Abstract
Purpose
Our objective was to evaluate the syndesmotic and fracture instability using conventional ankle computed tomography (CT) with stress maneuvers.
Methods
A consecutive sample of 123 individuals with an ankle sprain was assessed for eligibility. In total, 33 patients met the inclusion criteria. All patients underwent a magnetic resonance imaging (MRI) and CT scan with stress maneuvers (CTSM). The patterns of ligament tears f were classified using West Point grades I, IIA, IIB, III. Mann–Whitney test was used to test the differences in the numerical variables between injured and uninjured syndesmoses. The Spearman correlation tested the strength of the association between the tibial joint surface involved in posterior malleolus fracture and syndesmotic instability.
Results
In MRI, two patterns of syndesmotic ligament injury predominated. A completely torn anterior inferior tibiofibular (AITFL) and interosseous tibiofibular ligaments (ITFL) and a completely torn AITFL were combined with a partially torn ITFL. In the neutral phase CTSM and during the stress phase the median difference of the narrowest tibiofibular distance between injured and uninjured syndesmoses was 0.2 mm (P = 0.057) and 2.3 mm (P < 0.0001), respectively. There was no association between the percentage of involvement of the posterior tibial joint surface in the posterior malleolar fracture and syndesmotic instability as measured with CTSM.
Conclusion
The conventional computed tomography with external rotation and dorsiflexion represents a reproducible and accurate diagnostic option for detecting syndesmosis instability and fracture instability in acute isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II.
Level of Evidence: Prospective study among consecutive patients (Diagnosis); Level of evidence, 2.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A ligament-centered analysis is currently incorporated into the assessment of fracture stability and treatment decision making. The tibiotalar joint represents an intrinsically stable joint formed by three bones, with the talus lying inside the tibiofibular mortise, and three ligamentous complexes, the lateral, medial and the syndesmotic ligaments. Together, the bony and ligamentous structures provide a ring-like stability apparatus. The current definition of rotational ankle fracture stability is based on this ankle osseoligamentous ring integrity. When the ring is interrupted in one place in isolation, the stability is usually preserved; however, when the ring is injured in two places, then it becomes unstable [1, 2].
Posterior malleolar fractures Bartoníček/Rammelt type 2 represent an avulsion fracture that includes the insertion of the posterior inferior tibiofibular ligament (PITFL) and part of the tibial incisura, involving part of the footprint of the interosseous tibiofibular ligament (ITFL) [2,3,4]. In the setting of an acute isolated non-displaced posterior malleolar fracture of Bartoníček/Rammelt type II with normal radiographic stability parameters, such as medial clear space and tibiofibular clear space within normal limits, it is often difficult and controversial to define fracture stability and to recommend in favor or against surgical treatment.
The value of clinical tests to detect instability, such as palpation of the syndesmosis, and the squeeze, Cotton, fibular translation and external rotation stress tests, is limited because of their questionable reliability and variable patient’s perception of pain [4, 5]. Finally, imaging studies, such as radiographs and magnetic resonance imaging (MRI), have been proven insufficient for complete and meticulous assessment of rotational ankle fractures [3, 5,6,7,8,9,10,11,12].
In this context, computed tomography (CT) allows a better assessment of bony injuries, degree of fragment displacement, and changes in bone relationship that can indicate fracture instability [4, 13]. CT findings are usually extremely helpful in the assessment of fractures of the anterior and posterior malleolus, syndesmosis injury, intercalated fracture fragments and impaction of the tibial plafond [12]. However, similar to MRI, conventional CT is a static, non-weight-bearing imaging modality, whose findings might not directly correlate with the presence of tibiotalar or syndesmotic instability, particularly in the setting of subtle instability. More recently, conventional ankle CT with stress maneuvers has been shown useful for the decision making of many orthopedic disorders of the foot and ankle [11,12,13].
Our hypothesis was that acute conventional ankle CT with stress maneuvers in patients sustaining malleolar fractures would provide accurate assessment to differentiate between stable and unstable injuries. In the present study, conventional ankle CT with external rotation and dorsiflexion was used to assess syndesmotic and fracture instability in the setting of acute, isolated, non-displaced Bartoníček and Rammelt type II posterior malleolar fractures.
Patients and methods
This multi-center cross-sectional study was conducted with the approval of the Ethics Committee (62100016.5.0000.0071). Patients signed and dated the informed consent form before providing demographic data or performing imaging examinations. A consecutive sample of individuals with the orthopedic diagnosis of an ankle sprain, assisted at the Foot and Ankle Outpatient Clinic, was referred to the Radiology Department after standard weight-bearing X-ray investigation (anteroposterior, lateral and mortise views) to perform MRI investigation. Patients were prospectively enrolled according to the following inclusion criteria: adults aged 18 years and older; acute unilateral ankle sprain episode up to 3 weeks before; those participants who presented syndesmotic, lateral or medial ligament injury and isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II in MRI [5] were selected for stress CT protocol (after signing the consent form). The exclusion criteria were previous surgery; lateral malleolus fracture; medial malleolus fracture; congenital or acquired ankle deformities; and infection, inflammatory or neuropathic ankle arthropathies.
MRI technical and reading parameters
A phased array dedicated coil on 1.5-T magnet HDX (GE Healthcare, Milwaukee, USA) was used to perform all of the MRI examinations using the following sequences: sagittal T1-weighted (TR/TE, 542/9; the number of excitations [NEX], 1; matrix, 320 × 256; thickness, 4 mm; field of view [FOV], 10 cm); sagittal T2-weighted fat-suppressed (3000/39, 2, 384 × 224, 4, 10); axial T2-weighted fat-suppressed (3483/48, 2, 384 × 224, 4, 10); coronal T2-weighted fat-suppressed (3000/39, 2, 384 × 224, 3, 10) and coronal oblique DP-weighted (2840/35, 2, 384 × 224, 3, 10).
Radiologists classified the anterior inferior tibiofibular ligament (AITFL) posterior inferior tibiofibular ligament (PITFL), interosseous tibiofibular ligament (ITFL), superficial deltoid ligament and deep deltoid ligament as grade 0 (normal ligament), grade I (strained with soft tissue edema around the ligament but still intact), grade II (partially torn with high signal intensity and thickening) or grade III (completely torn with avulsion or discontinuity) [7]. All measurements were taken blindly.
CT scan technical and reading parameters
An Aquilion ONE V6 scanner (Toshiba Medical Systems, Tochigi, Japan) with 320 channels was used to perform the CT examinations using the following technical parameters: a volumetric acquisition, 120 kV, 150 mA, 0.5 s rotation time, 0.5 mm slice thickness, 0.25 mm interpolation, 320-detector rows, a field of view medium or large and fine filter for bone.
All patients underwent a CT scan with stress maneuvers (CTSM), following a protocol reported previously, comprising a first phase with the ankles in a neutral position, then a stress phase with the ankles in external rotation and dorsiflexion and semi-flexed knees.
The narrowest tibiofibular distance was measured in the axial plane using the image where the whole shape of the tibial plafond began to show [13] (Fig. 1). For consistency, we kept the same label d, as described by Ahn et al. [13]. The CT measurement d at the joint level has the best correlation with the exact arthroscopic measurement, reaching an area under the ROC curve of 0.86 for diagnosing syndesmotic instability.
Ankle CT scan in the axial plane. The sclerotic band on the distal tibia corresponding to the tibial plafond was used as a reference (red asterisk). In addition, the medial tibiotalar joint line may start to show on the image (red hashtag). The d measurement is the narrowest distance of the tibiofibular syndesmosis (red line pointed by the white arrow)
Due to significant interindividual variability, we measured the distance d for both syndesmoses of the same individual, and the uninjured syndesmoses were used as the normal standard. The difference in measurement d between injured and uninjured syndesmoses defined instability.
Based on a recent study, which showed significant differences in the distances between injured and uninjured syndesmoses estimated at 1.0 mm [4], we adopted a 1.0 mm cutoff point to define instability. In the current study, the d difference of less than 1.0 mm classified the syndesmoses as stable, while the d difference greater than or equal to 1.0 mm was classified as unstable.
Another essential cutoff point of 2.0 mm [26], often used as a guideline for treatment, was also adopted in this study. The measurement of the d difference smaller than 2.0 mm classified the syndesmoses as minor instability, generally indicating non-operative treatment. Differences d greater than or equal to 2.0 mm were classified as a relevant instability, generally indicating surgical treatment.
In addition, the percentage of the tibial articular surface affected by the posterior malleolus fracture was analyzed in the sagittal plane of the CT scan. First, the anteroposterior diameter of the articular surface of the tibia affected by the fracture was divided by the total anteroposterior diameter of the articular surface. Next, the strength of association between the percentage of tibial joint surface involvement and the d difference measurement determined the correlation between posterior malleolus fracture and syndesmotic instability.
Again, radiologists performed all measurements blindly.
West Point grading system
The West Point grading system classifies syndesmotic injuries into three instability categories [7]. An isolated tear of the AITF ligament does not cause instability and defines grade I. Combined tear of the AITF and IO ligaments defines grade II, which can be divided into IIA (stable) and IIB (unstable). Finally, the combined injury of the AITF, IO and PITF ligaments causes frank instability and defines grade III.
Investigators used the patterns of ligament tear found at MRI and instability at CTSM to classify all participants into West Point grades I, IIA, IIB or III.
Statistical analysis
Absolute frequencies and percentages described categorical variables. In addition, means, standard deviation (SD), medians, quartiles and minimum and maximum values defined numerical variables depending on the parametric or nonparametric distribution according to the Shapiro–Wilk test. Mann–Whitney test was used to test the differences in the numerical variables between injured and uninjured ankles. The strength of the association between the tibial joint surface involved in posterior malleolus fracture and syndesmotic instability was assessed with the Spearman correlation test.
The MedCalc Statistical Software (MedCalc Software Ltd, Oostende, Belgium), version 19.4.0, analyzed the data, considering a power of 80%, a 5% significance level and 95% confidence intervals. All statistical tests were two-sided and appropriate for parametric or nonparametric distributions.
Results
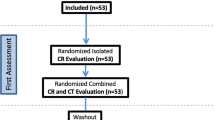
Between March 2018 and September 2022, 123 patients were assessed for eligibility. In total, 33 patients met the inclusion criteria.
Of these, approximately half (16/33) were male, with a mean age of 41 years. Seventeen ankle sprains occurred on the right side, mainly related to sports activity (25/33). Other causes for ankle sprains were walking on uneven sidewalks in five patients and falling on slippery stairs in three. The main complaint was ankle pain in all patients. In addition, approximately half of the patients had edema (17/33) and ecchymosis (16/33) on the lateral side of the ankle.
CT scan reading parameters
During the stress phase, the injured and uninjured syndesmoses had distinct behavior, and the 2.3 mm median difference for d measurement was statistically significant (P < 0.0001) (Table 1). In the neutral phase, the median difference of 0.2 mm in d measurements between injured and uninjured syndesmoses was not statistically significant (P = 0.057) (Table 2).
Applying the cutoff point of 1.0 mm, all patients had the d difference measurement inferior to 1.0 mm in the neutral phase, indicating that they had an acceptable tibiofibular relationship (Fig. 3). On the other hand, all patients had a d difference superior to or equal to 1.0 mm and were considered unstable in the stress phase. Figure 2 shows the typical finding of the current study.
A man, 64 years old, had a right ankle sprain five days ago. 3A: CT scan axial image in neutral phase showing posterior malleolus fracture Bartoníček and Rammelt type II and an usual tibiofibular relationship with d difference measurement less than 1.0 mm. 3B: CT scan axial image with stress maneuvers showing instability of the right tibiofibular syndesmosis with d difference greater than 2.0 mm
The anteroposterior diameter of the tibial joint surface involved in the PM fracture varied between 1.1 and 9.3 mm, with a median of 3.2 mm. Dividing the anteroposterior diameter of the tibia surface involved in the fracture by the total anteroposterior diameter of the tibia joint surface, we found the median percentage of the joint involvement was 12%, with a minimum value of 4% and a maximum of 31%. The Spearman correlation coefficient was 0.24 (P = 0.18, 95% CI − 0.11–0.53), confirming there was no association between the percentage of involvement of the tibia joint surface in the PM fracture and syndesmotic instability, considering the d difference in the CTSM. A scatter diagram with a heat map shows the distribution of the two variables (Fig. 3).
MRI reading parameters
Two patterns of syndesmotic ligament injury predominated when reading the MRI. A completely torn AITFL and IO ligament were found in two-thirds (22/33) of the participants, while a completely torn AITFL was combined with a partially torn IO in one-third (11/33). The PITF ligament was classified as normal in 23, strained in nine and partially torn in one patient. The superficial portion of the deltoid ligament was classified as normal in 25, strained in five and partially torn in one patient. The deep portion of the deltoid ligament was classified as normal in 28, strained in three, and partially torn in two. No patient had a completely torn PITFL, superficial or deep deltoid ligament.
West Point grading system
In the CT scan, all 33 patients presented a West Point grade IIB latent instability defined as a stable syndesmosis in the neutral phase and unstable in the stress phase (Table 2). About two-thirds (21/33) had an instability greater than or equal to 2.0 mm, and one-third (12/33) between 1.0 and 1.9 mm (Table 2). No patient was classified as grade I, IIA or III.
When analyzed along with the MRI findings, 18 out of 21 patients (83%) with instability greater than or equal to 2.0 mm were classified as having completely torn AITF and IO ligaments (Table 2). Ten out of 12 patients (83%) with instability between 1.0 and 1.9 mm were classified as having a completely torn AITF ligament combined with a partially torn IO (Table 2).
Discussion
Although highly specific and sensitive for syndesmotic injury, MRI does not provide a dynamic assessment. Thus, although a rupture of one or more ligaments can be identified, instability only suspected with an MRI [14]. In our study, the use of conventional ankle CT with stress maneuvers (external rotation and dorsiflexion) (Fig. 4) could reliably demonstrate the existence of instability of the syndesmosis after an isolated, non-displaced posterior malleolar (PM) fracture of Bartoníček and Rammelt type II. Using this method, two-thirds of patients had instability greater than or equal to 2.0 mm and one-third between 1.0 and 1.9 mm. This was closely correlated to our MRI findings, where two-thirds of patients had complete injury of the AITF and IO ligaments, and one-third had complete injury of the AITF ligament and incomplete injury of the IO ligament. No patient had a completely torn superficial or deep deltoid ligament, or PITF ligament. Applying the West Point grading system, all patients had latent instability, defined as a stable syndesmosis in the neutral phase and unstable in the stress phase (grade IIB). These findings support the Lauge-Hansen concept of equivalence of ligamentous and bony injuries around the ankle, namely that there is either a rupture of the PITFL or an osseous avulsion of the posterior tibial rim, that is, a PM fracture [14] (Fig. 5). The finding that a sprain or incomplete rupture of the PITFL was seen in MRI concurrent with a PM fracture in 10 cases may be explained by the fact that the footprint of the PITFL is larger than the average size of the PM fragment and therefore bony and ligamentous injury may concur, particularly with smaller PM fragments [14, 15].
Case example: A standard weight-bearing X-ray AP view right and left ankles, B standard weight-bearing X-ray AP view right and left ankles, C MRI sagittal view showing acute isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II, MRI axial view showing acute isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II, MRI axial view showing acute anteroinferior tibiofibular ligament rupture, MRI coronal view showing acute interosseous ligament rupture, D CT stress phase 1, E CT stress phase 2, F standard weight-bearing X-ray AP and lateral view post-operative control right ankle
In addition, there was no association between the percentage of involvement of the articular surface of the tibia due to the fracture of the posterior malleolus and syndesmotic instability (P = 0.18). The median percentage of the joint involvement was 12%, with a minimum value of 4% and a maximum of 31% which is consistent with a Bartoníček and Rammelt type II posterior malleolar fracture [3]. It may be concluded that these fragments only carry a minor part of the ITFL and syndesmotic instability only results in conjunction with further ligamentous injuries like rupture of the AITFL and the ITFL. Our study is the first to look at a combination of bony and ligamentous syndesmotic injuries. Earlier studies have been showing similar findings regarding purely ligamentous lesions. In a systematic review and meta-analysis, Raheman et al. [16] showed that the syndesmotic area is the most reliable parameter in the evaluation of syndesmosis injuries because it increases in the presence of instability during weight bearing. In a prospective comparative study of 39 consecutive patients, Del Rio et al. [17] suggested that both the dynamic change in area and weight bearing in comparison with the contralateral uninjured ankle are 2 parameters that may prove useful in the future for predicting syndesmotic instability.
The utility of the uninjured side as a valid internal control for confirming potential syndesmotic instability has been emphasized by Hagemeijer et al. [18]. Using WBCT, these authors evaluated the distal tibiofibular joints in patients with known syndesmotic instability, comparing the findings between the injured and uninjured sides. Values differed between both sides in 4 of the 7 measurements performed including direct anterior, middle and posterior differences, and sagittal translation (P < 0.001 in all measures). Indeed, in a more recent study, Bhimani et al. [15] suggested that syndesmotic joint volume measurements, including the medial and lateral clear space volume, and the syndesmotic joint volume from the tibial plafond seem to be best suited to diagnose syndesmotic instability among patients with Weber B ankle fractures, compared with other two-dimensional (2D) and three-dimensional (3D) WBCT measurements. In another study, the same authors [34] demonstrated that 3D volumetric measurement of the syndesmosis joint is the most effective way to diagnose syndesmotic instability, compared with more traditional 2D syndesmosis measurement. This was also demonstrated by Ashkani Esfahani et al. [19], who showed that the ability to compare the ankle joints bilaterally in a 3D manner under physiologic weight provided by weight-bearing CT has led to a more accurate diagnostic method. In the current study using CTSM with simulated weight bearing, we found a 2.3-mm median increase of the tibiofibular distance of the injured syndesmosis compared to the uninjured syndesmosis of the same patient (P < 0.0001), proving that CTSM is a potential diagnostic tool to reveal latent syndesmotic instability.
Some authors have suggested that both the tibiofibular ligament laterally and the deep deltoid ligament medially being the structures most commonly injured in the ankle in association with malleolar fractures including proximal fractures of the fibula [20, 21]. Our findings do not support the concept that the deltoid ligament directly contributes to the genesis of syndesmotic instability.
Based on our findings, we believe that injury to the deltoid ligament is not a primary factor in the instability of the distal tibiofibular syndesmosis but may act secondarily by increasing the degree of instability in case of rupture. In a cadaver study, complete disruption of the syndesmosis with a disruption of the deltoid ligament caused a 40% decrease in the tibiotalar contact area and a 36% increase in the tibiotalar contact pressures [22]. Nevertheless, in the clinical setting, the relevance of deltoid incompetence remains unclear and stress-positive isolated fibular fractures, i.e., with medial clear space widening on gravity stress testing, have excellent outcomes following non-operative treatment [23]. Future studies comparing WBCT and MRI may correlate the presence and size of posterior malleolus fractures with the existence of deltoid ligament injuries, decreased tibiotalar contact area and increased tibiotalar contact pressures.
It has been shown that anatomic reduction and stable fixation of even small PM fragments also provides stability to the syndesmosis, thus reducing the need for indirect syndesmotic fixation and leading to improved outcomes [1, 21]. Moreover, Fitzpatrick et al. [24] showed that medial–lateral syndesmotic reduction was affected by the quality of the PM fixation, with malreduction of the PM leading to syndesmotic malreduction. The present study supports the concept of stable fixation of smaller PM fragments to increase syndesmotic stability.
Our study has some limitations. First, we do not report on outcomes. Thus, the clinical relevance of non-surgical vs. surgical treatment of non-displaced syndesmotic avulsions with latent instability remains to be elucidated in further studies. Second, due to pain from the acute ankle injury, patients may have partially unloaded the lower extremity during image acquisition. Because we did not employ pain intensity measures such as the visual analog scale (VAS), our findings may be biased.
The strengths of our study include the homogeneous study group through the selection of patients with isolated, non-displaced Bartoníček and Rammelt type II PM fractures. To the best of our knowledge, this study is the first to look at a combination of bony and ligamentous syndesmotic injuries with prospective MRI and CTSM evaluation for all patients. Furthermore, we were able to show the importance of imaging stress tests in the assessment of initially non-displaced Bartoníček and Rammelt type II PM fractures, reinforcing some authors who showed that posterior malleolus fracture potentially leads to ankle instability and post-traumatic osteoarthritis of the ankle [1, 3, 5, 14, 21, 25].
Conclusion
In conclusion, conventional computed tomography with external rotation and dorsiflexion represents a reproducible and accurate diagnostic option for the detection of latent instability of the syndesmosis in the presence of acute isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II.
References
Rammelt S, Bartoníček J, Kroker L, Neumann AP (2021) Surgical fixation of quadrimalleolar fractures of the ankle. J Orthop Trauma 35(6):e216–e222
Nicolai C, Bierry G, Faruch-Bilfeld M, Sans N, Willaume T (2022) The concept of ring of injuries: evaluation in ankle trauma. Skeletal Radiol 51(10):2027–2037
Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I (2015) Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 135(4):505–516
Sman AD, Hiller CE, Refshauge KM (2013) Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: a systematic review. Br J Sports Med 47(10):620–628
Rammelt S, Bartoníček J, Kroker L (2022) Pathoanatomy of the anterolateral tibial fragment in ankle fractures. J Bone Joint Surg Am 104(4):353–363
Rammelt S, Bartoníček J, Schepers T, Kroker L (2021) Fixation of anterolateral distal tibial fractures: the anterior malleolus. Operat Orthop Traumatol 33(2):125–138
Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC (1998) Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int 19(10):653–660
Nortunen S, Flinkkilä T, Lantto I, Kortekangas T, Niinimäki J, Ohtonen P, Pakarinen H (2015) Diagnostic accuracy of the gravity stress test and clinical signs in cases of isolated supination-external rotation-type lateral malleolar fractures. Bone Joint J 97B(8):1126–1131
Seidel A, Krause F, Weber M (2017) Weightbearing vs gravity stress radiographs for stability evaluation of supination-external rotation fractures of the ankle. Foot Ankle Int 38(7):736–744
Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, Swierstra BA (2004) Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Rel Res 423:227–234
Vogl TJ, Hochmuth K, Diebold T, Lubrich J, Hofmann R, Stöckle U, Söllner O, Bisson S, Südkamp N, Maeurer J, Haas N, Felix R (1997) Magnetic resonance imaging in the diagnosis of acute injured distal tibio-fibular syndesmosis. Invest Radiol 32(7):401–409
Rodrigues JC, do Amaral e Castro A, Rosemberg LA, de Cesar Netto C, Godoy-Santos AL (2023) Diagnostic accuracy of conventional ankle CT scan with external rotation and dorsiflexion in patients with acute isolated syndesmotic instability. Am J Sports Med 51(4):985-996
Ahn TK, Choi SM, Kim JY, Lee WC (2017) Isolated syndesmosis diastasis: computed tomography scan assessment with arthroscopic correlation. Arthroscopy 33(4):828–834
Rammelt S, Boszczyk A (2023) Ligament ruptures in ankle fractures - was Lauge-Hansen right? Foot Ankle Clin 28(2):445–461
Bhimani R, Ashkani-Esfahani S, Lubberts B, Kaiser P, Kerkhoffs GMMJ, Waryasz G, DiGiovanni CW, Guss D (2022) Utility of WBCT to diagnose syndesmotic instability in patients with Weber B lateral malleolar fractures. J Am Acad Orthop Surg 30(3):e423–e433
Raheman FJ, Rojoa DM, Hallet C, Yaghmour KM, Jeyaparam S, Ahluwalia RS, Mangwani J (2022) Can weightbearing cone-beam CT reliably differentiate between stable and unstable syndesmotic ankle injuries? A systematic review and meta-analysis. Clin Orthop Relat Res 480(8):1547–1562
Del Rio A, Bewsher SM, Roshan-Zamir S, Tate J, Eden M, Gotmaker R, Wang O, Bedi HS, Rotstein AH (2020) Weightbearing cone-beam computed tomography of acute ankle syndesmosis injuries. J Foot Ankle Surg 59(2):258–263
Hagemeijer NC, Chang SH, Abdelaziz ME, Casey JC, Waryasz GR, Guss D, DiGiovanni CW (2019) Range of normal and abnormal syndesmotic measurements using weightbearing CT. Foot Ankle Int 40(12):1430–1437
Ashkani Esfahani S, Bhimani R, Lubberts B, Kerkhoffs GM, Waryasz G, DiGiovanni CW, Guss D (2022) Volume measurements on weightbearing computed tomography can detect subtle syndesmotic instability. J Orthop Res 40(2):460–467
Femino JE, Vaseenon T, Phisitkul P, Tochigi Y, Anderson DD, Amendola A (2013) Varus external rotation stress test for radiographic detection of deep deltoid ligament disruption with and without syndesmotic disruption: a cadaveric study. Foot Ankle Int 34(2):251–260
Rammelt S, Bartoníček J (2020) Posterior malleolar fractures. A critical analysis review. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.19.00207
Wiegerinck JJI, Stufkens SA (2021) Deltoid rupture in ankle fractures: to repair or not to repair? Foot Ankle Clin 26(2):361–371
Stockwell E, Thomas P, Grossman L, Lyden E, Mormino M, Siebler J, Putnam S (2024) Successful outcomes with nonoperative treatment and immediate weightbearing despite stress-positive radiographs in isolated distal fibula (OTA/AO 44B) fractures. J Orthop Trauma 38(1):e20–e27
Fitzpatrick E, Goetz JE, Sittapairoj T, Hosuru Siddappa V, Femino JE, Phisitkul P (2018) Effect of posterior malleolus fracture on syndesmotic reduction: a cadaveric study. J Bone Joint Surg Am 100(3):243–248
Giordano V, Babinski MA, Freitas A, Pires RE, Souza FS, Faria LPG, Labronici PJ, Godoy-Santos A (2023) Biomechanical efficacy of three methods for the fixation of posterior malleolar fractures: a three-dimensional finite element study. Diagnostics (Basel) 13(23):3520
Funding
The authors did not receive grants or outside funding in support of their research for or preparation of this manuscript. They did not receive payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, educational institution or other charitable or non-profit organization with which the authors are affiliated or associated.
Author information
Authors and Affiliations
Contributions
ALGS contributed to conceptualization, methodology, supervision and writing—original draft. JCR and DCBS were involved in data curation. CCN, NSBM and KAMC contributed to formal analysis and investigation. VG and SR were involved in validation, visualization and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest related to the content of this article.
Ethical approval
The study was approved by the institutional review board (62100016.5.0 000.0071) and followed the Standards for Reporting Diagnostic Accuracy Studies (STARD) guidelines. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Godoy-Santos, A.L., Rodrigues, J.C., Barros-Santos, D. et al. The role of computed tomography with external rotation and dorsiflexion in decision making for acute isolated non-displaced posterior malleolar fractures Bartoníček and Rammelt type II: a prospective study. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03952-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03952-4