Abstract
Objective
To determine the prevalence and diagnostic significance of fluid-fluid levels (FFLs) in focal bone lesions.
Design and patients
Clinical and radiological details of 738 consecutive patients referred with focal lesions of bone and who had undergone MRI were reviewed. FFLs were identified in 83 (11.2%). The proportion of the lesion occupied by FFLs was estimated, based on imaging in all available planes, as <1/3, 1/3–2/3, >2/3 but not the entire lesion, and complete. The degree of FFL change in each lesion was correlated with the final diagnosis, which was either histological (n=80) or clinicoradiological (n=3). There were 31 female and 52 male patients, mean age 25.5 years (range 5–83 years).
Results
Histology revealed 46 benign, 32 malignant and 2 non-neoplastic lesions. A clinicoradiological diagnosis was made in the 3 lesions without histology: 2 were benign (simple bone cyst and intraosseous lipoma) and 1 malignant (a metastasis). Malignant neoplasms commonly showed FFLs which occupied <1/3 of the entire lesion (n=22/32, 68.8%), and 50% of all the lesions in this group were conventional intramedullary osteosarcomas (n=16). With increasing FFL change, malignancy became less frequent: with >2/3 (but incomplete) FFL change, 81% (n=13/16) of tumours were benign. If the entire tumour showed FFL change, the histology was benign in 100% (n=11).
Conclusions
The extent of FFLs within a focal bone lesion appears to be inversely related to the degree of malignancy. If at least 2/3 of the lesion shows FFL change, 89% of diagnoses are benign.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fluid-fluid levels (FFLs) in bone lesions were initially described as a feature of an aneurysmal bone cyst (ABC) and then telangiectatic osteosarcoma, using X-ray CT [1, 2]. Subsequently, they were reported in an ABC using MRI [3], and comparison of the signal characteristics and relaxation times with a sample of anticoagulated blood showed similar characteristics. FFLs have since been demonstrated in a large number of both benign [4, 5, 6, 7, 8, 9, 10, 11] and malignant [11, 12, 13] bone lesions, leading some authors to conclude that they are a non-specific finding in bone and soft-tissue tumours [11, 13]. Secondary ABC formation within a primary lesion, which occurs with a frequency of 0–35% in several large series [14, 15, 16, 17, 18], may be the cause. The presence of FFLs may also be due to necrosis within the tumour, which may follow chemotherapy or radiotherapy [19].
The current study was performed to determine the prevalence and clinical relevance of FFLs demonstrated by MRI, and to correlate the extent of FFL change with final diagnosis.
Patients and methods
Between September 1998 and July 2002, clinical and radiological data from 1021 consecutive bone lesions were collected. These patients were referred to the London Bone and Soft Tissue Tumour Service for further management of suspected primary bone tumours. Only new referrals were included in the analysis, excluding treated or recurrent tumours.
Demographic and imaging details were entered onto a database as the patient was being investigated and treated, resulting in a prospective archive of a large number of bone lesions.
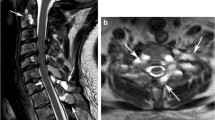
We reviewed 742 patients who were further investigated using MRI, either at the referring hospital or our unit. Four patients were excluded, as neither the MRI nor clinical details could be obtained for complete review, leaving 738 patients. A wide range of MRI scanners and protocols were used. However, a long axis (sagittal or coronal) or axial T2-weighted fast spin-echo (W FSE) or short T1 inversion recovery (STIR) sequence was available in all cases. All 738 examinations were evaluated prospectively for the presence of FFLs by a single experienced musculoskeletal radiologist (AS), who had no knowledge of the lesion histology. The proportion of the lesion occupied by FFLs was estimated from the MRI scan using a combination of long axis and transverse images, and results recorded under one of the following four headings: group 1, <1/3, where FFLs occupied less than one-third of the total volume of the lesion; group 2, 1/3–2/3, where FFLs occupied between one- and two-thirds of the volume of the lesion; group 3, >2/3 but incomplete, where FFLs occupied over two-thirds of the volume of the lesion, but there was adjacent solid tumour; and group 4, complete, where the entire lesion showed FFLs, with no additional solid component. Examples from these groups are shown in Figs. 1, 2, 3 and 4. The degree of FFL change was correlated with both final diagnostic category (benign, malignant or non-neoplastic) and eventual diagnosis, which was again either histological (n=80) or clinicoradiological (n=3).
Results
Of the 738 cases, the histological (n=624) or clinical (n=114) diagnosis (made using a combination of radiology and clinical follow-up) is recorded in Tables 1, 2 and 3. A total of 83 lesions (11.2%) contained FFLs. Of the 83 patients who showed FFLs on MRI, 31 were female and 52 male. Their mean age was 25.5 years, with a range of 5–83 years. All of these lesions were intramedullary with the exception of 2: 1 intracortical and 1 surface ABC. Multiple FFLs were the norm, occurring in 75 cases, with a single FFL noted in only 8.
Forty-eight patients had benign lesions, 33 malignant and 2 non-neoplastic (osteomyelitis, n=2). Diagnoses were confirmed histologically in 80 cases. Two benign lesions were diagnosed using a combination of imaging appearances and clinical follow-up: the first was a male patient aged 20 years with a non-progressive lucency in the femoral neck, unchanged in appearance for the preceding 4 years, diagnosed as a simple bone cyst. The second was an intraosseous lipoma in a middle-aged man, the diagnosis being made on MRI. One malignant lesion was diagnosed clinicoradiologically, after a needle biopsy of a mass in the bony pelvis under imaging guidance yielded only necrotic tissue. The patient was an elderly man with multiple pulmonary nodules, and the lesion was assumed to be metastatic.
In 33 patients, FFLs occupied less than 1/3 of the lesion (group 1). Ten (30%) of these were benign (one diagnosed radiologically as intraosseous lipoma); 22 (67%) were malignant, and 1 (3%) non-neoplastic. The diagnoses of the benign and malignant lesions are shown in Fig. 5, from which it is evident that half of the tumours (n=16) were osteosarcomas. All of these were conventional, intramedullary tumours. No ABCs or telangiectatic osteosarcomas were seen in this group.
In 22 patients, FFLs occupied between 1/3 and 2/3 of the lesion (group 2). Thirteen (59%) of these were benign, 8 (36%) were malignant (one diagnosed clinicoradiologically as metastatic disease), and 1 non-neoplastic (5%). The diagnoses of the benign and malignant lesions are shown in Fig. 6. Osteosarcoma was still the most common tumour (n=6, all conventional, intramedullary tumours), followed by ABC (n=5).
In 16 patients, FFLs occupied over 2/3 but not the entire lesion (group 3). Thirteen (81%) of these were benign and 3 malignant (19%). The diagnoses are shown in Fig. 7. The most common lesion was ABC (n=7, 44% of patients in group 3). The only malignant tumours showing this degree of FFL change were telangiectatic osteosarcomas (n=2, Fig. 8) and a necrotic metastasis (n=1).
A 20-year-old man, histological diagnosis of telangiectatic osteosarcoma. AP radiograph (A) shows aggressive bone destruction in the tibial diaphysis and a pathological fracture. Coronal T1W (B) and STIR (C) MR images confirm a large, haemorrhagic, extraosseous mass. Axial fat-suppressed T2W images (D) show most of the mass (estimated to be >2/3) to be occupied by FFLs. Solid intramedullary tumour is also visible
In 12 patients, the entire lesion showed FFL change (group 4), and all of these tumours were benign (including one simple bone cyst diagnosed radiologically). The diagnoses are shown in Fig. 9.
Combining the results from groups 3 and 4, if at least 2/3 of the lesion is occupied by FFLs, 89% (n=25/28) of the diagnoses are benign.
Discussion
Since the initial observation of FFLs on CT and MR images of ABCs, they have been identified in many different types of tumour. Although still classically associated with ABCs, the presence of FFLs has consequently become a non-specific observation. To our knowledge, no previous studies have addressed the degree of FFL change within individual lesions with a view to aiding diagnosis. The results of this study suggest that the extent of FFL change may be of assistance in differentiating benign from malignant tumours.
As the proportion of the lesion occupied by FFLs increases, so does the frequency of benign diagnoses. Some 81% of diagnoses in group 3 and 100% of those in group 4 were benign. This may be valuable in eliminating the need for diagnostic biopsy prior to surgery in lesions that are completely occupied by FFLs.
Conversely, if only a small proportion (<1/3) of the lesion is occupied by FFLs (group 1), the majority (67%) of diagnoses are malignant. Conventional intramedullary osteosarcoma shows this degree of FFL change particularly commonly.
Three high-grade malignant lesions were seen in group 3, demonstrating FFL change in over 2/3 of the mass. These lesions also possessed a small solid component, but similar MR imaging features were also seen in ABCs, which was the most common tumour in this group. Therefore, although usually suggesting a benign pathology, FFLs filling the majority of the mass can also be seen in aggressive, predominantly necrotic malignant tumours. In particular, differentiation of telangiectatic osteosarcoma and ABC based on visualization of FFLs either on CT or MRI can be problematic, as has been noted previously [19]. The plain radiograph may help to differentiate here, demonstrating the rate of growth of the lesion more accurately than MRI. FFLs tend to occur in the mid- and late stages of development of ABCs, and not the incipient (‘permeative’) stage [19], and radiographic appearances should therefore show more indolent features. However, radiographic features may be non-specific [20], either due to rapid growth of an ABC, or slow growth of an osteosarcoma. Sundaram et al. [21] reported the imaging findings in four cases of pseudocystic osteosarcoma, whose radiographic appearances were most in keeping with ABC or simple bone cyst. One of these, an osteoclast-rich osteosarcoma of the navicular, showed secondary ABC formation and multiple FFLs on MRI. It should therefore be remembered that malignant lesions may on occasion be predominantly cystic with multiple FFLs.
In summary, 11.2% of a cohort of 738 consecutive focal bone lesions showed FFLs on MRI. Sixty-seven percent of the lesions showing less than 1/3 of the tumour to be occupied by FFLs were malignant, and half of these were conventional intramedullary osteosarcomas. If at least 2/3 of the lesion showed FFL change, the diagnosis was benign in 89% of cases. We conclude that, in the majority of cases, extensive FFLs are associated with benign disease, with the caveat that necrosis within a malignant lesion may result in a similar appearance. Clinical features and radiographs should be used in these instances to differentiate ABC from telangiectatic osteosarcoma or metastasis, which are the most likely malignant diagnoses.
References
Hudson T. Fluid levels in aneurysmal bone cysts: a CT feature. AJR 1984; 141:1001–1004
Hertzanu Y, Mendelsohn D, Gottschalk F. Aneurysmal bone cyst of the calcaneus. Radiology 1984; 151:51–52
Hudson T, Hamlin D, Fitzsimmons J. Magnetic Resonance Imaging of fluid levels in an aneurysmal bone cyst and in anticoagulated human blood. Skeletal Radiol 1985; 13:267–270
Kudo T, Okada K, Hirano Y, Sageshima M. Chondroblastoma of the metacarpal bone mimicking an aneurysmal bone cyst: a case report and review of the literature. Tohoku J Exp Med 2001; 194:25–257
Maas E, Craig J, Swisher P, Amin M, Marcus N. Fluid-fluid levels in a simple bone cyst on magnetic resonance imaging. Australas Radiol 1998; 42:267–270
Buetow P, Newman S, Kransdorf M. Giant cell tumor of the tibia in a child presenting as an expansile metaphyseal lesion with fluid-fluid levels on MR. Magn Reson Imaging 1990; 8:341–344
Grey A, Mangham C, Davies A, Grimer R. Fluid-fluid level in an intraosseous ganglion. Skeletal Radiol 1997; 26:667–670
Davies A, Evans N, Mangham C, Grimer R. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol 2001; 11:1445–1449
Vilanova J, Maestro de Leon J, Aparico A, Capdevila A. MR imaging of a malignant schwannoma and an osteoblastoma with fluid-fluid levels. Report of two new cases. Eur Radiol 1998; 8:1359–1362
Rafii M, Firooznia H, Golimbu C, McCauley D. Hematogenous osteomyelitis with fat-fluid level shown by CT. Radiology 1984; 153:493–494
Tsai J, Dalinka M, Fallon M, Zlatkin M, Kressel H. Fluid-fluid level: a non-specific finding in tumors of bone and soft tissue. Radiology 1990; 175:779–782
Harter S, Nokes S. Plasmacytoma of the sacrum: fluid-fluid levels on MR images. AJR 1995; 165:741–742
Sone M, Ehara S, Sasaki M, et al. Fluid-fluid levels in bone and soft tissue tumors demonstrated by MR imaging. Nippon Igaku Hoshasen Gakkai Zasshi 1992; 52:1110–1115
Tillman B, Dahlin D, Lipscomb P, Stewart J. Aneurysmal bone cyst: an analysis of ninety-five cases. Mayo Clin Proc 1968; 43:478–495
Koskinen E, Visuri T, Holmstrom T, Roukkula M. Aneurysmal bone cyst: evaluation of resection and curettage in 20 cases. Clin Orthop 1976; 118:136–146
Szendroi M, Cser I, Konya A, Renyi-Vamos A. Aneurysmal bone cyst. A review of 52 primary and 16 secondary cases. Arch Orthop Trauma Surg 1992; 111:318–322
Martinez V, Sissons H. Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other pathology. Cancer 1988; 61:2291–2304
Bonakdarpour A, Levy W, Aegerter E. Primary and secondary aneurysmal bone cyst: a radiological study of 75 cases. Radiology 1978; 126:75–83
Davies A, Cassar-Pullicino V, Grimer R. The incidence and significance of fluid-fluid levels on computed tomography of osseous lesions. Br J Radiol 1992; 65:193–198
Kaufman R, Towbin R. Telangiectatic osteosarcoma simulating the appearance of an aneurysmal bone cyst. Pediatr Radiol 1981; 11:102–104
Sundaram M, Totty W, Kyriakos M, McDonald D, Merkel K. Imaging findings in pseudocystic osteosarcoma. AJR 2001; 176:783–788
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Donnell, P., Saifuddin, A. The prevalence and diagnostic significance of fluid-fluid levels in focal lesions of bone. Skeletal Radiol 33, 330–336 (2004). https://doi.org/10.1007/s00256-004-0779-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-004-0779-5