Abstract
Objective
To determine if it is possible to measure glenoid bone loss by using the Bernageau view and to compare it to a 3D CT scan.
Materials and methods
Fifty healthy subjects with a mean age of 34 ± 8 years old and 31 (62 %) male were submitted to the Bernageau view X-ray of both shoulders. Three blinded evaluators measured the distance between the posterior and anterior glenoid rim. Ten patients with multiple episodes of unilateral traumatic anterior shoulder dislocation with a mean age of 34 ± 9.1 years old and 90 % male were submitted to the same X-ray technique to determine the percentage of glenoid bone loss. They were also submitted to a bilateral 3D CT scan to be compared to the radiographs.
Results
In the 50 asymptomatic subjects, the AP distance was 24.48 mm ± 3.32 mm in the left shoulder and 24.82 mm ± 3.16 mm in the right shoulder. Comparing the X-ray study and the 3D CT scan of the ten patients with multiple episodes, there was no significant statistical difference of the AP normal distance in both methods (p = 0.646), the AP erosion distance (p = 0.386), as well as the percentage of bone loss (p = 0.513). Moreover, the differences between the percentages of bone loss in the X-ray, compared with the 3D CT scan were, on average 2.28 % (range 0 to 6.05 %).
Conclusions
The Bernageau radiographic view is an accurate and reproducible technique for measuring the presence of glenoid erosion, with similar results when compared to the 3D CT scan.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Antero-inferior glenoid rim bone loss has been related to the number of shoulder dislocations and, depending on its size, bone graft may be indicated to avoid shoulder dislocation recurrence [1–4]. Several radiographic views have been described to study recurrent shoulder dislocation and evaluate the anterior-inferior glenoid rim [5–8]; although radiographs have a low-cost and are commonly used, few studies have assessed their capability to measure antero-inferior glenoid bone loss. In addition to this, patient positioning is of utmost importance during an X-ray exam and the view utilized can be difficult to reproduce [5–7]. Edwards et al. have shown that by using the Bernageau profile view, it is possible to perform an adequate study of the anterior and inferior glenoid rims, and that 78.8 % of osseous abnormalities of the glenoid can be identified; a fluoroscopic device was used to confirm this technique’s reproducibility [6]. On the other hand, Itoi et al. have shown that the West Point view allows an accurate calculation of the anterior and inferior glenoid rim bone loss, in spite of the difficulty to reproduce this X-ray view [7].
The aim of this study was, first, to determine if it is possible to measure glenoid bone loss by using the Bernageau profile view and, second, to compare the Bernageau profile view to 3D CT scan in ten patients with multiple dislocations. To achieve this, the distance between the anterior and posterior glenoid rim and the difference between both shoulders need to be evaluated.
Materials and methods
Our institution’s ethical committee approved this project. All subjects read and signed an informed consent form. This prospective study was performed in two phases between June of 2009 and July of 2010. In the first phase, we analyzed if it would be possible to use the Bernageau profile X-ray view to calculate an antero-inferior glenoid bone loss. In the second phase, we compared this technique to 3D CT scan.
Phase I: Fifty healthy adult subjects were submitted to a radiographic evaluation of their shoulders (100 exams). The mean age of the subjects was 34 ± 8 years old (range: 20 to 68 years old) and 31 (62 %) were male. Patients were selected consecutively at the hospital’s general orthopedic clinic. For the first phase of the study, the inclusion criteria was absolutely no known history of shoulder pathology and the exclusion criteria was any kind of radiological abnormality at the shoulder or previous surgery at the shoulder.
Phase II: Ten patients (nine men, one woman) with traumatic shoulder dislocation with multiple episodes were evaluated (20 exams). The mean age of the subjects was 34 ± 9.1 years old (range: 19 to 47 years). The mean number of episodes was 32 (range 14 to 50 episodes). For the second phase of the study, the inclusion criteria was history of traumatic shoulder dislocation and the exclusion criteria was previous shoulder surgery or anatomical abnormalities not related to the dislocations.
Phase I
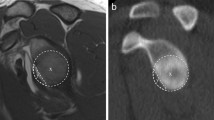
All subjects were submitted to a bilateral shoulder radiographic exam using the Bernageau profile view (Fig. 1a, b), performed as previously described [5, 6]. The X-ray tube (Shimadzu 1/2P38D; Shimadzu Corporation Kyoto—Japan) was positioned at a distance of 100 cm from the shoulder to be studied at an angle of 30º caudally and centered on the scapula spine. The patient was positioned standing with the arm to be studied at maximal forward flexion, usually 160 degrees at the scapular plane; the thorax in contact with the radiographic cassette at an angle of 70 degrees. A 10-cm-long number 3 Steinmann pin is positioned at the patient’s shoulder (fixed at the scapular spine) at the moment of the radiographic evaluation to control magnification [9].
The same technique was always applied (65 ± 5 kV, 20 mA) and, the same type and size of films were used for all subjects (FotoMed™—24 × 30 cm).
Using this position to perform the X-ray, usually no more than two repetitions were needed to obtain the Bernageau view. Our technician was trained to perform the patient positioning. There is also option to use fluoroscope to assist the positioning as described by Edwards et al. [6].
Phase II
Ten subjects with multiple episodes of unilateral traumatic anterior shoulder dislocation were submitted to the same X-ray technique described above to determine their percentage of glenoid bone loss. They were also submitted to a bilateral 3D CT scan (Phillips Brilliance 64-channel CT Scanner; Phillips Electronics—Koninklijke, The Netherlands) and, similar to the X-ray evaluation, the unaffected side served as control and the antero-posterior (AP) glenoid distance was considered to be 100 %. The affected side was measured in the same way, and the percentage of glenoid bone loss was calculated.
Measurement
-
a) X-rays
After performing the Bernageau profile view X-rays the distance between the anterior and posterior glenoid rim was calculated (Glenoid A-P distance), following the posterior and the anterior walls of the scapula.
Three blinded examiners performed this measurement; they were all shoulder surgeons with 10 or more years of experience. Each examiner repeated each measurement three times, with at least 1-week interval between measurements.
-
b) CT-scan
The largest glenoid AP distance of both sides was calculated using the tools provided by the 3D CT Scan software (Philips Brilliance Visualization Software) and the percentage of glenoid bone loss was calculated. A musculoskeletal radiologist with 15 years of experience made these measurements.
Statistical analysis
Pearson’s correlation coefficient was used to evaluate the intra-observer and inter-observer reproducibility and the Anderson-Darling normality test was used to study the variability of this distance, evaluating whether these objective measurements had normal distribution. The Wilcoxon test was used to compare the percentage of bone loss obtained by each method. The level of significance was set at 5 % (p < 0.05). Statistical analysis was performed with SPSS (Statistical Package for the Social Sciences, version 13.0, SPSS Ind., Chicago, IL).
Results
The distance between the anterior and posterior glenoid rims on the Bernageau profile view was measured for all normal X-rays (n = 100). The average distance was 24.82 mm ± 3.16 mm (range: 16.92–31.81 mm) in the right shoulder and 24.48 mm ± 3.32 mm (range: 18.64–32.22 mm) in the left shoulder.
The reproducibility was evaluated among the three measurements taken from each of the three evaluators. Pearson’s correlation test was used and a significant correlation among the three measurements of each examiner, as well as, among the three examiners, (p < 0.01) was found. The average intra-observer ICC was 0.965 for evaluator 1, for evaluator 2 it was 0.897, and for evaluator 3 it was 0.968. The average inter-observer ICC was 0.81 for the right side and 0.76 for the left side.
In addition to this, the distance from the anterior to the posterior glenoid rim had a normal distribution using the Anderson-Darling normality test (95 % of the samples within the confidence interval).
In regards to the ten subjects with anterior shoulder dislocation evaluated, the erosion percentage of the AP distance of the glenoid cavity calculated on the Bernageau view varied from 17.0 to 29.0 % (average 24.1 %) and, the erosion percentage calculated on the 3D CT scan varied from 19.0 to 31.0 % (average 23.4 %) (Tables 1 and 2). There was no significant statistical difference when comparing the AP normal distance in both methods (p = 0.646), the AP erosion distance (p = 0.386), as well as, the percentage of bone loss (p = 0.513) (Fig. 2a–d) Moreover, the differences between the percentages of bone loss in the X-ray, compared to the 3D CT Scan was, on average, 2.28 % (range 0 to 6.05 %) (Table 2).
Discussion
This study evaluated the utility of radiographs for measuring AP glenoid distance as well as anterior-inferior glenoid rim erosion. We have found that the Bernageau profile view is helpful in evaluating the anterior-inferior glenoid rim and in calculating the glenoid A-P distance and that the distances were not significantly different than those measured on a 3D CT scan.
In a cadaveric study performed by Bueno et al. in 61 scapulae specimens from the Anatomy Lab where one of the variables measured was the largest AP distance of the glenoid, an average of 26.38 mm ± 2.69 mm (range 20.03 mm to 32.35 mm) of the glenoid AP distance was obtained [10]. In the current study with the Bernageau view, the average distance was 24.82 mm ± 3.16 mm (range: 16.92–31.81 mm) in the right shoulder and 24.48 mm ± 3.32 mm (range: 18.64–32.22 mm) in the left shoulder. Those are very close values obtained in two different studies and therefore we used the same concept to measure the glenoid on the CT scan, measuring the largest AP glenoid distance and found no significant statistical difference.
Although radiographs are used to diagnose glenoid bone loss, only a few studies have described the possibility of using them to calculate the percentage of bone loss [6, 7, 11], and as the left and right shoulders presented with almost the same glenoid A-P distances, we believe that the unaffected shoulder can be used as a control to predict glenoid bone loss.
In addition to this, the glenoid A-P distances obtained in this study were similar to the distances found in previous studies as well as to the distances measured in the 3D CT scan. Churchill et al., after studying 344 scapulae, observed that the glenoid width was in average 27.8 ± 1.6 mm in males and 23.6 ± 1.5 mm on females [12]. Burkhart et al. studied the glenoid A-P distance in ten cadavers and found that this distance was, in average, 24.40 mm [13]. Kwon et al. studied the anatomy of the glenoid and compared it with CT scans and found that the maximum glenoid width at the cadavers measurement was, on average, 26.8 ± 5.0 mm and 25.2 ± 4.7 mm [14]. Ikemoto et al. observed that the maximum glenoid A-P distance was, on average, 24.21 mm ± 2.57 mm after evaluating 93 embalmed scapulae [15]. In 2010, Ikemoto et al. described how to perform a radiographic study with the Bernageau view [16].
Many authors believe that a circle can fit the inferior portion of the glenoid contour [11, 13, 17, 18] and this circle diameter is used arthroscopically to calculate glenoid bone loss. We believe that the A-P glenoid distance measured in the Bernageau profile view also represents the glenoid circle diameter and, when compared to the contra-lateral side, can be used to predict bone loss. According to some studies [17, 19, 20], the glenoid bone defect is anterior and we considered the diameter of the circle to be a good parameter to measure it.
At an anatomical study performed by Itoi et al. [21], progressive osteotomies of the glenoid were done and it was observed that a loss of the AP distance on average of 6.8 mm corresponds on average to a decrease of 21 % of the glenoid surface area, to 21 % of the glenoid length and to 25 % of the AP distance, being the critical size of erosion where bone grafting is needed. With that in mind, we considered that the linear AP glenoid distance can provide enough information to help the surgeon to decide on the best procedure to be done.
If anterior-inferior glenoid rim erosion is greater than 25 %, it can lead to a high recurrence rate of shoulder dislocation when only soft tissue reconstruction is performed [1, 17, 22, 23]. According to Burkhart et al., the recurrence rate of the arthroscopic Bankart repair in patients with glenoid AP erosion greater than 25 % is up to 67 %, and therefore should be treated with a bone graft procedure [24]. Montgomery et al. published an anatomical study where they created glenoid bone defects and then fixed a bone graft to restore it in several different positions. After that, they tested the intrinsic stability provided by the graft. They concluded that anterior-inferior instability of the shoulder caused by an osseous defect in the glenoid could be corrected with bone grafting [25].
Therefore, the pre-operative diagnosis is important, though intra-operative arthroscopy evaluation can give us significant information about the glenoid’s anatomy [13, 26]. However, not every surgeon performs soft-tissue reconstruction by arthroscopy. Besides, these intra-operative techniques depend on the surgeon’s experience, and they are not always reproducible [27].
In spite of the fact that 3D CT scan can determine glenoid bone loss with significant efficacy, it is more expensive than a simple radiographic study [14, 18, 28]. In addition to this, radiation exposure of the 3D CT scan is notably higher than a radiographic exam. This study has shown that the Bernageau profile view is a useful tool for evaluating the anterior rim bone loss, with similar results to the CT scan (Fig. 3a, b). In patients with glenoid AP erosion greater than 25 %, the Bernageau view rules out the possibility of arthroscopic repair even before the CT scan is obtained (Fig. 4).
Example of comparative study: Bernageau profile view versus 3D CT scan. a A-P glenoid distance calculated with Bernageau profile view of the affected side, confirming a glenoid bone loss of 23.6 %. b A-P glenoid distance calculated with Bernageau profile view of the unaffected side. c A-P glenoid distance calculated with 3D CT scan of the affected side, confirming a glenoid bone loss of 22.9 %. d A-P glenoid distance calculated with 3D CT scan of the unaffected side
We do not intend to substitute the CT scan for the Bernageau but to use the Bernageau view as a triage exam to detect glenoid bone loss. For those patients on borderline between soft-tissue repair or bone-block procedure, the CT scan should follow the Bernageau view to help in the surgical planning. Furthermore, in those patients where the Bernageau shows glenoid bone loss that needs a bone block procedure, the CT scan is also useful in confirming the size of the defect and to plan the adequate bone graft to be used (coracoid, iliac crest, or other).
Summary statement
The Bernageau radiographic view is an effective and low-cost method for evaluating glenoid bone erosion.
Conclusions
The Bernageau radiographic view is an accurate and reproducible way for measuring the presence of glenoid erosion, with similar results compared with the 3D CT scan.
References
Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–94.
Edelson JG. Bony changes of the glenoid as a consequence of shoulder instability. J Shoulder Elbow Surg. 1996;5(4):293–8.
Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–63.
Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76(12):1819–26.
Bernageau J, Patte D, Debeyre J, Ferrane J. Value of the glenoid profile in recurrent luxations of the shoulder. Rev Chir Orthop Reparatrice Appar Mot. 1976;62(2 suppl):142–7.
Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19(7):732–9.
Itoi E, Lee SB, Amrami KK, Wenger DE, An KN. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31(1):112–8.
Rockwood CA. X-ray evaluation of shoulder problems. The shoulder. Philadelphia: W.B. Saunders; 1990. p. 196–200.
Ikemoto RY, Nascimento LG, Bueno RS, Strose E, Almeida LH, Murachovsky J. The technique to calculate glenoid bone loss with the Bernageau profile view: is it possible? Tech Shoulder Elbow Surg. 2010;11(2):37–40.
Bueno RS, Ikemoto RY, Nascimento LG, Almeida LH, Strose E, Murachovsky J. Correlation of coracoid thickness and glenoid width: an anatomical morphometric analysis. Am J Sports Med. 2012. doi:10.1177/0363546512445997.
Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg. 2006;15(6):759–63.
Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg. 2001;10(4):327–32.
Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002;18(5):488–91.
Kwon YW, Powell KA, Yum JK, Brems JJ, Iannotti JP. Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elbow Surg. 2005;14(1):85–90.
Ikemoto RY, Checchia SL, Fujiki EN, Murachovsky J, Nascimento LGP. Análise das mesurações da cavidade glenoidal em peças anatômicas. Rev Bras Ortop. 2005;40(11–12):663–71.
Ikemoto RY, Nascimento LGP, Bueno RS, Strose E, Almeida LHO, Murachovsky J. Mensuração da erosão da borda anterior da glenóide através do exame radiográfico: uma forma simples de realizar a incidência de Bernageau. Rev Bras Ortop. 2010;45(6):538–42.
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A(5):878–84.
Sugaya H, Kon Y, Tsuchiya A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy. 2005;21(5):635.
Griffith JF, Antonio GE, Tong CW, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol. 2003;180(5):1423–30.
Saito H, Itoi E, Sugaya H, Minagawa H, Yamamoto N, Tuoheti Y. Location of the glenoid defect in shoulders with recurrent anterior dislocation. Am J Sports Med. 2005;33(6):889–93.
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82(1):35–46.
Carr AJ. Biomechanics of shoulder stability. Current Orthopaedics. 1996;10:146–50.
Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16.
Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23(10):1033–41.
Montgomery Jr WH, Wahl M, Hettrich C, Itoi E, Lippitt SB, Matsen 3rd FA. Anteroinferior bone-grafting can restore stability in osseous glenoid defects. J Bone Joint Surg Am. 2005;87(9):1972–7.
Lo IKY, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy. 2004;20(2):169–74.
Kralinger F, Aigner F, Longato S, Rieger M, Wambacher M. Is the bare spot a consistent landmark for shoulder arthroscopy? A study of 20 embalmed glenoids with 3-dimensional computed tomographic reconstruction. Arthroscopy. 2006;22(4):428–32.
Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24(4):376–82.
The authors have no conflicts of interest to declare and did not receive funding for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Murachovsky, J., Bueno, R.S., Nascimento, L.G.P. et al. Calculating anterior glenoid bone loss using the Bernageau profile view. Skeletal Radiol 41, 1231–1237 (2012). https://doi.org/10.1007/s00256-012-1439-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-012-1439-9