Abstract
Objective
To present the ultrasound appearance of stress fractures (SF) of the ankle malleoli.
Material and Methods
We present a retrospective review of 6 patients (4 women and 2 men, with an age range of 24–52 years, mean age of 39 years) in which ultrasound diagnosed, together with the clinical findings, an SF of the ankle malleoli. For all of these patients ultrasound was the first imaging technique applied because of a clinical suspicion of soft tissue injuries following excessive exertion. Patients were subsequently examined using standard radiographs and/or MRI.
Results
At ultrasound patients showed thickening of the periosteum in all patients, calcified bone callus was evident in 3 out of 6 patients. Cortical irregularities and subcutaneous oedema were found in all but one patient. Colour Doppler showed local hypervascular changes in all patients. Local compression with the transducers during real-time scanning increased pain in all cases.
Conclusion
Ultrasound, together with the clinical findings, can diagnose an SF of the ankle malleoli. We suggest that sonologists should include malleolar SF in their differential diagnosis, particularly in the case of perimalleolar pain from over-solicitation. They must also include, as part of every ultrasound examination of the ankle, the evaluation of both malleoli and should be aware of the ultrasound appearance of malleolar SF. If the diagnosis remains uncertain, an MRI should be prescribed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress fractures (SF) are a consequence of excessive repeated loading applied to a normal bone and are common in both recreational and elite athletes. The diagnosis is frequently suspected on the basis of clinical findings, but an imaging study is necessary to confirm the diagnosis and to rule out other sources of pain. Standard radiographs are often negative initially when the radio-opaque callus is not visible. Computed tomography (CT) is useful in selected situations such as longitudinal fractures of the tibia. Bone scintigraphy is very sensitive, but not specific. Magnetic resonance imaging (MRI) is the imaging gold standard for the early detection of SF, but it is poorly accessible and expensive [1].
Ultrasound is now accepted as a first-line modality in the assessment of injuries affecting muscles, tendons, joints and nerves of the extremities [2–5]. We present a retrospective review of six cases in which ultrasound, together with the clinical findings, diagnosed an SF of the ankle malleoli. For all of these cases ultrasound was the first imaging technique applied because of a clinical suspicion of soft-tissue injury. Standard radiographs and/or MRI confirmed the diagnosis in 5out of 6 patients.
Materials and methods
In the last 6 months, we identified two subjects in whom ultrasound detected an SF of one of the two malleoli in routine practice. The two cases induced us to conduct a retrospective analysis of the teaching files (over the last 6 years) of the same institution (CIM SA), which identified four further cases. The clinical and ultrasound data of the six patients are summarised in Table 1.
We identified 2 men and 4 women (age range 24–52 years, mean age 39 years) who had an ultrasound examination of the ankle to assess peri-articular soft tissue because of persistent mechanical ankle pain following excessive exertion. An ultrasound examination was performed in 5 out of 6 patients to rule out tendinitis. In 1 patient there were no details concerning clinical suspicion at the time of ultrasound examination. All but one patient had a history of mechanical pain either at the medial (2) or lateral (4) ankle malleolus. Three patients were referred by orthopaedic surgeons, 2 by rheumatologists, and 1 by a general practitioner. None of the patients were evaluated by other imaging techniques before ultrasound examination. In none of the cases was there a clinical suspicion of SF.
The ultrasound examinations were all performed by a musculoskeletal radiologist who had 29 years of experience in the field (SB). Commercially available ultrasound equipment (iU22; Philips Medical Systems, Bothell, WA, USA) with 17-5- or 12-5-MHz electronic linear transducers was used. After adequate optimisation of equipment parameters for assessment of the ankle, the joint and para-articular tissues were assessed using a standard technique. We used a generous amount of coupling gel. No stand-off pad was used. The patient lay on the examination table in dorsal decubitus with the knee slightly flexed. The painful ankle was examined in internal and external rotation and on axial, sagittal and coronal planes. All compartments of the ankle were systematically studied. Colour Doppler was performed in all patients. After discovering the irregularity of the damaged malleolus, we obtained additional images to evaluate in more detail the periosteum, surface of the bone cortex, and the adjacent soft tissues. The ultrasound images and videos of all patients were reviewed using our PACS system. In grey-scale examinations we assessed and measured (in millimetres) the presence of thickening of the periosteum, the presence of calcified bone callus, cortical irregularities and subcutaneous oedema. Semiquantitative assessment of periosteal hypervascularisation (minimal, moderate, severe) and hypervascular changes of subcutaneous soft tissues and bone (present/absent) were evaluated in colour Doppler images and videos.
In 5 of the 6 patients (patients 1–4, 6) the diagnosis was confirmed by an additional imaging modality (MRI and radiographs in 2 patients (patients 2 and 4), MRI in 2 patients (patients 1 and 6), radiographs in 1 patient (patient 3)). One patient had no additional imaging studies (patient 5). MRI was obtained within 10 days of the ultrasound examination with a 1.5-T scanner using an ankle standardised protocol including sagittal PD and STIR images, axial oblique fat-saturated proton density-weighted images, coronal T1 and fat-saturated T2-weighted images. Standard radiographs were obtained using a routine technique including anteroposterior, profile and internal oblique view of the malleolus involved.
All patients were treated conservatively with rest and medical treatment. All but one of the patients were contacted by phone and had a good outcome with no significant ankle pain and functional limitation. One patient was lost to follow-up (patient 5).
Results
The retrospective analysis of our 6 patients is summarised in Table 1. The SF affected the lateral malleolus in 4 patients (patients 2, 3, 5 and 6) and the medial malleolus in 2 patients (patients 1 and 4). The left ankle was affected in 4 patients; the right ankle in 2 patients.
At ultrasound, thickening of the periosteum ranged from 1 to 2 mm (mean 1.5 mm; Fig. 1). Calcified bone callus was evident in 3 out of 6 patients (Fig. 2). Cortical irregularities were found in all but one patient. Subcutaneous oedema was found in all but one patient. Colour Doppler showed local hypervascular changes in all patients. The changes were minimal in 1 patient, moderate in 3 patients and severe in 2 patients (Fig. 3). The soft tissues showed increased vascularisation in 4 out of 6 patients while increased flow signal inside the bone was noted in 2 out of 6 patients. Local compression with the transducers during real-time scanning increased pain in all cases. Ultrasound evaluation in this series of patients revealed no other pathological changes. The perimalleolar tendons were normal with no evidence of tenosynovitis or tears in any of the patients. The talocrural joint did not show any signs of synovitis.
a Grey-scale and b colour Doppler coronal ultrasound, c T1-weighted and d STIR images. MRI coronal images of patient 1 were obtained over the medial malleolus. Ultrasound shows the thickening (arrowheads) and hypervascular changes (black curved arrow) of the tibial periosteum. Note the presence of some intraosseous vessels (white curved arrow). MRI shows the hypointense trabecular line (black arrow) corresponding to the fracture line, the surrounding bone marrow oedema (asterisk) as well as the thickened and inflamed periosteum (white arrowhead)
a Grey-scale and b colour Doppler coronal ultrasound, c standard radiograph and d STIR MRI sagittal image of patient 2 obtained over the lateral malleolus. Ultrasound shows the thickening (arrowheads) and hypervascular changes (black curved arrow) of the peroneal periosteum. Note the presence of a calcified callus (white arrow). Standard radiograph confirms a small periosteal calcification (white arrow). MRI shows a thin hypointense trabecular line (black arrow) surrounded by bone marrow oedema and inflammation of local periosteum and adjacent soft tissues (white arrowheads)
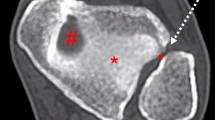
a Colour Doppler axial ultrasound, b corresponding T1-weighted fat-saturated post-gadolinium MRI axial image (image was turned anticlockwise to match the ultrasound) and c proton density-weighted MRI coronal image of patient 4 obtained over the medial malleolus. Ultrasound shows massive hypervascular changes of the periosteum (black curved arrows), intraosseous vessels (white curved arrow) and adjacent soft tissues. Note the presence of a focal interruption of the cortex (white arrow). Native and post-injected MRI images correlate well with the ultrasound appearance. Note the hypointense trabecular fracture line (black arrow), enhancement of bone marrow oedema (asterisks), local periosteum and adjacent soft tissues. The focal cortical interruption is also evident (white arrow). Clear arrow posterior tibialis tendon
Radiographs (in patients 2, 3 and 4) showed a small periosteal calcification in 2 patients (patients 2 and 4), while in the third patient they showed evidence of an SF with local bone sclerosis and a huge periosteal reaction (patient 3). MRI obtained in 4 patients (patients 1, 2, 4, 6) confirmed the diagnosis by showing a hypointense line surrounded by an area of bone marrow oedema, as well as subcutaneous soft tissue oedema in 3 patients (Figs. 1–3). In 1 patient (patient 6) the hypointense line was not detected. MRI showed no other pathological findings.
We report a paradigmatic case (patient 1).
Patient 1
A 39-year-old-nurse presented with progressive pain and swelling of the medial malleolus region for about 30 days following an increase in her running programme (5–7 km three times a week). She consulted an ankle and foot surgeon who asked for an ultrasound examination to rule out tenosynovitis of the tibialis posterior tendon. She denied any local trauma or any systemic symptoms such as fever, weight loss or anorexia. There was neither a history of previous sport injury of the lower extremities nor a history of diabetes mellitus, osteoporosis or high blood pressure. The pain was local, exacerbated while she was standing or walking, and limited her activities. Physical examination revealed localised oedema that was painful on palpation of the medial malleolus region. There was no sign of tenderness of the lateral malleolus or the calcaneus. The neurological and vascular examinations were normal.
There were no standard radiographs or other imaging studies of her ankle available. Ultrasound was performed using the standard protocol described above. Ultrasound showed reduced echogenicity with fluid distension of the lymphatics of the subcutaneous soft tissues superficial to the medial malleolus. The periosteum of the medial malleolus was thickened (1.3 mm), irregular and hypoechoic (Fig. 1). Local palpation with the transducer reproduced the patient’s symptoms. Colour Doppler showed marked hyperaemia of the periosteum with only minimal hypervascular changes inside the bone or in the adjacent subcutaneous tissues. There was no sign of tendinopathy or tenosynovitis of the ankle tendons, including the tibialis posterior tendon. Dynamic ultrasound examination was normal. The ankle joint and the subtalar joints were normal. The medial retromalleolar neurovascular bundle was normal. MRI showed a hypointense line located in the trabecular bone of the medial aspect of the distal tibia corresponding to an SF. The fracture appeared to be surrounded by an area of hyperintense bone marrow oedema on the T2-weighted fat-saturated images. Hyperintensity of the periosteum and of the adjacent swollen soft tissues was also evident on the T2-weighted fat-saturated images owing to local inflammation. No cortical bone discontinuity was seen. There was no fluid collection in the soft tissues. The peri-articular tendons were normal.
The patient was treated with rest and NSAIDs with a good outcome. She was free of symptoms at follow-up after 3 months.
Discussion
The exact physiopathology of SF is not yet known. When a bone experiences recurring loads that exceed the threshold of elastic deformity, plastic deformities occur and they are followed by microfractures [6, 7]. The accumulation of microfractures may cause clinical symptoms and, if the causative stress continues, a complete fracture may follow. SF are responsible for as many as 10 % of all sports-related pathological condition, especially in runners [8]. Even though they can affect the whole body, SF usually involve the lower extremities, which are more exposed to repetitive loading charges [1, 9]. The most common site is the tibia followed by the tarsals, metatarsals, femur, fibula, pelvis, plantar sesamoids and the spine. [8]
Patients with SF generally present local mechanical pain. Physical examination usually shows swollen surrounding soft tissues and pain on local bone palpation. Often, the patient reports a recent history of changes in training habits [8]. The diagnosis relies on clinical findings and imaging studies, and early detection of the fracture allows proper treatment, thus lowering morbidity and the risks of complications [1, 10]. For malleolar SF, conservative treatments usually have very good outcomes. They consist of stopping the sporting activity associated with the fracture and using a technical aid such as crutches for 3 to 8 weeks, depending on the clinical course and the patient’s characteristics [11]. Resuming the causative physical activity must be done progressively in the absence of pain and radiographic abnormalities (except for the presence of a bone callus). The patient’s training habits should also be evaluated and changed if necessary to prevent recurrence of SF. If an insufficiency fracture is suspected, complementary studies should be performed according to clinical suspicion [7].
To confirm the SF and to eliminate the differential diagnoses, imaging studies must be carried out. Standard radiographs are often negative, initially with a sensitivity that may be as low as 15 %. Even at follow-up, periosteal reactions with a hairline crack and/or callous formation are detectable in only about half of the cases [12]. Computed tomography (CT) is useful in some situations, such as longitudinal fractures of the tibia, but otherwise has a very low sensitivity (88 % vs 42 %) compared with MRI [13]. Bone scintigraphy is very sensitive, showing an increase in bone uptake as early as 24 h after the fracture [8]. However, its specificity is very low [14]. MRI is the imaging gold standard for the early detection of SF, but remains poorly accessible and expensive [15].
Many studies have evaluated the ability of ultrasound to detect acute fractures that are difficult to detect by X-ray, such as fatigue fractures and insufficiency fractures [16–24]. A recent study even showed that ultrasound had a good sensitivity (83 %) and specificity (76 %) compared with MRI in the early diagnosis of metatarsal bone SF. It has also been shown that ultrasound is more sensitive than standard radiographs for detecting metatarsal SF [25]. Normal cortical bone appears on ultrasound as a regular, highly hyperechoic line with strong posterior acoustic shadowing and some reverberation artefact [26]. The periosteum cannot be detected in normal adults; however, it may appear as a thin hypoechoic line adjacent to the bone cortex in children. Under normal conditions, ultrasound is unable to examine structures under the cortical bone.
In our small series, 5 patients were referred for suspected tendinopathy. None of them had any tendon lesions or any other pathology of the adjacent structures (except for SF). Thus, in our series ultrasound allowed a change in the diagnosis and treatment in all patients. SF appeared on ultrasound as subcutaneous oedema, thickening of the periosteum, cortical bone irregularities or even discontinuity, and local hyperaemia was demonstrated by colour Doppler and sometimes the presence of a local calcified bone callus formation. These characteristics resemble those described by previous studies of metatarsal SF [25, 27]. Furthermore, local compression with the transducer reproduced the patient’s symptoms. A high degree of correlation between clinical findings and ultrasound data is necessary to diagnose an SF because ultrasound findings are not specific and, if taken out of the clinical context, can represent osteomyelitis or even bone neoplasia.
As in the investigation of metatarsal SF by Banal et al. [25], we propose that plain radiography should be the first imaging study when a malleolar SF is suspected, as it is very accessible, inexpensive and can eliminate other diagnoses. If it does not confirm the SF, ultrasound should be the second imaging study, as it is inexpensive, accessible, comfortable for the patient and can allow a dynamic examination. Ultrasound may be, as for metatarsal fractures, more sensitive than plain radiographs for detecting malleolar SF. However, further studies, ideally prospective, that include a greater number of patients should be carried out to demonstrate its superior sensitivity. MRI should be the next imaging modality if the diagnosis remains doubtful or in the case of high-level trained athletes. If the clinical evolution is favourable, no other imaging studies should be performed. However, if not favourable, follow-up imaging studies, usually an MRI, should be carried out to evaluate the evolution of the SF and to eliminate other diagnoses.
It should be noted that the majority of our cases were referred, not for an SF, but for suspected perimalleolar tendinopathy, which was not confirmed. Sonologists should include malleolar SF in their differential diagnosis, particularly in the case of perimalleolar pain from over-solicitation. They must also include, as part of every ultrasound examination of the ankle, the examination of both malleoli and should be aware of the ultrasound appearance of malleolar SF. If the diagnosis remains uncertain, an MRI should be prescribed.
References
Moran DS, Evans RK, Hadad E. Imaging of lower extremity stress fracture injuries. Sports Med. 2008;38:345–56.
Bianchi S, Martinoli C, Bianchi-Zamorani M, Valle M. Ultrasound of the joints. Eur Radiol. 2002;12:56–61.
Martinoli C, Bianchi S, Dahmane M, Pugliese F, Bianchi-Zamorani MP, Valle M. Ultrasound of tendons and nerves. Eur Radiol. 2002;12:44–55.
Peetrons P. Ultrasound of muscles. Eur Radiol. 2002;12:35–43.
Campbell SE, Adler R, Sofka CM. Ultrasound of muscle abnormalities. Ultrasound Q. 2005;21:87–94. quiz 150, 3-4.
Bousson V, Wybier M, Petrover D, et al. Les fractures de contrainte. J Radiol. 2011;92:188–207.
Royer M, Thomas T, Cesini J, Legrand E. Stress fractures in 2011: practical approach. Joint Bone Spine. 2012;79 Suppl 2:S86–90.
Matheson GO, Clement DB, Mckenzie DC, Taunton JE, Lloyd-Smith DR, Macintyre JG. Stress fractures in athletes. Am J Sports Med. 1987;15:46–58.
Miller TL, Kaeding CC. Upper-extremity stress fractures: distribution and causative activities in 70 patients. Orthopedics. 2012;35:789–93.
Pegrum J, Crisp T, Padhiar N. Diagnosis and management of bone stress injuries of the lower limb in athletes. BMJ. 2012;344:e2511.
Sherbondy PS, Sebastianelli WJ. Stress fractures of the medial malleolus and distal fibula. Clin Sports Med. 2006;25:129–37. x.
Anderson MW, Greenspan A. Stress fractures. Radiology. 1996;199:1–12.
Gaeta M, Minutoli F, Scribano E, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235:553–61.
Prather JL, Nusynowitz ML, Snowdy HA, Hughes AD, McCartney WH, Bagg RJ. Scintigraphic findings in stress fractures. J Bone Joint Surg Am 1977;59:869–74.
Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16:291–306.
Khy V, Wyssa B, Bianchi S. Bilateral stress fracture of the tibia diagnosed by ultrasound. A case report. J Ultrasound. 2012;15:130–4.
Botchu R, Lee KJ, Bianchi S. Radiographically undetected coracoid fractures diagnosed by sonography. Report of seven cases. Skeletal Radiol. 2012;41:693–8.
Arni D, Lambert V, Delmi M, Bianchi S. Insufficiency fracture of the calcaneum: sonographic findings. J Clin Ultrasound. 2009;37:424–7.
Celi J, de Gautard G, Della Santa JD, Bianchi S. Sonographic diagnosis of a radiographically undiagnosed hook of the hamate fracture. J Ultrasound Med. 2008;27:1235–9.
Fusetti C, Poletti PA, Pradel PH, et al. Diagnosis of occult scaphoid fracture with high-spatial-resolution sonography: a prospective blind study. J Trauma. 2005;59:677–81.
Copercini M, Bonvin F, Martinoli C, Bianchi S. Sonographic diagnosis of talar lateral process fracture. J Ultrasound Med. 2003;22:635–40.
Boutry N, Vanderhofstadt A, Peetrons P. Ultrasonography of anterosuperior calcaneal process fracture: report of 2 cases. J Ultrasound Med. 2006;25:381–5.
Bodner G, Stockl B, Fierlinger A, Schocke M, Bernathova M. Sonographic findings in stress fractures of the lower limb: preliminary findings. Eur Radiol. 2005;15:356–9.
Caruso G, Lagalla R, Derchi L, Iovane A, Sanfilippo A. Monitoring of fracture calluses with color Doppler sonography. J Clin Ultrasound. 2000;28:20–7.
Banal F, Gandjbakhch F, Foltz V, et al. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fractures: a pilot study of 37 patients. J Rheumatol. 2009;36:1715–9.
Erickson SJ. High-resolution imaging of the musculoskeletal system. Radiology. 1997;205:593–618.
Banal F, Etchepare F, Rouhier B, et al. Ultrasound ability in early diagnosis of stress fracture of metatarsal bone. Ann Rheum Dis. 2006;65:977–8.
Conflict of interest
The authors declare that they have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bianchi, S., Luong, D.H. Stress fractures of the ankle malleoli diagnosed by ultrasound: a report of 6 cases. Skeletal Radiol 43, 813–818 (2014). https://doi.org/10.1007/s00256-014-1861-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-1861-2