every 10° in tibial slope [7]. Several clinical studies have indicated there is a higher risk of ACL injuries in patients with a greater posterior slope [5, 13, 25, 28].
In addition to the posterior tibial bone slope, the meniscus also contributes to antero-posterior knee stability [8, 17]. Elmansori et al. showed that an increased meniscal slope is a risk factor for ACL injury [17], and Song reported that an increased medial meniscus slope increases the risk of meniscus ramp lesions in ACL deficient knees [24]. As the posterior horn of the meniscus is thicker than the anterior horn, the posterior bone slope should be counter-balanced by the menisci and reduced to neutral, or even converted to anterior, tibial slope [17, 24]. In fact, the posterior horns of the menisci could stabilize the knee against anterior tibial translation similar to a chock block next to a tyre, reducing roll by acting as a physical barrier.
MRI imaging has been successfully used to measure tibial slope and soft tissue slopes with high inter- and intra-rater reliability [11, 12, 20]. Lustig et al. have measured the soft tissue slope using MR imaging and reported that the menisci shift the tibial slope towards the horizontal [20]. Unfortunately, they have measured meniscus soft tissue slope including the anterior horns, which may not influence or reduce anterior tibial translation [1, 6, 19, 27].
Hence the purpose of this study was to quantify the posterior horn meniscal slope of both the medial and lateral meniscus using MR images and to determine their contributions to the reduction in posterior tibial bone slope. The hypothesis was that both would contribute to a reduction in the effective bony posterior tibial slope evident on plain radiographs.
Methods
This investigation was approved by the ethics committee of the University of Pretoria (South Africa ethics approval number: 668/2019—blinded for review), and complied with all the requirements set out in the National Health Act 63 of 2003. The study utilized the IMPAX (AGFA Healthcare©, Mortsel, Belgium) Picture Archiving and Communication System (PACS) database of the department of radiology at a subspecialty tertiary hospital for orthopaedic surgery. The database was searched for all knee MR images from January 2018 to May 2020. MR images were included if patients were aged between 16 and 60 years, had reached skeletal maturity, and had intact menisci with no evidence of previous injury or surgery. Knees were excluded if there was radiological evidence of osteoarthritis Grades II–IV, and if there were any acute or chronic meniscus injuries. Images with evidence of prior fractures, multi-ligament injuries, injuries to the collaterals, and injuries to the posterior cruciate ligaments or posterolateral corner were also excluded. Images with ACL injuries or evidence of previous ACL injuries were included only if they fulfilled the criteria outlined in the inclusion and exclusion parameters. For all identified MR images, the electronic medical records were cross-checked to ensure adherence to the inclusion and exclusion criteria.
Slope measurements
The annotation tools of the PACS system were utilized to carry out all measures of the bone and meniscal slope angles. These tools allow tracing of the anatomical landmarks, connecting regions of interest, and measurement of different angles. Proton density MR images were used for all measures. Slope measures for both the bony tibial posterior slope and meniscus slope were performed using previously established methods [11, 12, 20].
Bony posterior tibial slope
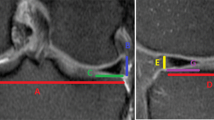
To ensure reliable and reproducible measurements, a standard protocol was applied by all observers. On a split screen the coronal, sagittal, and axial images were displayed, and the scout line and localizer mode were used to scroll through all three planes simultaneously. The annotation tools were then used to establish the centre of the tibial plateau on the axial image. The corresponding coronal image was defined as the reference image and the vertical intermediate line (yellow) defined the centre of the knee, dividing the tibial plateau into a medial and lateral half (Fig. 1). A second line (blue) was then drawn from the lateral to the medial border of the tibia, passing through the most inferior aspect of the tibial plateau. The annotation tools were then again used to establish the distance between the medial and lateral borders of the plateau. Parallel lines were drawn 25, 50, and 75% from the outer margin of the tibial plateau (Fig. 2). The corresponding sagittal images were used to measure both the bone and meniscal slopes in these three anatomic locations (Fig. 3). The proximal tibial anatomic axis (red line) was drawn by establishing two lines (blue lines), 2 and 4 cm distal to the joint line, and connecting the midpoint between these two lines (red line) (Fig. 3). The tibial plateau was marked with a line from the most anterior to the most posterior point of the tibial plateau (yellow line) (Fig. 3). The slope was measured between the tibial plateau (yellow line) and a line that was established 90° to the proximal tibial anatomic axis. If the slope was directed posteriorly it was defined as posterior or negative (−), and if the slope was directed anteriorly it was defined as anterior or positive (+).
The annotation tools of the PACS Impax were used to establish the centre of the tibial plateau. The tools allow simultaneous shifting of reference lines in all three images. The corresponding coronal image was defined as the reference image and the vertical intermediate line (yellow) defined the centre of the knee, dividing the tibial plateau into a medial and lateral half
In this step, the most medial and lateral aspects of the joint line were marked with a vertical line (blue line). A line was then drawn from the joint line (blue line) to the centre of plateau passing through the most inferior aspects of the plateau (yellow line). The annotation tool is then used to draw three parallel lines 25, 50, and 75% of the distance across the joint line (red lines)
The proximal tibial anatomic axis (PTAA) was established by drawing two lines on a sagittal image, 2 cm apart, from anterior to posterior (blue lines). The midpoint between these two lines was connected, resulting in a vertical line (red line) that is defined as the PTAA. The tibial plateau was defined by a line drawn from the most anterior to the most posterior point on a sagittal image (yellow line). An additional perpendicular line (green line) to the PTAA was drawn from the point where the tibial plateau line meets the PTAA. The angle between this line (green) and the tibial plateau line (yellow) has been defined as the posterior tibial slope. The slope was defined as posterior (−) if the plateau line is inferior to the perpendicular line, and anterior (+) if the plateau line is proximal to the perpendicular line
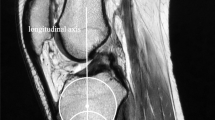
Meniscus slope
To establish the meniscus slope of the posterior horn, a line was drawn across the superior surface of the meniscus between the most posterior and the most proximal point of the meniscus, tangent to its superior surface (red line) (Fig. 4). The angle between the meniscus line and tibial plateau was then defined as the slope of the posterior horn of the meniscus (Fig. 4). The combined resultant slope was calculated by adding the meniscal slope to the bone slope. Similar to the bone slope, a posteriorly directed slope was defined as posterior or negative (−), and anterior or positive (+) if the slope was directed anteriorly.
Statistical analysis
Descriptive statistics were applied to all measures. Mean bone and meniscal slope angles, standard deviation, range, and 95% confidence intervals were calculated. Normality of the data distribution was assessed using the Shapiro–Wilks test, and homogeneity of variance was verified with Levene’s test. A series of paired student t tests were used to compare the medial to the lateral knee compartment measures. Intra- and inter-rater reliability (ICC) for all drawings and angles were established by repeating the measures in ten randomly selected MR images. Three independent research associates drew all predefined lines and measured all angles on two consecutive days. The images were presented in random order to reduce recognition. The algorithm of Landis and Koch was used to assess the rate of agreement [16]. Values above 0.80 represented excellent agreement, values between 0.62 and 0.79 were considered good agreement, values between 0.41 and 0.61 indicated moderate agreement, and values below 0.4 suggested fair to poor agreement [16]. All analyses were conducted using STATA SE (Version 12.0; StataCorp, College Station, Texas, USA) for Windows.
Results
A total of 831 MR images were performed from January 2018 to May 2020. Of those, 329 images had signs of meniscus injuries and were excluded. There were 93 images performed in patients less than 16 years, 42 images exhibited significant chondral and degenerative changes, 23 images confirmed multi-ligament injuries, and 19 images were performed in patients over 60 years. Therefore, a total of 506 images were excluded, and the remaining number of included MR images were 325. The mean age was 37.1 ± 10.9 years (range 16–60). There were 194 males and 131 females, and 162 left and 163 right knees.
Intra- and inter-rater reliability (ICC) between the three raters for vertical intermediate line and 25, 50, and 75% lines ranged from 0.95 to 0.98 for inter-rater reliability and 0.94–0.99 for intra-rater reliability. Intra- and inter-rater reliability (ICC) between the three raters for proximal tibial anatomic axis and tibial plateau slope lines ranged from 0.89 to 0.93 for inter-rater reliability and 0.92 to 0.96 for intra-rater reliability. Intra- and inter-rater reliability (ICC) between the three raters for the bone slope and slope of the posterior horn of the menisci ranged from 0.91 to 0.94 for inter-rater reliability and 0.94 to 0.97 for intra-rater reliability. Given the consistent higher ICC for intra-rater reliability, all measures utilized were those performed by the first author [EH] only.
Posterior tibial bone slope
The results for the posterior tibial bone slope in both the medial and lateral compartment are summarized in Table 1. The mean slope was significantly higher in the medial compartment at the 25% (p = 0.0001), 50% (p = 0.0001), and 75% (p = 0.0001) distance from the medial border of the tibial plateau. The 95% confidence intervals did not overlap, further strengthening statistical significance. However, the mean differences for all angles ranged from 1.1° to 1.8°, and these differences are possibly not clinically relevant. There were no significant between gender differences for the posterior tibial bone slope (Tables 2 and 3).
Meniscus slope
The results for the slope of the posterior meniscal horns in both the medial and lateral compartment are summarized in Table 1. The slope ranged between 27° and 29°, and these differences were not statistically significant. There were no significant between gender differences for the meniscus slope (Tables 2 and 3).
Resultant combined posterior tibial slope
The results for the resultant combined slope for both the medial and lateral compartment are summarized in Table 1. The combined slope decreased the tibial posterior bone slope from (−) 1° to 2° to a combined positive anterior slope ranging from 23° to 27°. The differences between the medial and lateral knee compartment were statistically significant. At the 25% distance the p-value was 0.037, at the 50% distance p = 0.00001, and at the 75% distance p = 0.0001. This was most likely related to the higher posterior bone slope in the medial compartment and very similar meniscal slopes in both compartments, resulting in less overall slope reduction in the lateral knee compartment. There were no significant between-gender differences for the resultant combined posterior tibial slope (Tables 2 and 3).
Discussion
This study demonstrated that the posterior horns of both the medial and lateral menisci significantly reduced the posterior tibial bone slope from an average of (−) 1°–2° to a positive value of (+) 23°–27°. Although the posterior bone slope was larger in the medial compartment, the posterior horn meniscus slopes were very similar in both knee compartments, resulting in a smaller slope reduction by 1°–2° in the lateral knee compartment.
These findings are consistent with earlier studies. Alici et al. showed a mean bone slope of 3.2°–3.6° in the medial compartment compared to 2.7°–2.9° in the lateral compartment [2]. However, Stijak et al. reported larger posterior slopes in the lateral knee compartment by a mean of 2° [25]. Interestingly, there were no significant between-gender differences for both posterior tibial slope and meniscus slope, consistent with the findings reported by Han et al. [10]. They analysed anthropometric differences of the knee on MRI, and did not find any variation in posterior tibial slope between gender and age [10]. In contrast, Koh et al. identified significant between-gender differences for posterior tibial slope in osteoarthritic patients [15]. Obviously, gender differences could reflect the population groups investigated, and any anthropometric measures should take these factors into consideration when reporting on anatomic morphology.
In a finite element model, Bendjaballah et al. demonstrated medial meniscectomy caused increased coupled tibial external rotation, increased forces on the lateral tibial plateau, and resulted in larger compressive joint forces [4]. In their in silico model, the menisci had no direct effect on knee stability [4]. However, these findings using finite element analysis were not confirmed by later clinical studies. Hollis et al. reported an increase in strain in both the medial and lateral posterior horn of the meniscus from 1.2 to 1.7% when the ACL was severed, with a return to intact strains after ACL reconstruction [14]. It could be argued that an increase in strain of 50% is clinically relevant, but most likely the relevance for non-solid viscous biological tissues can be questioned.
Watanabe et al. investigated anterior tibial translation following resection of one-third, two-thirds, and the entire posterior horn of the medial meniscus [27]. Anterior tibial translation increased by 0.1 mm with one-third resection, 0.5 mm with two-thirds resection, and 1.1 mm with total meniscectomy. They suggested resection of the posterior horn of the medial meniscus by two-thirds or more will significantly change the kinematics of the knee, resulting in increased anterior tibial translation by removing the posterior buttress [27]. However, again the clinical relevance of their findings must be questioned. Chen et al. studied the effect of posterior horn medial meniscus tears on knee stability and reported the posterior horn was important in controlling external rotation but had no effect on anterior tibial translation [6]. In contrast, Lorbach et al. noted that an additional meniscus tear in ACL deficient knees caused a significant increase in anterior tibial translation by 17%, which returned to the previous values with meniscal suturing. [19] However, this study can be criticized for their conclusions as the standard deviations overlapped for all scenarios, and both the internal and external validity of their results are uncertain. Ahn et al. found that medial meniscus posterior horn longitudinal tears resulted in a significant increase in antero-posterior tibial translation at all flexion angles and that meniscal repair improved tibial translation [1]. It appears that the current evidence with regard to the medial meniscus as a secondary stabilizer is inconclusive, and largely based on indirect clues. However, current published data support the concept that the posterior horn of the medial meniscus does contribute to anterior stability in the ACL deficient knee.
The role of the lateral meniscus in providing anterior–posterior knee stability is not clear. The lateral meniscus apparently has no significant posterior wedge effect, and less robust capsular attachments allow more movement under load [21]. Levy et al. reported in a cadaver model that, in contrast to medial meniscectomy, anterior and posterior translations after lateral meniscectomy were not affected in the ACL deficient knee [18]. Musahl et al. revealed lateral meniscectomy resulted in a significant increase in anterior tibial translation during a pivot shift manoeuvre, but not during a simulated Lachman test [21]. They concluded that the lateral meniscus added significant restraint to anterior translation during combined valgus and rotatory loads [21]. Shybut et al. confirmed these results and found that in ACL deficient knees the pivot shift manoeuvre was significantly increased but the Lachman manoeuvre had no effect on anterior tibial translation [22]. Similarly, Tang et al. reported that a lateral meniscal posterior root tear increased knee laxity and that repair restored knee stability under anterior tibial load while normalizing the pivot shift [26]. Forkel et al. showed that transection of the lateral meniscus posterior root decreased knee stability similar to an ACL deficient knee, whereas repair reduced anterior tibial translation close to the native state. [9]. Zaffagnini et al. performed allograft meniscus transplantation and noted a 25% decrease in antero-posterior laxity and a 50% decrease in internal rotation with both medial and lateral meniscus transplantations [29]. The posterior horn of the lateral meniscus also probably plays a role in augmenting knee stability but, similar to the medial meniscus, the current evidence is controversial, and based on indirect clues rather than appropriately designed biomechanical and clinical studies.
Despite the lack of evidence, it seems that both lateral and medial menisci contribute to knee stability. One could argue that meniscus preservation is critical for knee stability in ACL-intact individuals, but especially in patients with ACL-deficient knees. There is clearly sound motivation to design and execute the appropriate studies to investigate this further.
Limitations
This study has some important limitations. The height and weight of the included subjects were not measured, and there might be a correlation between with the posterior slope and these demographic variables. The MR images were performed in the supine position with all knees in slight flexion, and weight bearing may have a flattening effect on the meniscus and intra-articular soft tissues. The images were obtained mainly in European and Arabic patients and morphometric differences between other population groups such as African–American and Asian subjects may exist, potentially limiting the generalizability of the findings.
Conclusions
The results of study demonstrated a significant reduction in posterior tibial bone slope by the posterior horns of both the medial and lateral meniscus from a mean of (−) 1° to 2° to a more horizontal anterior slope. The posterior bone slope was larger in the medial compartment by 1° resulting in a smaller slope reduction in the lateral knee compartment. These findings support the current theory that both posterior meniscal horns could act as chock blocks reducing anterior tibial translation.
References
Ahn JH, Bae TS, Kang KS et al (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 39:2187–2193. https://doi.org/10.1177/0363546511416597
Alici T, Esenyl CZ, Esenyl M (2011) Relationship between meniscal tears and tibial slope on the tibial plateau. Eurasian J Med 43:146–151. https://doi.org/10.5152/eajm.2011.35
Allen CR, Wong EK, Sakane M et al (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18:109–115. https://doi.org/10.1002/jor.1100180116
Bendjaballah MZ, Shirazi-Adl A, Zukor DJ (1998) Biomechanical response of the passive human knee joint under anterior-posterior forces. Clin Biomech (Bristol, Avon) 13:625–633. https://doi.org/10.1016/s0268-0033(98)00035-7
Beynnon BD, Slauterbeck JR, Schutt RC Jr, Mansouri H, Dabezies E (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Am 90:2724–2734. https://doi.org/10.2106/JBJS.G.01358
Chen L, Linde-Rosen M, Hwang SC et al (2015) The effect of medial meniscal horn injury on knee stability. Knee Surg Sports Traumatol Arthrosc 23:126–131. https://doi.org/10.1007/s00167-014-3241-9
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76:745–749
Elmansori A, Lording T, Dumas R et al (2017) Proximal tibial bone and meniscal slopes are higher in ACL injured subjects than controls: a comparative MRI study. Knee Surg Sports Traumatol Arthrosc 25:1598–1605. https://doi.org/10.1007/s00167-017-4447-4
Forkel P, von Deimling C, Lacheta L et al (2018) Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 26:2302–2309. https://doi.org/10.1007/s00167-018-4949-8
Han H, Oh S, Chang CB, Kang SB (2016) Anthropometric difference of the knee on MRI according to gender and age groups. Surg Radiol Anat 38:203–211. https://doi.org/10.1007/s00276-015-1536-2
Hashemi J, Chandrasekar N, Gill B et al (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Am 90:2724–2734. https://doi.org/10.2106/JBJS.G.01358
Hashemi J, Chandrasekar N, Mansouri H et al (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38:54–62. https://doi.org/10.1177/0363546509349055
Hohmann E, Bryant A, Reaburn P et al (2011) Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc 19:S109-114. https://doi.org/10.1007/s00167-011-1547-4
Hollis JM, Pearsall AW 4th, Niciforos PG (2000) Change in meniscal strain with anterior cruciate ligament injury and after reconstruction. Am J Sports Med 28:700–704. https://doi.org/10.1177/03635465000280051401
Koh YG, Nam JH, Chung HS, Chun HJ, Kim HJ, Kang KT (2020) Morphometric study of gender difference in osteoarthritis posterior tibial slope using three-dimensional magnetic resonance imaging. Surg Radiol Anat 42:667–672. https://doi.org/10.1007/s00276-020-02429-3 (Epub 2020 Feb 21)
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Lee YS, Kim JG, Lim HC et al (2009) The relationship between tibial slope and meniscal insertion. Knee Surg Sports Traumatol Arthrosc 17:1416–1420. https://doi.org/10.1007/s00167-009-0847-4
Levy M, Torzilli PA, Gould JD et al (1989) The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 71:401–406
Lorbach O, Kieb M, Herbort M et al (2015) The influence of medial meniscus in different conditions on anterior tibial translation in the anterior cruciate deficient knee. Int Orthop 39:681–687. https://doi.org/10.1007/s00264-014-2581-x
Lustig S, Scholes CJ, Leo SPM, Cooligan M, Parker DA (2013) Influence of soft tissues on the proximal bony tibial slope with two-dimensional MRI. Knee Surg Sports Traumatol Arthrosc 21:372–379. https://doi.org/10.1007/s00167-012-1990-x
Musahl V, Citak M, O’Laughlin PF et al (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597. https://doi.org/10.1177/0363546510364402
Shybut TB, Vega CE, Haddad J et al (2015) Effect of lateral meniscus root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 43:905–911. https://doi.org/10.1177/0363546514563910
Shoemaker SC, Markolf KL (1986) The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. J Bone Joint Surg Am 68:71–79
Song GY, Liu X, Zhang H et al (2016) Increased medial meniscal slope is associated with greater risk of ramp lesions in noncontact anterior cruciate ligament injury. Am J Sports Med 44:2039–2046. https://doi.org/10.1177/0363546516640516
Stijak L, Herzog RF, Schai P (2008) Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc 16:112–117. https://doi.org/10.1007/s00167-007-0438-1
Tang X, Marshall B, Wang JH et al (2019) Lateral meniscal posterior root repair with anterior cruciate ligament reconstruction better restores knee stability. Am J Sports Med 47:59–65. https://doi.org/10.1177/0363546518808004
Watanabe Y, Van Scyoc A, Tsuda E et al (2004) Biomechanical function of the posterior horn of the medial meniscus: a human cadaveric study. J Orthop Sci 9:280–284. https://doi.org/10.1007/s00776-004-0781-8
Webb JM, Salmon LJ, Leclerc E et al (2013) Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed knee. Am J Sports Med 41:2800–2804. https://doi.org/10.1177/0363546513503288
Zaffagnini S, Di Paolo S, Stefanelli F et al (2019) The biomechanical role of meniscal allograft and preliminary in-vivo kinematic evaluation. J Exper Orthop 6:27. https://doi.org/10.1186/s40634-019-0196-2
Author information
Authors and Affiliations
Contributions
EH: conceptualisation, protocol, design interpretation, writing, final approval of manuscript; MN: conceptualisation, protocol, final approval of manuscript; KT: conceptualisation, protocol, writing, final approval of manuscript; VG: conceptualisation, protocol, writing, final approval of manuscript; NK: conceptualisation, protocol, design interpretation, writing, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hohmann, E., Tetsworth, K., Glatt, V. et al. The posterior horn of the medial and lateral meniscus both reduce the effective posterior tibial slope: a radiographic MRI study. Surg Radiol Anat 43, 1123–1130 (2021). https://doi.org/10.1007/s00276-021-02696-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-021-02696-8