Abstract
Background
Evaluation of glenoid bone loss following recurrent anterior shoulder dislocations is normally performed using cross sectional imaging.
Objectives
To assess how anteroposterior (AP) and Bernageau view radiographs compare to computed tomography (CT), magnetic resonance imaging (MRI) and arthroscopy for evaluating glenoid bone loss in patients with recurrent anterior shoulder dislocation.
Materials and methods
A prospective observational study was performed on 32 patients over two years at a tertiary orthopedic center. The loss of sclerotic glenoid rim (LSGL) on AP radiograph and the percentage relative glenoid bone loss on the Bernageau radiograph were assessed. The percentage glenoid bone loss and anterior straight line (ASL) were calculated using a best fit en face circle method using CT and MRI. Percentage glenoid bone loss was also calculated during arthroscopy in multiples of 5%.
Results
In our study, 90.6% (29) patients were males, while only 9.4% (3) were females. This can be attributed to the involvement of the males in outdoor activities and sports. Also, the maximum number of patients were found to belong to 21–30 years of age, with the mean age being 28.66 years. Of the 32 patients, loss of sclerotic glenoid line (LSGL) on AP radiographs correlated with glenoid bone loss on cross-sectional imaging in 27 patients. Three patients had equivocal LSGL and 2 patients with glenoid bone loss on CT did not demonstrate LSGL. The difference between the two modalities was not statistically significant (p value = 0.002). The glenoid bone loss on Bernageau view correlated with glenoid bone loss on cross sectional imaging in all but one patient. The bone loss as evaluated by radiograph Bernageau view was found to have strong correlation (correlation coefficient r = 0.948, p value < 0.0001).
Conclusion
AP and Bernageau radiographic views for anterior shoulder dislocations demonstrate good correlation with glenoid bone loss on cross-sectional imaging. They may also be used as an adjunct to predict overall bone loss on CT and at arthroscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The glenohumeral joint is a ball and socket joint and accommodates the most extensive range of motion within the human body, including flexion, extension, abduction, adduction, internal, and external rotation [1]. This is made possible by the relatively shallow and small glenoid cavity as compared to a larger humeral head, but these freedoms also make the joint vulnerable to dislocation [2]. Several primary and secondary stabilizers reinforce the joint such as the glenoid labrum, glenohumeral ligaments, and rotator cuff muscles to prevent dislocation.
Injury or deficiency in these stabilizers may lead to glenohumeral instability and subsequently make individuals prone to recurrent shoulder dislocation [3, 4]. The most common type of dislocation is the anterior glenohumeral dislocation [5]. Patients with recurrent anterior dislocation may develop a mixture of soft tissue and bony Bankart lesions of the glenoid labrum as well as Hill Sach’s deformities of the humeral head. Several methods have been described to ascertain glenoid bone loss in the case of bony Bankart lesions [6, 7]. Bony restoration methods are typically undertaken if bone loss exceeds 15%, as this is the critical level at which labral repair alone is unlikely to restore glenohumeral stability or maintain a normal humeral position [8, 9].
Although 3D CT is widely regarded as an optimal imaging modality to assess glenoid bone loss, recent studies have suggested good correlation of this to evaluation with plain radiographs. This study aims to assess the role of radiography, using standard anteroposterior (AP) and Bernageau views when, compared to CT and MRI.
Ethical consideration
Ethics review committee
The Institutional Ethics Committee at author’s institute scrutinized the protocol design, tools for data collection, consent forms, and patient information sheets. The study commenced only after obtaining approval from the Ethics Committee.
Consent procedure
The Ethics Committee at author’s institute sanctioned appropriately designed consent forms for obtaining written consent. Participants were thoroughly briefed on the study’s procedure, associated risks, and requirements. Only after ensuring the participant’s full understanding and satisfaction with the procedure were they invited to sign the consent form. Additionally, each participant also signed a patient information sheet.
Participant confidentiality
Patient confidentiality was maintained to the full extent.
Materials and methods
Patient selection
A prospective observational analysis was performed over a period of 2 years of patients visiting the orthopedic clinic were included. Both male and female patients with recurrent shoulder dislocations were included. In our study, the male to female ratio was found to be 9.6:1.
Patients with bilateral shoulder dislocations and those under the age of 18 were excluded.
A total of 32 patients were evaluated.
Radiographic evaluation
Plain radiographs were obtained using anteroposterior (AP) and Bernageau views. For the AP view, the patient was made to stand erect with their back was placed against the image detector with the midcoronal plane was aligned parallel to it. The glenohumeral joint was placed in the center of the image [10]. For the Bernageau view, the patient was made to stand erect and the chest was brought into contact with the image detector at a 70° angle in order to evaluate the arm’s anterior flexion at 160°.
-
(1).
The anterior sclerotic glenoid rim was evaluated on anteroposterior (AP) radiographs. Abnormality was classified as an absence of the normal sclerotic anterior glenoid rim or discontinuity of more than 5 mm from the inferior glenoid border were regarded as abnormal and termed “loss of sclerotic glenoid line” (LSGL) (Fig. 1A) [11]. The patients were divided into three groups: (i) LSGL involving more than 50% anterior glenoid rim, (ii) LSGL involving less than 50% anterior glenoid rim, and (iii) equivocal findings. The findings were then corroborated with findings on CT scan to determine the bone loss and whether it was less or more than the critical level.
-
(2).
For the Bernageau view, the glenoid antero-posterior (AP) distance was measured in both the affected arm and the contralateral normal shoulder. The difference in AP distance between the normal and affected shoulder was calculated as a percentage to determine “glenoid percentage bone loss” (Fig. 1B, C).
A AP radiograph of a normal shoulder demonstrating the normal sclerotic anterior glenoid (arrow). Absence of this indicates the Loss of sclerotic glenoid line (LSGL) sign. B Bernageau view measuring the anteroposterior (AP) glenoid distances in a normal shoulder and C abnormal contralateral shoulder (c). Percentage of glenoid bone loss is calculated as (c-b)/c × 100
2D CT analysis
Computed tomography (CT) was performed with the patient’s affected shoulder and arm positioned against the chest wall using 64 × 0.625 collimation, 400 mA, 120 kV, 1-mm slice thickness, and 0.765 pitch, a 64-slice on a Philips Brilliance scanner. The field of view spanned from the acromion to the glenoid in cranio-caudal direction.
(1) “Percentage bone loss” was measured by obtaining two measurements. After drawing a best fit circle of the inferior two thirds of the glenoid on the sagittal reconstructed image, a line was drawn from the anterior to the posterior part of the circle and termed “diameter of inferior glenoid circle.” A second line was drawn from the anterior margin of the glenoid to the anterior part of the circle and termed “defect width.” A percentage of glenoid bone loss was calculated using the following formula: Percentage bone loss = (defect width/diameter of inferior glenoid circle) × 100%) (Fig. 2) (2). The anterior straight line was also measured on the sagittal reconstructed image utilizing a best fit circle. A line was drawn from the superior to inferior extent of the anterior glenoid (i.e., along the craniocaudal axis of the defect) [9].
A, B Normal sagittal oblique 3D computer tomography (CT) images demonstrating en face glenoid; A a best-fit circle (yellow) of the inferior 2/3rds and “diameter of inferior glenoid” (dashed arrow) and B normal curved anterior glenoid rim (arrows), absence of which leads to a positive “anterior straight line” (ASL) sign and measurement. C, D Abnormal study glenoid bone loss; C “Diameter of inferior glenoid” of 3.17 cm and second line demonstrating the “defect width” of 0.69 cm. “Glenoid percentage bone loss” is (3.17/0.69) × 100 = 13.4%. D Absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.63 cm. Measurements were done using similar technique on MRI
MRI
MRI of the affected shoulder was performed using a 3 T (GE discovery MR750) with following parameters: PDFS coronal (3-mm thick sections, TR > 1500 ms, TE = 30–50 ms), PDFS axial (3-mm thick TR = 2000–3000 ms, TE = 20–40 ms), and T1-weighted sagittal (1-mm thick TR = 600 ms, TE = 1 ms), FOV = 160 × 160 mm, and matrix size = 320 × 192.
The best-fit circle and “percentage bone loss” method described in the CT section was utilized to calculate percentage bone loss and the anterior straight line.
Arthroscopy
All patients underwent arthroscopy under general anaesthesia. The procedure involved performing arthroscopy with a 4-mm arthroscope while the patient was in the lateral decubitus posture. Using the central glenoid bare spot as a reference, the arthroscopic probe’s tip was first positioned against the posterior glenoid margin, then against the bare spot in the middle of the inferior glenoid and lastly against the anterior glenoid margin in order to measure extent of anterior glenoid bone loss (Fig. 3). The orthopedic surgeon reported arthroscopic assessments of glenoid bone loss at intervals of 5%:5%, 5–10%, 10–15%, and > 15% bone loss). These measurements were in multiples of 5% due to limitations of the orthopedic surgeon at the time of arthroscopy (Table 1).
All images of the same patient have been shown. A Anteroposterior (AP) radiograph of the right shoulder demonstrating the “loss of sclerotic line” (LSGL) sign (arrows). B, C Bernageau view radiographs of bilateral shoulders with B a “glenoid AP diameter” of 2.7 cm in the affected right shoulder and C 3.26 cm in the unaffected left shoulder; the “glenoid relative bone loss” is 17.1%. D, E Sagittal oblique proton density-fat suppressed (PD-FS) images demonstrating en face glenoid with A “diameter of inferior glenoid” of 2.56 cm and second line demonstrating the “defect width” of 0.43 cm. “Glenoid percentage bone loss” is 16.7% and C Absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.87 cm. F, G Sagittal oblique 3D computer tomography (CT) images with F a “diameter of inferior glenoid” of 3.17 cm and second line demonstrating the “defect width” of 0.69 cm “Glenoid percentage bone loss” is 21.7% and G absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.63 cm. H Arthroscopic image shows loss of the rounded anterior glenoid contour (arrows) with approximately 15% of “glenoid percentage bone loss”
Image analysis
The images were reviewed by trained senior Musculoskeletal radiologist with expertise in shoulder pathologies and over 7 years of experience.
The arthroscopic GBL measurements were provided by a senior orthopedic surgeon and head of department with expertise in shoulder and knee surgeries and over 30 years of experience.
For detecting intra-observer reproducibility, radiographic measurements were done initially by a trained senior Musculoskeletal radiologist and were subsequently repeated after 1 week. For inter-observer variability, measurements were done by junior radiologist with 1-year experience as well.
Data analysis
The Statistical Package for Social Sciences (SPSS) version 21.0 was used for analysis of data recorded on a Microsoft Excel spreadsheet. Numbers and percentages (%) were used to represent categorical data, whereas mean ± SD and median were used to represent continuous variables. The Kolmogorov–Smirnov test was used to check for data normalcy. A non-parametric test was employed if the normalcy was denied. Statistical analysis was performed with the chi-squared test for qualitative variables. The Pearson correlation and Spearman rank correlation coefficients were used to assess differences in radiographic findings of glenoid bone loss between (a) radiographic findings and arthroscopy and (b) between CT, MRI, and arthroscopy. The Bland–Altman plot was used to compare two measurement techniques and determine the 95% confidence interval (CI) limits.
Results
In our study, 90.6% (29) patients were males, while only 9.4% (3) were females. This can be attributed to the more involvement of the males in outdoor activities and sports. Also, maximum number of patients were found to belong to 21–30 years of age, with the mean age being 28.66 years.
Of the 32 patients, aged over 18 years, with a history of recurrent unilateral anterior shoulder dislocation were evaluated. The mean age was 28.66 ± 7.53 years. Five patients were less than 20 years old, 15 (47%) patients were aged between 21 to 30 years, and 12 patients were in 30–40 years age group.
The percentage bone loss was less than 15% in 22 (69%) patients on plain radiograph and CT, and 21 (56.2%) patients on MRI and arthroscopy. The mean bone loss was 14.74% ± 7.07 on CT (range 7.1 to 42.4) and 14.85 ± 7.07% (range 7.8 to 42.4%) on MRI. The mean anterior straight line (ASL) was 15.04 ± 5.12 mm (range 7.3 to 29.1 mm) on CT and 14.92 ± 5.12 (range = 7.4 to 29.5 mm) on MRI.
Of the 32 patients evaluated, On the anteroposterior (AP) radiographic view, 27 demonstrated loss of the anterior sclerotic rim line (LSGL) (Figs. 4, 5, 6, 7 and 8. In 3 patients, findings were equivocal. In 2 patients, this could not be radiographically appreciated despite there being glenoid bone loss of 8 and 8.5% respectively as evaluated by CT (Fig. 6). Of the 27 patients with LSGL, 16 demonstrated less than 50% interruption and 11 demonstrated more than 50% interruption of the anterior sclerotic glenoid line. CT was used as the gold standard for the assessment of glenoid bone loss. Comparative analysis revealed that in patients with less than 50% LSGL, 87.5% showed < 15% loss on CT; the other 12.5% had ≥ 15% bone loss on CT. The difference between the two modalities was not statistically significant (p value = 0.002). In all patients with > 50% interruption of the anterior glenoid rim on radiograph, CT revealed > 15% bone loss .
All images of the same patient have been shown). A Anteroposterior (AP) radiograph of the right shoulder demonstrating the “loss of sclerotic line” (LSGL) sign (arrows) > 50%. B, C Bernageau view radiographs of bilateral shoulders with B a “glenoid AP diameter” of 2.18 cm in the affected right shoulder and C 3.08 cm in the unaffected left shoulder; the “glenoid relative bone loss” is 28%. D, E Sagittal oblique proton density-fat suppressed (PD-FS) images demonstrating en face glenoid with “diameter of inferior glenoid” of 2.56 cm and second line demonstrating the “defect width” of 1.07 cm. “Glenoid percentage bone loss” is 42.4% and Absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 2.95 cm. F CT 3D reconstruction of the same patient demonstrating a large bony Bankart from 2 o’ clock to 6 o’ clock position. G, H Sagittal oblique 3D computer tomography (CT) images with F a “diameter of inferior glenoid” of 2.67 cm and second line demonstrating the “defect width” of 1.11 “Glenoid percentage bone loss” is 41.8% and G absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 2.91 cm. I Arthroscopic image show loss of the rounded anterior glenoid contour (arrows) with approximately 30% of “glenoid percentage bone loss”
All images of the same patient have been shown. A Anteroposterior (AP) radiograph of the right shoulder demonstrating the “loss of sclerotic line” (LSGL) sign (arrows) < 50%. B, C Bernageau view radiographs of bilateral shoulders with B a “glenoid AP diameter” of 2.56 cm in the affected right shoulder and C 2.93 cm in the unaffected left shoulder; the “glenoid relative bone loss” is 12.6%. D, E Sagittal oblique proton density-fat suppressed (PD-FS) images demonstrating en face glenoid with “diameter of inferior glenoid” of 2.78 cm and second line demonstrating the “defect width” of 0.30 cm. “Glenoid percentage bone loss” is 11.1% and Absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.49 cm. F, G Sagittal oblique 3D computer tomography (CT) images with F a “diameter of inferior glenoid” of 2.62 cm and second line demonstrating the “defect width” of 0.35 “Glenoid percentage bone loss” is 13.3% and G absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.77 cm
All images of the same patient have been shown). A AP radiograph of the left shoulder shows a relatively preserved sclerotic rim though MRI/CT showed a bone loss. Thus, the intact sclerotic glenoid rim does not rule out bone loss. B, C In the same patient, Bernageau view radiographs of bilateral shoulders with B “glenoid AP diameter” of 3.36 cm in the affected left shoulder and C 3.64 cm in the unaffected right shoulder; the “glenoid relative bone loss” is 7.7%. D, E Sagittal oblique proton density-fat suppressed (PD-FS) images demonstrating en face glenoid with “diameter of inferior glenoid” of 2.76 cm and second line demonstrating the “defect width” of 0.21 cm. “Glenoid percentage bone loss” is 7.6% and absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 0.85 cm. F, G Sagittal oblique 3D computer tomography (CT) images with F a “diameter of inferior glenoid” of 2.81 cm and second line demonstrating the “defect width” of 0.26 “glenoid percentage bone loss” is 9.2% and G absence of the normal curved anterior glenoid rim with a positive “anterior straight line” (ASL) sign measuring 1.09 cm. H, I Arthroscopic image shows subtle loss of the rounded anterior glenoid contour (arrows) with minimal bone loss
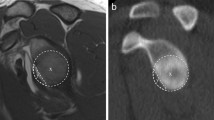
A AP radiograph of the left shoulder shows sclerosis of the postero-lateral aspect of the humeral head suggestive of Hill Sach’s lesion. B Axial sections of CT at the level of the gleno-humeral joint show a wedge-shaped defect involving the postero-lateral humeral head. C Axial sections of the PDFS MRI sequence show a wedge-shaped defect involving the postero-lateral aspect of the humeral head with bone marrow edema consistent with Hill Sach’s lesion
A strong correlation was also found between the percentage of glenoid bone loss measured using the Bernageau view and MRI (correlation coefficient r: 0.941, p < 0.0001). Radiograph and arthroscopy correlation also revealed similar results (correlation coefficient r 0.883, p < 0.0001).
Percentage glenoid bone loss on CT demonstrated a significant correlation when compared to MRI (r 0.986, p < 0.0001). There was also a significant correlation between both the modalities for the anterior straight line (r = 0.987, p value < 0.0001) as well. No significant difference was found between glenoid bone loss between CT and MRI with assessment by the Bland–Altman plot.
Percentage glenoid bone loss on CT showed a significant correlation with arthroscopy (r = 0.92, p value < 0.0001). MRI also demonstrated a significant correlation with arthroscopy (r = 0.915, p value < 0.0001).
To assess measurement consistency, we calculated inter-observer and intra-observer reliability using the Intraclass Correlation Coefficient (ICC). The analysis yielded excellent results, with an ICC of 0.98 (95% CI: [0.87, 0.99]) for interobserver reliability and 0.99 (95% CI: [0.98, 1.00]) for intra-observer reliability. These high ICC values, both exceeding 0.90, indicate excellent consistency between the two observers and across time for individual observer. These findings demonstrate the high reliability of our measurement process, strengthening the validity of subsequent analyses and conclusions drawn from this data.
Discussion
Preoperative assessment of glenoid bone loss is important in patients with recurrent shoulder dislocation. Bone loss can be reliably assessed on AP and Bernageau view radiographs.
In our study, there was a strong correlation between Radiograph Bernageau view and CT in the evaluation of the glenoid bone loss. Moreover, radiograph AP view also has an important role to play since the loss of sclerotic line sign is quite useful to determine clinically significant bone loss.
Thus, radiograph is a useful modality which may or may not be supplemented by another imaging modality. AP and Bernageau views were specifically used in our study as these are known radiographic techniques for the evaluation of glenoid bone loss and are currently in practise in the orthopedics department of our hospital.
There are other shoulder radiographs such as Grashey’s view west point and axillary views. The Grashey view is a true AP view of the shoulder joint and allows for better evaluation of the glenohumeral cartilage space, joint congruity, and humeral head subluxation. This view is great to inspect the joint space for subtle fractures such as a Bankart lesion post-dislocation-relocation. However, disadvantage of this view in instability cases is that subtle abnormalities, such as nondisplaced Bankart fractures, can be missed due to anterior and posterior glenoid rim overlap.
AP radiograph is useful for glenoid bone loss assessment that is seen as loss of sclerotic glenoid line which is useful for evaluation of glenoid bone loss and is used routinely in our hospital. Bernageau view allows accurate quantitative estimation of the glenoid bone loss, however has its limitations as it is difficult to obtain this view.
Out of 32 patients of anterior shoulder instability, maximum number of patients 15 (46.88%) were found to belong to 21–30 years of age, with the mean age being ~ 28.66 ± 7.53 years. In their research, Mehmet Tas et al. discovered that individuals with recurrent disorder belonged to lesser age group compared to those with single time dislocation, with a mean age of 29.7 ± 14.5 years. The elevated risk of recurrence among younger patients poses a significant challenge, a viewpoint also supported by Rhee et al., who reported a mean ~ 25 years, range varying from 14 to 47 years [12].
Out of 32, 29 (90.62%) included males while only 3 (9.38%) were females. This can be attributed to increased involvement of males in outdoor activities and sports. In the study by Rhee et al. [13] on 246 patients, 214 patients were males, while 24 were found to be females, i.e., only 9.75% patients were females.
Overall, the GBL percentage was found to be less than 15% in majority patients by all imaging modalities.
Although 3-D CT is widely regarded as the optimal imaging technique for assessing glenoid bone loss in individuals with recurrent shoulder dislocations [14, 15], Lee et al. demonstrated a good correlation between the radiographic parameters of the anterior straight line length, glenoid width, and the degree of glenoid bone loss, with MRI and CT, especially when the best-fit circle width approach was applied [16, 17]. Several other recent studies have suggested radiography as a tool showing good correlation with CT in assessing glenoid bone loss [18].
Overall, the percentage of glenoid bone loss was found to be less than 15% in the majority of our patients by all imaging modalities. Similar results were documented in study conducted by Bhatia S et al., in which a significant proportion of patients exhibited mild or moderate bone loss [19]. Similarly, Griffith et al. documented that out of 145, 74 (51%) patients had glenoid bone loss of10% or less, 54 (37%) between 10 and 20%, and 17 (31%) had more than 20% glenoid bone loss [20].
Loss of the anterior sclerotic glenoid rim line (ASGL) reflected deficiency of the anterior bony glenoid. In our study, this could not be appreciated in 2 patients despite there being bone loss of 8% and 8.5% respectively on the follow-up CT scan. This suggests that the detection of small glenoid bone defects may be missed using this method alone. However, when present, all patients demonstrated bone loss on CT. This supports findings from Jankauskas et al. who compared the LSGL sign on AP radiographs with CT images and concluded that LSGL is moderately sensitive and highly specific for the detection of anterior osseous lesions [21]. In a clinical setting, where the anterior sclerotic glenoid rim is deficient, this is an overall good predictor for a glenoid defect. We also found that the percentage interruption of the anterior sclerotic rim on AP radiograph correlated with percentage bone loss on CT. This suggests that the degree of loss of the LSGL can be useful in predicting whether the glenoid bone loss is beyond 15% or otherwise and thus can help in triaging patients who are likely to require further cross sectional imaging (and/or surgery) and those that can be managed conservatively, respectively. We could not identify any studies correlating the extent of LSGL with glenoid bone loss on CT and this represents an area of future study.
The percentage glenoid bone loss on the Bernageau radiographic view demonstrated good correlation with 2D CT findings in all but one patient. In this patient, there was 28% loss on Bernageau view compared to 42.4% on CT. This suggests that in cases with severe bone loss, particularly in post-traumatic cases, radiographs may not fully appreciate the extend of glenoid bone loss. It may be explained by a more accurate assessment of the glenoid’s inferior width on CT as compared to radiograph [22]. Muracovsky et al. [18] have also reported differences between the percentages of bone loss on the radiograph when compared with 3D CT which was on average 2.28% (range 0 to 6.05%). Overall, the Bernageau radiographic view remains an accurate and reproducible way for assessing glenoid loss with similar results compared to 2D CT scan. Although we identified no prior studies which compared glenoid bone loss on radiograph against MRI or arthroscopy, our analysis demonstrates that there is no significant difference.
Comparative analysis of both glenoid percentage bone loss and the anterior straight line (ASL) between CT and MRI showed very good correlation. These findings closely mirror those Lee et al. (12), wherein the anterior straight line length measured by MRI imaging (mean = 12 mm ± 8.4) and CT (mean = 11.8 mm ± 8.3) exhibited robust correlation, with an r value of 0.97 and a p-value of less than 0.0001. Furthermore, similar results on glenoid bone loss, using a best-fit circle method, were observed by Yanke et al. and Tian et al. who reported a statistically significant correlation between the two imaging modalities [23]. Glenoid bone loss on 2D CT and MRI compared to that observed during arthroscopy demonstrated a significant correlation and this has also been reported by previous authors [16].
Thus, despite the abovementioned role of radiographs in glenoid bone loss assessment, there are a few limitations too. As mentioned previously, it may be difficult to identify small glenoid bone defects on radiographs. Hill Sach’s lesion cannot be measured on radiographs. The evaluation of on track and off lesions is important in deciding operative management of patients with recurrent shoulder dislocation. However, this is possible only using cross-sectional imaging (CT/MRI) and cannot be done using radiography alone. This hence highlights the limitation of radiography which can be used as screening tool in deciding which patients could be taken up for CT/MRI to help plan surgical management of patients with recurrent shoulder dislocation.
This study mainly focusses on the available imaging modalities and comparison between them to decide role of each imaging modality as well tailoring the use of modalities according to individual patient needs.
One of the limitations of our study was that the sample size is relatively small.
Conclusion
This study demonstrates that radiographic findings in patients with recurrent shoulder dislocation have a good correlation with follow-up cross-sectional imaging and arthroscopic findings. The extent of LSGL on AP radiographs may be used to predict the extent of bone loss and therefore may have a role in determining whether a patient should have further imaging or be managed conservatively. Bernageau view radiograph is also quite accurate method for determining the glenoid bone loss. CT and MRI perform equally where assessing glenoid bone loss and correlate well to appearances on final arthroscopy. However, small glenoid bone loss may be difficult to assess on plain radiographs.
References
Kammel KR, Leber EH. Dislocation, Shoulder (Humerus), Posterior. In: StatPearls. StatPearls Publishing; Treasure Island (FL); 2018.
Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–17.
Mclaughlin HL, Cavallaro WU. Primary anterior dislocation of the shoulder. Am J Surg. 1950;80:615–21.
Simonet WT, Cofield RH. Prognosis in anterior shoulder dislocation. Am J Sports Med. 1984;12:19–24.
Cotman SJ, Trinh TQ, Vincent S, Backes JR. Proximal humerus fracture-dislocation with laceration of the axillary artery: a case report. Iowa Orthop J. 2017;37:53–5.
Ho AG, Gowda AL, Wiater JM. Evaluation and treatment of failed shoulder instability procedures. J Orthop Traumatol. 2016;17:187–97.
Bankart AS. Recurrent or habitual dislocation of the shoulder-joint. Br Med J. 1923;2:1132–3.
Shin SJ, Koh YW, Bui C. What is the critical value of glenoid bone loss at which soft tissue Bankart repair does not restore glenohumeral translation, restricts range of motion, and leads to abnormal humeral head position? Am J Sports Med. 2016;44:2784–91.
Skendzel JG, Sekiya JK. Diagnosis and management of humeral head bone loss in shoulder instability. Am J Sports Med. 2012;40:2633–44.
Whitley S. Upper Limb. In: Whitley S, Jefferson G, Holmes K, Sloane C, Anderson C, Hoadley G, editors. Clark’s positioning in radiography. 13th ed. London: CRC Press; 2016. p. 53–5.
Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791–6.
Tas M, Canbora MK, Kose O, Egerci OF, Gem M. Demographic and clinical characteristics of traumatic shoulder dislocations in an urban city of Turkey: a retrospective analysis of 208 cases. Acta Orthop Traumatol Turc. 2013;47(3):147–52.
Hamamoto JT, Leroux T, Chahla J. Assessment and evaluation of glenoid bone loss. Arthrosc Tech. 2016;5:e947–51.
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85:878–84.
Stevens KJ, Preston BJ, Wallace WA, Kerslake RW. CT imaging and three-dimensional reconstructions of shoulders with anterior glenohumeral instability. Clin Anat. 1999;12(5):326–36.
Lee RKL, Griffith JF, Tong MMP, Sharma N, Yung P. Glenoid bone loss: assessment with MRI imaging. Radiology. 2013;267:496–502.
Gyftopoulos S, Hasan S, Bencardino J, Mayo J, Nayyar S, Babb J. Diagnostic accuracy of MRI in the measurement of glenoid bone loss. Am J Roentgenol. 2012;199(4):873–8.
Murachovsky J, Bueno RS, Nascimento LG, Almeida LH, Strose E, Castiglia MT, de Oliveira HC, Ikemoto RY. Calculating anterior glenoid bone loss using the Bernageau profile view. Skeletal Radiol. 2012;41:1231–7.
Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB, LeClere L, Romeo AA. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92:133–51.
Yanke AB, Shin JJ, Pearson I, Bach BR Jr, Romeo AA, Cole BJ, Verma NN. Three-dimensional magnetic resonance imaging quantification of glenoid bone loss is equivalent to 3-dimensional computed tomography quantification: cadaveric study. Arthroscopy. 2017;33(4):709–15.
Skupiński J, Piechota MZ, Wawrzynek W, Maczuch J, Babińska A. The bony Bankart lesion: how to measure the glenoid bone loss. Pol J Radiol. 2017;82:58–63.
Charousset C, Beauthier V, Bellaïche L, Guillin R, Brassart N, Thomazeau H. Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop Trauma Surg Res. 2010;96:S88-93.
Tian CY, Shang Y, Zheng ZZ. Glenoid bone lesions: Comparison between 3D VIBE images in MRI arthrography and nonarthrographic MSCT. J Magnet Reson Imaging. 2012;36(1):231–6.
Acknowledgements
We would like to acknowledge the help of Mr. Aniket Aman Data Science Fellow Max Super Speciality hospital, Saket, New Delhi, India with statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lohiya, N., Hussein, M., Sahu, A.K. et al. Assessing the current role of AP and Bernageau view radiographs in measurement of glenoid bone loss in patients with recurrent shoulder dislocation: correlation with computed tomography, magnetic resonance imaging, and arthroscopy. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04797-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04797-y