Abstract
Purpose
The accuracy of magnetic resonance (MR) imaging in assessing meniscal and cartilage injuries in anterior cruciate ligament (ACL)-deficient knees as compared to arthroscopy was evaluated in the present study.
Methods
The results of all preoperative MR imaging performed within 3 months prior to the ACL reconstruction were compared against intraoperative arthroscopic findings. A total of 206 patients were identified. The location and type of meniscal injuries as well as the location and grade of the cartilage injuries were studied. The negative predictive value, positive predictive value, sensitivity, specificity and accuracy of MR imaging for these 206 cases were calculated and analysed.
Results
In patients with an ACL injury, the highest incidence of concomitant injury was that of medial meniscus tears, 124 (60.2 %), followed by lateral meniscus tears, 105 (51.0 %), and cartilage injuries, 66 (32.0 %). Twenty-three (11.2 %) patients sustained injuries to all of the previously named structures. MR imaging was most accurate in detecting medial meniscus tears (85.9 %). MR imaging for medial meniscus tears also had the highest sensitivity (88.0 %) and positive predictive value (88.7 %), while MR imaging for cartilage injuries had the largest specificity (84.1 %) and negative predictive value (87.1 %). It was least accurate in evaluating lateral meniscus tears (74.3 %). The diagnostic accuracy of medial meniscus imaging is significantly influenced by age and the presence of lateral meniscus tears, while the duration between MR imaging and surgery has greater impact on the likelihood of lateral meniscus and cartilage injuries actually being present during surgery. The majority of meniscus tears missed by MR imaging affected the posterior horn and were complex in nature. Cartilage injuries affecting the medial femoral condyle or medial patella facet were also often missed by MR imaging.
Conclusion
MR imaging remains a reliable tool for assessing meniscus tears and cartilage defects preoperatively. It is most accurate when evaluating medial meniscus tears. However, MR imaging should be used with discretion especially if there is a high index of suspicion of lateral meniscus tears.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The accuracy of magnetic resonance (MR) imaging in knee sports injuries has been reported to be variable [2, 3, 6, 11, 17, 28, 29, 31, 32]. As suggested by Thomas et al. [32] MR imaging might not be helpful where history and clinical findings are suggestive of an injury and when therapeutic intervention had already been planned. It was reported in their study to have low sensitivity, specificity and positive predictive value, but a high negative predictive value for MR imaging, rendering it more useful as a negative diagnostic tool [32].
In their study of 100 patients, it was reported by Rose et al. [27] that the accuracy of MR imaging was 75 % for medial meniscus tears and 69 % for lateral meniscus tears, whereas that of clinical examination were 82 and 76 %, respectively. It was concluded that MR imaging is not as cost-effective as a good clinical examination of an acutely injured knee combined with careful consideration of the patient’s medical history.
Conversely in a prospective study by Khan et al. [19] it was reported that MR imaging accuracy was 84.21 % and that of clinical examination was 63.16 %. MR imaging was found to be a valuable diagnostic tool prior to arthroscopy in a study done by Sharifah et al. [29]. In their study, MR imaging has been shown to yield accuracy rates of 88 and 92 % for medial and lateral meniscus tears, respectively [29]. Twenty-nine studies of meniscal and cruciate injuries in 3683 knees from 1991 to 2000 was systematically reviewed by Oei et al. [26]. It was shown that a higher magnetic field strength modestly improves diagnostic performance, but a significant effect was demonstrated only for ACL tears.
The diagnostic efficacy of MR imaging for meniscus tears in ACL-competent versus ACL-deficient knees has been compared by Nam et al. [24]. From their analysis, it was found that if a patient had an acute ACL tear, the sensitivity and negative predictive value of MR imaging for a meniscal tear were less than if there was no ACL tear [24].
The accuracy of MR imaging for the detection of meniscal and cartilage injuries in patients with ACL-deficient knees was evaluated in the present study. The correlation between the different variables was also studied.
Materials and methods
All ACL reconstructions performed at our institution were identified. Patients who had their surgery within three months of their preoperative MR imaging were included. All patients who underwent multiple knee ligament reconstructions and revision ACL reconstructions were excluded.
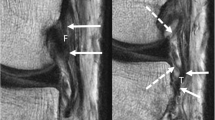
All MR imaging scans were done using the Siemens Magnetom Aera 1.5-Tesla MR scanner, taking 3-mm slice cuts. Five sequences were used: sagittal turbo spin echo photon density (time 2.42 min), axial turbo spin echo photon density (time 2.44 min), coronal turbo spin echo photon density (time 2.42 min), sagittal turbo spin echo photon density (time 2.42 min) and sagittal turbo spin echo T2 fat saturated (time 2.41 min). The field of view was 140 mm × 140 mm using a matrix resolution of 512 × 358.
The MR imaging reports were done by three musculoskeletal radiologists at our institution. The MR findings for meniscal injuries were classified based on location and pattern of the tear, while that of cartilage injuries were classified based on location and grade of the injury.
The ACL reconstructions were performed by three knee surgeons in our institution. The surgeons were not blinded to the MR imaging results. Arthroscopic findings of meniscal injuries were classified based on their location and pattern, while that of cartilage injuries were classified based on their location and Outerbridge grading. The arthroscopic findings were then documented in surgical reports following a standardised format.
Epidemiological data of each patient were collated. The findings for both MR imaging and arthroscopy were then compared to check if they matched. These were recorded and collated by two independent evaluators at the same seating to ensure test–retest reliability of measurement. If there were discrepancies in the readings, the MR imaging reports and surgical reports in question were re-read at the same seating. The negative predictive value (NPV), positive predictive value (PPV), sensitivity (Sn), specificity (Sp) and accuracy (Ac) were calculated. The different variables were also analysed using logistic regressions.
The present study was approved by the Singhealth Centralised Institutional Research Board (IRB 2012/549/D).
Statistical analysis
Statistical analyses were performed using SAS statistical software (version 9.4; SAS Institute Inc.). Multinomial logistic regressions were performed to identify significant variables affecting the classifiers of diagnosis outcomes for medial meniscal, lateral meniscal and cartilage injuries, while binary logistic regressions were performed to identify any significant variable impacting the accuracy of diagnosis or the likelihood of an actual injury. A p value of <0.05 was taken as statistically significant.
Results
Three hundred and twenty-nine patients who underwent ACL reconstructions in our institution were identified. One hundred and twenty-three patients were excluded because their surgeries were more than 3 months after MR imaging. Of the 206 patients remaining in the study, 186 were male, while 20 were female. The median age was 22 (range 17–50) years. One hundred and sixty-eight (81.6 %) cases were due to sports injuries, while 38 (18.4 %) were due to non-sports-related trauma or falls. The mean duration between MR imaging and operation was 63 (range 12–119) days.
In ACL-deficient knees, medial meniscus tears, 124 (60.2 %), were the most common concomitant finding, followed by lateral meniscus tears, 105 (51.0 %), and cartilage injuries, 66 (32.0 %). Twenty-three (11.2 %) of our ACL-deficient patients had all three types of injuries. Table 1 shows the breakdown of the injuries described and the surgical intervention.
Medial meniscus tears were the most accurately diagnosed (85.9 %) by MR imaging with the highest sensitivity (88.0 %) and positive predictive value (88.7 %). MR imaging had the highest specificity (84.1 %) and negative predictive value (87.1 %) for cartilage injuries. MR imaging was the least accurate for lateral meniscus tears (74.3 %). Table 2 summarises these results.
Among the various factors, an increase in age results in more accurate diagnoses of medial meniscus tears. In contrast, the presence of a lateral meniscus tear negatively affects diagnostic accuracy (p < 0.05). It also increases the likelihood of having a concomitant medial meniscus injury (Table 3).
For lateral meniscus tears, none of the examined variables significantly influenced diagnostic accuracy. However, the likelihood of the injury being present during arthroscopy does significantly increase if the medial meniscus is also torn, but decreases as time from MR imaging increases. Additionally, the relative log odds of false negatives versus true negatives decrease with time from MR imaging (p < 0.05) (Table 3).
The relative log odds of false-positive versus true-negative diagnoses of cartilage injuries are lower with increasing age (p < 0.05), while false negatives and true positives are less likely than true negatives as time from MR imaging increases. As more time passes, the probability of an injury actually being present during arthroscopy also falls (p < 0.05) (Table 3).
The majority of false-positive and false-negative diagnoses for meniscus tears were for injuries located in the posterior horn and involved complex tears, while for cartilage injuries, they were mainly located either on the medial femoral condyle or on medial patella facet.
Discussion
The most important finding of the present study is that although MR imaging is one of the best modes of imaging when evaluating meniscus and cartilage injuries in the knee, there are limitations to its effectiveness, especially where it concerns lateral meniscus and cartilage injuries (i.e. low positive predictive values).
Medial meniscus tears are more common in chronic ACL-deficient knees because of the higher rotatory forces and medial femoral condyle translation [5, 33]. Lateral meniscus tears are more likely in the acutely injured ACL-deficient knee [25]. In a study by Feucht et al. [12] it was also found that male patients, patients <30 years, and particularly patients who sustained contact injuries have higher risks of associated major lateral meniscus tears.
Medial meniscus tears had an incidence of 60.2 % in the present study; this is consistent with previously published studies. In a study by De Smet and Graf, 59.3 % of patients with ACL tears had a concomitant medial meniscus tear [8]. In another study done by Nam et al. [24] out of the 159 ACL-deficient knees which were examined, 59.1 % had medial meniscus tears.
Fifty-one percentage of our ACL-deficient knees had concomitant lateral meniscus tears. A rate of 44.0 % for concomitant lateral meniscus tears was reported by Nam et al. [24] while an incidence rate of 46.9 % was published by De Smet and Graf [8]. Thus, compared to published studies, our incidences of medial and lateral meniscus tears are fairly similar, with the incidence of medial meniscus tears being more common than that of lateral meniscus tears in ACL-deficient knees.
From the present study, the presence of a lateral meniscus tear increases the likelihood of a medial meniscus tear being present (p < 0.05). The reverse is also true (p < 0.05). This is likely as the initial injury tearing the ACL potentially tears the lateral meniscus and the subsequent instability leads to tears in the medial meniscus. There should be a high index of suspicion of a concomitant tear in the other meniscus whenever one meniscus shows a tear.
Furthermore, if a lateral meniscus tear were present, the diagnostic accuracy for medial meniscus tears was negatively affected. This was reflected by the fact that we were twice as likely to make a false-negative diagnosis as compared to a true-positive diagnosis. As such, should there be a meniscus tear in one compartment, special attention must be paid to the other compartment before ruling out a meniscus tear there.
MR imaging is a valuable non-invasive and reasonably accurate diagnostic tool [3, 4, 11, 22]. Recent literature on MRI accuracy for knee injuries differs widely in their conclusions (Table 4) [27, 29, 32]. As such, differing recommendations by various authors have been made on the use of MRI for evaluation prior to arthroscopy [29, 32].
Fifty-nine articles with a total of 7367 MR imaging scans were systematically reviewed by Crawford et al. [6]. It was found that MR imaging for medial meniscus tears had accuracy, sensitivity and specificity of 86.3, 91.4 and 81.1 %, respectively [6]. Similar results to this published meta-analysis, i.e. 85.9, 88.0 and 82.7 %, were reported by the present study. Nonetheless, widely varying accuracy rates for MR imaging in the diagnosis of meniscus tears have been reported by other authors [17, 32].
The sensitivity for lateral meniscus tears was found to be 80.2 %. This is again comparable to the published sensitivity rates of 76 % in a meta-analysis by Crawford et al. [6] and 79.3 % in the study by Oei et al. [26]. We postulate that diagnostic accuracy for lateral meniscal injuries will always be lower than that for medial meniscal tears because of the anatomy. The presence of a popliteus tendon and popliteal hiatus can affect the accurate diagnosis of posterior horn lateral meniscal tears.
In the present study, it was found that for both the lateral meniscus and cartilage, a longer time from MR imaging to surgery reduces the likelihood of finding an injury during arthroscopy and lowers the type II error rate (i.e. false negatives). As our cohort is relatively young, we suspect that there may be some degree of age-dependent self-healing. This is further evidenced by significantly lower probabilities of false positives for medial meniscal and cartilage injuries with advancing age. It is possible that the younger the patient is, the higher the chances that lesions initially identified on MR imaging may have healed by the time of arthroscopic surgery. In addition, the log odds of an accurate diagnosis rise by 0.0604 with each additional year (p < 0.05), which could be due to the fact that older patients are more prone to degenerate tears that are more clearly defined on MR imaging and unlikely to heal given time.
The potential for meniscal healing is also dependent on its location with peripheral zone tears having superior healing potential [20, 21]. This has been attributed to the vascular anatomy proposed by Arnoczky and Warren [1]. Not all meniscal tears require repair as some can heal spontaneously [16, 25]. A lower number of lateral meniscus tears in chronic ACL tears were reported by Nikolic. This was attributed to the healing of small tears [25].
Similar to other studies, false-positive and false-negative tears were mostly in the posterior horns of the meniscus [6, 29]. It was highlighted by Sharifah et al. [29] that the oblique course of the posterior horn relative to the coronal and sagittal MR images could have been a possible cause.
MR imaging has a sensitivity of 70.5 % and specificity of 84.1 % when used to diagnose cartilage injuries. In comparison, the sensitivity quoted by other published studies ranged from as low as 0 % to as high as 94 % [2, 23, 31], while the published specificity is between 97 and 100 % [2, 31]. The wide variation in results is due to the location, size and depth of the lesion, along with the MR imaging sequence, field strength and contrast agent [10, 15, 18].
In a meta-analysis summarised by Smith et al. [30] MR imaging while resulting in high specificity has poorer sensitivity when used to diagnose cartilage disease. Additionally, higher-field-strength MR imaging machines are superior to lower-field-strength equipment and higher-grade lesions are easier to detect than lower-grade ones. The study by Figueroa et al. [13] had an MR imaging sensitivity of 45 % and specificity of 100 %. It was also highlighted that a considerable number of lesions will remain undetected until arthroscopy. The utility of MR imaging in diagnosing cartilage injuries has been concluded to be more doubtful than in diagnosing meniscus tears [23].
It has been shown by the present study that most false readings for cartilage were for injuries in the medial femoral condyle and medial patella facet in contrast to the findings by Disler et al. [9] (Table 4). It was reported in their study that the lateral tibial plateau resulted in the most false readings for cartilage injuries. Like us, it has been concluded by many authors that MR imaging is not able to replace arthroscopy as a diagnostic tool, but may be used as a tool for exclusion due to its high specificity [13, 14].
The present study confirms that medial meniscus injuries are more common than lateral meniscus injuries in ACL-deficient knees. In addition, more than 30 % of ACL-deficient knees had tears in both menisci, emphasising the importance of careful inspection of both menisci during surgery. According to the present study, age is a significant positive factor affecting the diagnostic accuracy of MR imaging for medial meniscus tears. MR imaging has also been found to have poorer accuracy in the detection of tears in the lateral meniscus. It may be prudent to include this information when counselling patients preoperatively.
One limitation of this study is the assumption of arthroscopy being the gold standard for confirmation. The direct visualisation of a tear is confirmation of the injury, but it is still surgeon dependent [19, 27]. The second limitation is that we reviewed all patients who had their surgery within 3 months of their MR imaging. Ideally, it would be better if the time from MR imaging to surgery was less than 6 weeks. However due to our referral pattern, the waiting time till surgery is approximately 2–3 months. Having 6 weeks as a criterion would leave a sample size that is too small to evaluate.
Finally, there was no control group used. The analysis of diagnostic accuracy of MR imaging in detecting menisci and chondral injuries in patients without ACL injury would have been possible with a control group of ACL-competent knees.
Conclusion
MR imaging remains a reliable tool for assessing meniscal tears and cartilage defects preoperatively. It is most accurate for evaluating medial meniscal tears and least accurate for lateral meniscal tears.
References
Arnoczky SP, Warren RF (1982) Microvasculature of the human meniscus. Am J Sports Med 10:90–95
Bredella MA, Tirman PF, Peterfy CG, Zarlingo M, Feller JF, Bost FW, Belzer JP, Wischer TK, Genant HK (1999) Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. Am J Roentgenol 72:1073–1080
Carmichael IW, MacLeod AM, Travlos J (1997) MRI can prevent unnecessary arthroscopy. J Bone Joint Surg Br 79:624–625
Chissell HR, Allum RL, Keightley A (1994) MRI of the knee: its cost-effective use in a district general hospital. Ann R Coll Surg Engl 76:26–29
Cipolla M, Scala A, Gianni E, Puddu G (1995) Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees. Classification, staging and timing of treatment. Knee Surg Sports Traumatol 3:130–134
Crawford R, Walley G, Bridgman S, Maffulli N (2007) Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull 84:5–23
Crues JC, Mink J, Levy IL, Lotysch M, Stolter DW (1987) Meniscal tears of the knee: accuracy of MR imaging. Radiology 164:445–448
De Smet AA, Graf BK (1994) Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. Am J Roentgenol 162:905–911
Disler DG, McCauley TR, Kelman CG, Fuchs MD, Ratner LM, Wirth CR, Hospodar PP (1996) Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. Am J Roentgenol 167:127–132
Eckstein F, Charles HC, Buck RJ, Kraus VB, Remmers AE, Hudelmaier M, Wirth W, Evelhoch JL (2005) Accuracy and precision of quantitative assessment of cartilage morphology by magnetic resonance imaging at 3.0T. Arthritis Rheum 52:3132–3136
Feller JA, Webster KE (2001) Clinical value of magnetic resonance imaging of the knee. ANZ J Surg 71:534–537
Feucht MJ, Bigdon S, Bode G, Salzmann GM, Dovi-Akue D, Südkamp NP, Niemeyer P (2015) Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg 10:34
Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I (2007) Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy 23:312–315
Friemert B, Oberlander Y, Schwarz W, Haberle HJ, Bahren W, Gerngross H, Danz B (2004) Diagnosis of chondral lesions of the knee joint: can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc 12:58–64
Grossman JW, De Smet AA, Shinki K (2009) Comparison of the accuracy rates of 3-T and 1.5-T MRI of the knee in the diagnosis of meniscal tear. Am J Roentgenol 193:509–514
Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW (1988) Arthroscopic meniscus repair with a posterior incision. Instr Course Lect 137:209–221
Jee WH, McCauley TR, Kim JM (2004) Magnetic resonance diagnosis of meniscal tears in patients with acute anterior cruciate ligament tears. J Comput Assist Tomogr 28:402–406
Kawahara Y, Uetani M, Nakahara N, Doiguchi Y, Nishiguchi M, Futagawa S, Kinoshita Y, Hayashi K (1998) Fast spin-echo MR of the articular cartilage in the osteoarthritic knee. Correlation of MR and arthroscopic findings. Acta Radiol 39:120–125
Khan HA, Ahad H, Sharma P, Bajaj P, Hassan N, Kamal Y (2015) Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma Mon 20:e18635
King D (1990) The healing of semilunar cartilages. Clin Orthop Relat Res 252:4–7
Kobayashi K, Fujimoto E, Deie M, Sumen Y, Ikuta Y, Ochi M (2004) Regional differences in the healing potential of the meniscus—an organ culture model to eliminate the influence of microvasculature and the synovium. Knee 11:271–278
Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J (1998) Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology 166:861–864
Munk B, Madsen F, Lundorf E, Staunstrup H, Schmidt SA, Bolvig L, Hellfritzsch MB, Jensen J (1998) Clinical magnetic resonance imaging and arthroscopic findings in knees: a comparative prospective study of meniscus, anterior cruciate ligament and cartilage lesions. Arthroscopy 14:171–175
Nam TS, Kim MK, Ahn JH (2014) Efficacy of magnetic resonance imaging evaluation for meniscal tears in acute anterior cruciate ligament injuries. Arthroscopy 30:475–482
Nikolic DK (1998) Lateral meniscal tears and their evolution in acute injuries of the anterior cruciate ligament of the knee. Arthroscopic analysis. Knee Surg Sports Traumatol Arthrosc 6:26–30
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG (2003) MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 22:837–848
Rose NE, Gold SM (1996) A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruciate ligament tears. Arthroscopy 12:398–405
Rubin DA, Kettering JM, Towers JD, Britton CA (1998) MR imaging of knees having isolated and combined ligament injuries. Am J Roentgenol 170:1207–1213
Sharifah MI, Lee CL, Suraya A, Johan A, Syed AF, Tan SP (2015) Accuracy of MRI in the diagnosis of meniscal tears in patients with chronic ACL tears. Knee Surg Sports Traumatol Arthrosc 23:826–830
Smith TO, Drew BT, Toms AP, Donell ST, Hing CB (2012) Accuracy of magnetic resonance imaging, magnetic resonance arthrography and computed tomography for the detection of chondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc 20:2367–2379
Spiers AS, Meagher T, Ostlere SJ, Wilson DJ, Dodd CA (1993) Can MRI of the knee affect arthroscopic practice? A prospective study of 58 patients. J Bone Joint Surg Br 75:49–52
Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P (2007) The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc 15:533–536
Yao J, Snibbe J, Maloney M, Lerner AL (2006) Stresses and strains in the medial meniscus of an ACL deficient knee under anterior loading: a finite element analysis with image-based experimental validation. J Biomech Eng 12:135–141
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, K.P.L., Han, A.X., Wong, J.L.Y. et al. Reliability of magnetic resonance imaging in evaluating meniscal and cartilage injuries in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc 25, 411–417 (2017). https://doi.org/10.1007/s00167-016-4211-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4211-1