Abstract
Purpose
To investigate the diagnostic efficacy of morphological sequences at 3.0 T MR imaging in detecting anterior cruciate ligament (ACL), meniscal pathology and traumatic cartilage legions in young patients with chronic deficient anterior cruciate ligament knees.
Methods and materials
This prospective study included 43 patients (39 male) between the age of 15 and 37 years (mean age 22.6 years) with a history of knee injury sustained at least 3 months prior to the decision to repair a torn ACL. All patients underwent a 3.0 T MR scan with the same standard protocol, including intermediate-weighted and three-dimensional spoiled gradient-recalled T1-weighted sequences with fat saturation and subsequently surgical reconstruction of the ACL, along with meniscal and cartilage repair, when necessary.
Results
All ACL tears were correctly interpreted by 3.0 T MR images. The sensitivity of the MR scans regarding tears of the medial meniscus was 93.7%, the specificity 92.6%, the positive predictive value 88.2% and the negative predictive value 95.8%. The sensitivity of the MR scans regarding tears of lateral meniscus was 85.7%, the specificity was 93.1%, the positive predictive value 85.7% and the negative predictive value 93.1%. With regard to the grading of the cartilage lesions, Cohen’s kappa coefficient indicated moderate agreement for grade I and II cartilage lesions (0.5), substantial agreement for grade III and IV cartilage lesions (0.70 and 0.66) and substantial agreement for normal regions (0.75). Regarding location of the cartilage lesions, Cohen’s kappa coefficient varied between almost perfect agreement in the lateral femoral condyle and no agreement in the trochlea.
Conclusion
In the setting of chronic ACL deficiency, MR imaging at 3.0 T achieves satisfactory diagnostic performance regarding meniscal and ligamentous pathology. In the detection of cartilage lesions MRI is less successful.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injuries are relatively common among young adults with moderate to advanced physical activity [1, 2]. ACL tears, either partial or complete, may be accompanied by meniscal tears and traumatic chondral lesions [3–6]. The latter group of lesions is related to an increased risk of developing early joint degeneration, although this process seems to be multifactorial, especially in chronic ACL-deficient knees [7].
Magnetic resonance imaging is the non-invasive imaging modality of choice for preoperative assessment of knee structures [8–10], and the diagnostic efficacy of this method regarding ACL and meniscal tears has been explored extensively in the literature [4, 11–15]. The diagnostic performance of MRI with 1.0 T and 1.5 T scanners regarding detection and grading of traumatic cartilage defects has been controversial [15–17]. It has been reported that at the above field strengths, the diagnostic performance of MRI is considered adequate in detecting advanced cartilage defects, whereas it is less effective in the early detection of low-grade cartilage lesions [18]. The advent of 3.0 T MRI in clinical practice with the well-established advantages of increased signal-to-noise ratio (SNR) has introduced new standards of imaging. Therefore, the diagnostic performance at 3.0 T regarding knee and cartilage pathology has been revisited [19–21].
The purpose of the present study was to determine the diagnostic efficacy of routine morphological sequences including intermediate-weighted and three-dimensional spoiled gradient-recalled (3D-SPGR) T1-weighted sequences with fat saturation with 3.0 T MRI in detecting meniscal and anterior cruciate ligament pathology and in assessing and classifying traumatic cartilage defects among patients with chronic ACL deficiency. The diagnostic performance of MRI was compared with that of arthroscopy, which was used as the standard of reference.
Materials and methods
This prospective study included 43 patients (22.58 ± 6.15 years; range 15–37 years) of which 39 were male (23.33 ± 5.97 years; range 15–37 years and 4 were female (15.25 ± 0.43 years; range 15–16 years). All of them attended the Orthopaedic Department of our Hospital for the surgical management of a deficient ACL over a one-and-half-year period (April 2008 to November 2009). All patients had a history of knee injury of between 3 to 12 months prior to arthroscopy and were therefore classified as having chronic injury.
The inclusion criteria were:
-
1.
Rupture of the ACL in the affected knee with positive clinical evaluation
-
2.
No previous knee surgery
-
3.
No other ligamentous injury of the knee
-
4.
Patient’s agreement to undergo a preoperative MRI of their operated knee 24–48 h before surgery
Exclusion criteria from the present study included inability to perform an MRI (e.g. metal implants or retained metal fragments). Informed consent was obtained from all participating patients and the study was approved by the institutional review board.
Magnetic resonance imaging
All MRI were performed in a 3.0 T scanner (GE; Signa HDx Healthcare) with a quadrature knee coil. The protocol used for detection of ligamentous pathology, meniscal tears and cartilage lesions included axial (TR/TE 2,500/32, 18-cm FOV, 4-mm slice thickness), coronal (TR/TE 1,800/32, 18-cm FOV, 3-mm slice thickness) and sagittal (TR/TE 2,300/32, 18-cm FOV, 2-mm slice thickness) proton density-weighted fast spin echo sequences with fat saturation, coronal T1-weighted (TR/TE 500/8, 18-cm FOV, 3-mm slice thickness) fast spin echo sequence and 3D-SPGR) T1-weighted sequence (TR/TE 12/2.5, 18-cm FOV, 1-mm slice thickness) with fat saturation. The total scanning time was approximately 35 min.
All MRI examinations were reviewed by a trained musculoskeletal radiologist with 6 years’ experience in MR imaging for the presence of ligamentous pathology, meniscal tears and cartilage lesions. The status of the ACL was assessed as being intact, completely torn or partially torn. The coexistence of meniscal tears was recorded and classified by location and morphology. Location was described by the meniscal radial anatomical section involved, using the terms anterior horn, body, or posterior horn, and combinations of these terms. Tear morphology was described by common terms accepted in the radiological and orthopaedic literature and included bucket handle, horizontal, complex, vertical and degenerative tears. Concomitant pivot-shift bone marrow contusions were also recorded. To evaluate intra-observer variability, a subset of 10 random scans was assigned evaluation a second time after 1–2 weeks by the radiologist who performed the initial assessment.
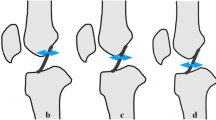
The articular surfaces of the knee were divided into six regions: patella, trochlea, medial femoral condyle, medial tibial condyle, lateral femoral condyle and lateral tibial condyle. MR grading of the cartilage lesions was based on the International Cartilage Repair Society classification for traumatic cartilage lesions and compared directly with arthroscopic findings as defined by the Outerbridge classification [22]. Normal cartilage was scored as grade 0 and the threshold of 50% was used for MR evaluation as follows: grade I for superficial lesions such as fissures and cracks, grade II for lesions extending down to <50% of cartilage depth, grade III for defects extending down >50% of cartilage depth and grade IV for full-thickness lesions with subchondral bone exposure. Arthroscopic findings were considered to be the standard of reference. A total of 258 articular surfaces were assessed by both methods in order to detect the presence or absence of a cartilage lesion and to classify the lesion correctly.
Surgical technique
General or spinal anaesthesia was used in all patients. Standard arthroscopic portals including an anterolateral and an anteromedial portal were used in all cases. A thorough evaluation of the joint was performed in every case using the anterolateral portal as a viewing portal and the anteromedial (using a probe) as a working portal.
The ACL was classified after arthroscopic probing as intact, completely torn or partially torn (when an isolated rupture of the anteromedial or the posterolateral bundle was identified). Both menisci were carefully examined using the probe and tears (if present) were classified as vertical, bucket handle, horizontal, complex and degenerative. In addition, tear location, tear length and rim width were recorded at the time of surgery. Finally, the status of the articular cartilage of the patella, trochlea, medial femoral condyle, medial tibial condyle, lateral femoral condyle and lateral tibial condyle were recorded and classified using the Outerbridge system [22]. After diagnostic arthroscopy an arthroscopy-assisted ACL reconstruction was subsequently performed and meniscal and cartilage injuries were treated as indicated. The orthopaedic surgical team was aware of the MR findings for the patients’ benefit. The orthopaedic team consisted of three surgeons (M.H., S.M. and K.M.), with 15, 4 and 25 years’ experience in knee arthroscopy, respectively.
Statistical analysis
The diagnostic values of sensitivity, accuracy and positive and negative predictive values were calculated for detecting meniscal pathology. To determine consistency among MR findings and arthroscopy in detecting loci and grading of cartilage lesions, we used the unweighted κ statistic. Grading statistics were estimated on a per region basis whereas loci statistics were estimated on a per lesion basis.
The κ statistic is commonly used to examine rater agreement, but it has also been used to compare classification methods [23, 24]. It compares the probability of agreement, PA, with that being expected, PE, if the ratings were not associated, and is given by
All statistical indices were calculated using the R Project for Statistical Computing [25]. Kappa values were calculated using the vcd package (http://cran.r-project.org/web/packages/vcd/index.html).
Results
Our study group consisted of young patients who had previously sustained knee injury and subsequent ACL deficiency. The aetiology of ACL tear was either a sport injury during occasional weekend activity or a fall. The mean duration time between the injury and the arthroscopic repair was 19.6 months, which was consistent with chronic ACL tear.
Magnetic resonance imaging correctly detected ACL tear in all 43 patients. It found 2 cases of partial ACL tears, which were also confirmed arthroscopically. None of the patients in our study group was found to have a tear of the posterior cruciate ligament.
Regarding meniscal lesions, MRI detected 17 tears involving the medial meniscus (39.5%) and 14 tears involving the lateral meniscus (32.6%). Based on MR findings, 26 medial menisci (60.5%) and 29 lateral menisci (67.4%) were found to be normal. The sensitivity, specificity and positive and negative predictive values for detecting tears of the medial meniscus on 3.0 T MR scans were 93.7%, 92.6%, 88.2%, and 95.8% respectively. The sensitivity, specificity and positive and negative predictive value for detecting tears of the lateral meniscus on 3.0 T MR scans were 85.7%, 93.1%, 85.7% and 93.1% respectively (Table 1).
Magnetic resonance scans demonstrated correctly all but one case of bucket handle tears in both menisci and all vertical tears in the medial meniscus. The number of vertical tears of the lateral meniscus was overestimated; therefore, 7 cases (50%) were interpreted as such and only 3 (21.4%) were confirmed arthroscopically. Horizontal and complex tears were the most commonly acquired ruptures of both menisci, and MRI classified correctly all cases of medial and only 5 cases (50%) of lateral tears (Table 2). The overall sensitivity, specificity and positive and negative predictive values of meniscal tears on 3.0 T MR scans were found to be 90%, 92.9%, 87.1% and 94.5% respectively (Table 1).
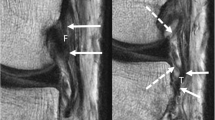
With respect to the integrity of articular cartilage, 3.0 T MR imaging demonstrated 26 traumatic cartilage lesions of various grades among 23 patients (53.4%) and 20 patients (46.5%) with normal articular cartilage. Arthroscopy found that 20 patients (46.5%) had normal articular knee cartilage in the setting of chronic ACL injury, whereas 23 patients (53.4%) were found to have 35 cartilage lesions (Tables 3, 4) (Figs. 1, 2, 3, 4 and 5).
Cohen’s kappa coefficient was calculated in order to quantify the agreement between MR imaging and arthroscopy. Our results (Table 5) showed that the two methods displayed moderate (grade I and grade II) to substantial agreement (grade III and grade IV) as far as grading was concerned. Grade IV defects also displayed the greatest variation found, since our data included only one patient with grade IV lesions. Also, both MRI and arthroscopy agreed on 222 normal articular surfaces, namely without chondral defects (sensitivity 65%, specificity 99%). Overall, a kappa coefficient of 0.75 ± 0.06 was calculated, also showing substantial grading agreement. Our results regarding the location of cartilage lesions indicated a substantial variation between complete disagreement in the femoral trochlea region to perfect agreement in the lateral femoral condyle region. Patella cartilage results displayed substantial agreement with 2 positive lesions (sensitivity 50%, specificity 100%) and MFC showed almost perfect agreement with only 3 lesions classified as normal (sensitivity 78%, specificity 100%).
Intra-observer variability of MR imaging assessment was almost excellent (κ = 0.81) with an interval of 1–2 weeks between the two assessments. The findings of arthroscopy were evaluated only once by the orthopaedic team in consensus.
Discussion
Tears of the ACL have been reported to occur in combination with meniscal tears and traumatic cartilage lesions [1, 5, 6, 26]. The incidence of severe articular cartilage injury in acute ACL tears has been reported to vary between 16 and 46% [3], whereas the time from ACL to arthroscopy was positively correlated with more advanced degenerative changes and the presence of meniscal tears was associated with a greater degree of articular damage [6, 27]. The preoperative assessment using MR imaging for detection of meniscal and cartilaginous pathology in patients with chronic ACL tears is therefore important and aids pre-treatment planning.
Our results suggest that MR imaging at 3.0 T is excellent at detecting ACL tears, as it correctly detected all 41 cases with a complete and 2 cases with a partial tear of ACL in our study group. The above results are in agreement with other studies [14, 15, 19] regarding complete ACL tears. However, detection of partial ACL tears by MR imaging could be difficult, and the number of cases that were included in our study group is not sufficient to provide a statistically significant result.
The sensitivity and specificity of 3.0 T MR imaging regarding the classification of type and location of meniscal tears may be considered satisfactory, with an overall positive and negative predictive value of 87.1% and 94.5% respectively. The detection of medial meniscal tears was better than that of lateral meniscal tears with sensitivities of 93.7% and 85.7% respectively. These findings are in agreement with previous published data that reported that tears of the posterior horn of the lateral meniscus are more prone to misdiagnosis as normal in patients with ACL tears [11]. Our data show slightly better performance compared with recently published results regarding detection of lateral meniscal tears by the use of three-dimensional IDEAL GRASS sequences at 3.0 T [28].
It has been reported that in patients with chronic deficient ACL, the most common meniscal tear occurs medially and the most common morphological type of tear is complex [12, 29]. The overall sensitivity and specificity in chronic ACL-deficient knees on MRI has been reported to be as high as 90% and 89% respectively for 1.5 T MR images [12] and these percentages are similar to our findings for 3.0 T images, namely 89.7% and 89.5% respectively. Sampson et al. [14] found that sensitivity for the overall detection of meniscal tears in their study at 3.0 T was 84% and specificity was 93%. However, other studies found that MR studies at 1.5 T were less accurate in detecting ACL and meniscal tears, with overall reported accuracies of 91% for ACL, 68% for medial meniscus and 86% lateral meniscus [15]. Rayan et al. [13], have also suggested that clinical examination performs better than MR imaging in detecting ACL and meniscal pathology and that MR studies should be performed on the basis of excluding serious underlying pathology.
Based on our results, we would suggest that the advent of 3.0 T MR imaging in routine clinical practice might contribute to more accurate and effective diagnosis of ACL and meniscal pathology, with fewer controversial findings reported due to a higher standard of image quality that allows more confident diagnosis. Even in equivocal cases, on 3.0 T images [30], a descriptive approach in reporting subtle findings such as a possible tear on just one image has been reported to increase the specificity up to 91% and 93% for the medial and lateral meniscus respectively.
The performance of MR imaging regarding cartilage lesions, which are expected to occur in patients with deficient ACL, is less effective compared with meniscal and ligmanetous pathology. It has been reported that 3.0 T MR imaging performs better than 1.5 T MR imaging [31, 32]; however, this is controversial since other reports suggest that only grade III and IV cartilage lesions could be reliably detected [20].
Kijowski et al. [33] found that 3.0 T MR imaging showed significantly higher specificity and accuracy, but not higher sensitivity in detecting cartilage lesions, compared with 1.5 T, when a routine imaging protocol was applied for detection of early cartilage defects, and therefore the implementation of dedicated sequences for cartilage imaging might be necessary.
Based on our findings, it could be suggested that grade I and II cartilage lesions are still a diagnostic challenge, since it is possible that they could be missed (Cohen’s kappa coefficient was 0.5 ± 0.14 and 0.5 ± 0.16 for grade I and II lesions respectively). The more advanced the cartilage lesion, the more reliable the imaging findings, with agreement between imaging and arthroscopy expressed as Cohen’s kappa coefficient 0.7 ± 0.14 and 0.66 ± 0.33 for grades III and IV respectively. In our dataset, we had a very limited number of grade IV cartilage lesions, and therefore this may explain the better performance of 3.0 T MR imaging in grade III than in grade IV lesions.
The MR results are better and more promising with regard to the detection of the location of a cartilage lesion. We observed a slight variation between lateral and medial femoral condyle lesions, since both arthroscopy and MRI demonstrated agreement of 0.81 ± 0.10 and 0.78 ± 0.21 respectively, whereas there was no correct detection of trochlear lesions at all because MR scans failed to detect all three lesions present. The retrospective review of MR images after arthroscopy in those patients with trochlear lesions did not alter the initial negative diagnosis for chondral defects. Our findings disagree with previous reported results that MRI allows reliable grading of isolated injury to the trochlear groove cartilage [26]. A possible explanation may be attributed to the anatomy of the area, which could hide small cartilage defects and make them invisible even in 3D-SPGR images with zero spacing between slices.
Wong et al. [21] reported that a comparison between 1.5 and 3 T MR images with arthroscopy as the gold standard led to improved diagnosis of cartilage abnormalities at 3.0 T with greater sensitivity (75.7% versus 70.6%) and accuracy (88.2% versus 86.4%) and correct grading of cartilage lesions (51.3% versus 42.9%). Other studies [20, 27] suggest that the value of arthroscopy might be irreplaceable in detecting cartilage lesions even by the use of 3.0 T MR studies, and although the initial studies show a clear precedence of arthroscopy over MRI, the development of new sequences may eventually lead to a more confident non-invasive classification of cartilage lesions. Such attempts have already been reported in the literature [34–37] with results that need to be further evaluated.
Conclusion
In the setting of chronic ACL deficiency, MR imaging at 3.0 T achieves satisfactory diagnostic performance with regard to meniscal and ligamentous pathology. In the detection of cartilage lesions MRI is less successful.
References
Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262–70.
Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies. Knee. 2007;14:177–82.
Brophy RH, Zeltser D, Wright RW, Flanigan D. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy. 2010;26:112–20.
Frobell RB, Le Graverand MP, Buck R, Roos EM, Roos HP, Tamez-Pena J, et al. The acutely ACL injured knee assessed by MRI: changes in joint fluid, bone marrow lesions, and cartilage during the first year. Osteoarthritis Cartilage. 2009;17:161–7.
Jee WH, McCauley TR, Kim JM. Magnetic resonance diagnosis of meniscal tears in patients with acute anterior cruciate ligament tears. J Comput Assist Tomogr. 2004;28:402–6.
Maffulli N, Binfield PM, King JB. Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy. 2003;19:685–90.
Amin S, Guermazi A, Lavalley MP, Niu J, Clancy M, Hunter DJ, et al. Complete anterior cruciate ligament tear and the risk for cartilage loss and progression of symptoms in men and women with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:897–902.
Galea A, Giuffre B, Dimmick S, Coolican MR, Parker DA. The accuracy of magnetic resonance imaging scanning and its influence on management decisions in knee surgery. Arthroscopy. 2009;25:473–80.
Li XM, Peng WJ, Wu H, Kacher D, Xia LM, Ai F, et al. MRI findings in injured articular cartilage of the knee correlated with surgical findings. Chin Med J (Engl). 2009;122:2624–30.
Oei EH, Ginai AZ, Hunink MG. MRI for traumatic knee injury: a review. Semin Ultrasound CT MR. 2007;28:141–57.
Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol. 2009;193:515–23.
Naranje S, Mittal R, Nag H, Sharma R. Arthroscopic and magnetic resonance imaging evaluation of meniscus lesions in the chronic anterior cruciate ligament-deficient knee. Arthroscopy. 2008;24:1045–51.
Rayan F, Bhonsle S, Shukla DD. Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. Int Orthop. 2009;33:129–32.
Sampson MJ, Jackson MP, Moran CJ, Shine S, Moran R, Eustace SJ. Three Tesla MRI for the diagnosis of meniscal and anterior cruciate ligament pathology: a comparison to arthroscopic findings. Clin Radiol. 2008;63:1106–11.
Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc. 2007;15:533–6.
Recht MP, Goodwin DW, Winalski CS, White LM. MRI of articular cartilage: revisiting current status and future directions. AJR Am J Roentgenol. 2005;185:899–914.
Trattnig S. Overuse of hyaline cartilage and imaging. Eur J Radiol. 1997;25:188–98.
Winalski CS, Gupta KB. Magnetic resonance imaging of focal articular cartilage lesions. Top Magn Reson Imaging. 2003;14:131–44.
Craig JG, Go L, Blechinger J, Hearshen D, Bouffard JA, Diamond M, et al. Three-tesla imaging of the knee: initial experience. Skeletal Radiol. 2005;34:453–61.
Von Engelhardt LV, Kraft CN, Pennekamp PH, Schild HH, Schmitz A, von Falkenhausen M. The evaluation of articular cartilage lesions of the knee with a 3-Tesla magnet. Arthroscopy. 2007;23:496–502.
Wong S, Steinbach L, Zhao J, Stehling C, Ma CB, Link TM. Comparative study of imaging at 3.0 T versus 1.5 T of the knee. Skeletal Radiol. 2009;38:761–9.
Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–7.
Lewicke A, Sazonov E, Corwin MJ, Neuman M, Schuckers S. Sleep versus wake classification from heart rate variability using computational intelligence: consideration of rejection in classification models. IEEE Trans Biomed Eng. 2008;55:108–18.
Rasheed S, Stashuk DW, Kamel MS. Integrating heterogeneous classifier ensembles for EMG signal decomposition based on classifier agreement. IEEE Trans Inf Technol Biomed. 2010;14:866–82.
RDC Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2007.
Hamada M, Shino K, Mitsuoka T, Toritsuka Y, Natsu-Ume T, Horibe S. Chondral injury associated with acute isolated posterior cruciate ligament injury. Arthroscopy. 2000;16:59–63.
Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med. 2009;37:955–61.
Kijowski R, Blankenbaker DG, Woods MA, Shinki K, De Smet AA, Reeder SB. 3.0-T evaluation of knee cartilage by using three-dimensional ideal grass imaging: comparison with fast spin-echo imaging. Radiology. 2010;255:117–27.
Slauterbeck JR, Kousa P, Clifton BC, Naud S, Tourville TW, Johnson RJ, et al. Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am. 2009;91:2094–103.
Van Dyck P, Vanhoenacker FM, Gielen JL, Dossche L, Weyler J, Parizel PM. Three-Tesla magnetic resonance imaging of the meniscus of the knee: what about equivocal errors? Acta Radiol. 2010;51:296–301.
Fischbach F, Bruhn H, Unterhauser F, Ricke J, Wieners G, Felix R, et al. Magnetic resonance imaging of hyaline cartilage defects at 1.5 T and 3.0 T: comparison of medium T2-weighted fast spin echo, T1-weighted two-dimensional and three-dimensional gradient echo pulse sequences. Acta Radiol. 2005;46:67–73.
Kornaat PR, Reeder SB, Koo S, Brittain JH, Yu H, Andriacchi TP, et al. MR imaging of articular cartilage at 1.5 T and 3.0 T: comparison of SPGR and SSFP sequences. Osteoarthritis Cartilage. 2005;13:338–44.
Kijowski R, Blankenbaker DG, Davis KW, Shinki K, Kaplan LD, De Smet AA. Comparison of 1.5- and 3.0-T ME imaging for evaluating the articular cartilage of the knee joint. Radiology. 2009;250:839–48.
Jung JY, Yoon YC, Kwon JW, Ahn JH, Choe BK. Diagnosis of internal derangement of the knee at 3.0-T MR imaging: 3D isotropic intermediate-weighted versus 2D sequences. Radiology. 2009;253:780–7.
Kijowski R, Davis KW, Woods MA, Lindstrom MJ, De Smet AA, Gold GE, et al. Knee joint: comprehensive assessment with 3D isotropic resolution fast spin-echo MR imaging—diagnostic performance compared with that of conventional MR imaging at 3.0 T. Radiology. 2009;252:486–95.
Notohamiprodjo M, Horng A, Pietschmann MF, Muller PE, Horger W, Park J, et al. MRI of the knee at 3 T: first clinical results with an isotropic PDFS-weighted 3D-TSE-sequence. Invest Radiol. 2009;44:585–97.
Yoon YC, Kim SS, Chung HW, Choe BK, Ahn JH. Diagnostic efficacy in knee MRI comparing conventional technique and multiplanar reconstruction with one-millimeter FSE PDW images. Acta Radiol. 2007;48:869–74.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vlychou, M., Hantes, M., Michalitsis, S. et al. Chronic anterior cruciate ligament tears and associated meniscal and traumatic cartilage lesions: evaluation with morphological sequences at 3.0 T. Skeletal Radiol 40, 709–716 (2011). https://doi.org/10.1007/s00256-010-1054-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-010-1054-6