Abstract
Objective
To investigate the usefulness of multi-detector computed tomography (MDCT) in three-part intertrochanteric fractures of proximal femur.
Materials and Methods
Twenty-six patients with Boyd-Griffin type 2 intertrochanteric fractures with MDCT (group 1) and 36 patients of the same type fracture without MDCT (group 2) were compared. Lesser trochanter (LT)/greater trochanter (GT) volume ratio above 0.5 or the volumetric proportion of GT in total volume of proximal femur below 25% was considered an unstable fracture. The fractures were fixed with dynamic compression hip screws (DCS). Additional greater trochanter stabilizing (GTS) plate or bone cement augmentation of the femoral head was performed in unstable fractures. Clinical outcome between the two groups by fixation failure and radiological results was compared.
Results
The volume ratio of the LT/GT was 0.33 (range, 0.13–0.73). The volume of the LT was inversely correlated with that of the GT (p < 0.001). The volume of the GT was significantly correlated with the LT/GT ratio or the head and neck (HN)/GT ratio (p < 0.001). Seven cases were regarded as unstable fractures in group 1. Fixation failures happened in one case in group 1 and five cases in group 2. There was significantly lower failure rate in group 1 than group 2 (p = 0.03). Neck-shaft angle at last follow-up was 134.8° ± 5.3 in group 1 and 131.3° ± 5.1 in group 2 (p = 0.01). The sliding length of lag screws were 5.6° ± 2.9 mm in group 1 and 8.3° ± 3.2 in group 2 (p = 0.03).
Conclusion
Preoperative use of MDCT provides useful information about the fracture pattern and the geometry of the proximal femur in unstable intertrochanteric fractures and helps surgical planning. The ratio of the LT to the GT is inversely correlated with fracture stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intertrochanteric fractures in the elderly are a frequent problem and are becoming more common as the proportion of elderly people in the population increases. Sometimes such fractures can become life-threatening disasters during or after treatment in elderly patients [1]. Surgery is the treatment of choice for both stable and unstable intertrochanteric fractures [2, 3], with the goal of achieving stable fixation to allow early patient mobilization and to restore the patient’s previous level of activity and function [3, 4].
Compression hip screws have been widely used for the treatment of intertrochanteric fractures because of their biomechanical and theoretic advantages [5, 6], but they have a relatively higher rate of failure compared to other methods [1, 7–10]. Excessive sliding of the lag screw or cutting out from the femoral head are common failure modes, especially in unstable fractures. Factors contributing to fixation failures in intertrochanteric fractures using compression hip screws are facture stability, comminution, osteoporosis, the type of reduction, and surgical techniques [3, 7, 8, 11]. This combination of factors has been implicated in the difficulty in obtaining and maintaining stable reduction and rigid internal fixation of unstable intertrochanteric fractures. The use of methylmethacrylate bone cement in osteoporotic intertrochanteric fractures reduced significantly the incidence of cutting-out of lag screws by increasing the purchase power of the screw within the head [12].
The classification system of trochanteric fractures contains valid information about fracture stability, but sometimes surgeons using them still cannot predict precisely the risk of postoperative fixation failure. Also, surgeons may have seen different clinical outcomes of trochanteric fractures, even among those with fracture patterns, degree of osteoporosis, and quality of applied surgical techniques that are nearly the same.
Boyd-Griffin type 2, posteromedial comminuted fractures, are the most frequent fracture pattern of unstable fractures [13]. The posteromedial fragment is thought to be the keystone to mechanical stability for intertrochanteric fractures. It has long been known that the size of the displaced posteromedial fragment affects fracture stability [14, 15]. Jacobs et al. [16] suggested that the greater trochanter plays the role of lateral buttress in resisting stress during impaction of fracture surfaces. Also, use of an attachable lateral support plate could greatly decrease the rate of fixation failures in unstable intertrochanteric fractures [17]. Recent research has addressed the importance of the lateral trochanteric wall for maintenance of stable bone-implant construction in the treatment of intertrochanteric fractures with dynamic compression hip screws [18]. We hypothesized that the size of the lateral trochanteric wall as well as the size of posteromedial fragment can affect fracture stability and that the size of both fragments could affect each other’s stability.
Osteosynthesis is the treatment of choice in stable trochanteric fractures, whereas replacement arthroplasty [19] can be another surgical option in severely unstable fractures, especially in elderly patients. Thus, a precise preoperative evaluation of stability in intertrochanteric fractures is very important for surgical planning. Three-dimensional CT scanning is a useful tool for understanding the exact type of fracture pattern and estimating dimensional volumes or bone-mineral density. We investigated how the volumetric proportions are distributed among each fragment of Boyd-Griffin type 2 intertrochanteric femoral fractures by measuring the dimensional volumes of fragments in elderly patients for determining fracture stability. When the fracture was regarded as an unstable one, we applied DCS plus additional fixation such as GTS plate or bone cement augmentation to enhance the stability of bone-implant assembly. And we preoperatively evaluated the efficacy of MDCT for predicting the fracture stability of a three-part intertrochanteric fracture.
Materials and methods
Between March 2004 and February 2006, 69 patients, each at least 65 years old, were admitted to our institution with three-part intertrochanteric fractures (Boyd-Griffin type 2 or Jensen’s modification [20] of Evans’s classification type 4) were included in our study. According to AO/OTA classification, there were 6 cases in A2.1, 18 cases in A2.2 and 2 cases in A2.3 in group 1. In group 2, there were 14 cases in A2.1, 19 case in A2.2 and 3 cases in A2.3. Among them, seven patients were excluded due to inadequate period of follow-up or death. Fifty-eight patients were injured when they slipped; the other 4 patients were injured when they fell down. Consecutive 26 patients (3 males and 26 females, group 1) with MDCT (group 1) between February 2005 and February 2006 and consecutive 36 patients (7 males and 29 females, group 2) without MDCT (group 2) between March 2004 and January 2005 were included. The average age of the patients was 76.7 years (range, 65–89 years) in group 1 and 77.6 years (range, 65-95) in group 2.
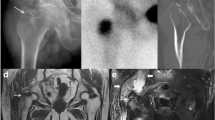
Before surgery, all patients underwent three-dimensional 16-row multidetector CT scanning (Light Speed 16, GE Healthcare, Waukesha, WI, USA) with 1.25-mm acquisition. Intravenous contrast was not used. Scan duration was 8-10 s depending on the area to be scanned. Slice thickness was 1.25 mm and pitch was 1.375. Table speed was 17 mm/s. The kVp was 120 with 50-350 mA. CT raw data were transferred to a workstation (AW 4.1 systems using the volume analysis software tool; GE, Waukesha, WI, USA), and volume rendering image and multiplanar reconstruction were obtained. The three fragments of Boyd-Griffin type 2 intertrochanteric fractures were classified as the lesser trochanter (LT), greater trochanter (GT), and the femoral head-neck (HN). GT was defined as the bony fragment from the proximolateral bony protrusion of the femoral shaft from its top to 7 cm below. The volume of each fragment was measured by a musculoskeletal radiologist. LT/GT volume ratio above 0.5 or the volumetric proportion of GT in total volume of proximal femur below 25% is considered as an unstable fracture. All patients in both groups were operatively given dynamic compression hip screws by a single surgeon (SKH). When LT/GT volume ratio was above 0.5, we performed an additional plating using TSP (Fig. 1). And when the volumetric proportion of GT in total volume of proximal femur was below 25%, we augmented bone cement around the lag screw in the femoral head. Preoperatively, we did not consider the status of bone densitometry because all patients in our study were elderly. Also, the choice of bone cement was done only by our criteria.
A Boyd-Griffin type 2 intertrochanteric fracture in an 84-year old woman, caused by a slip. Anteroposterior hip radiograph (a) showed a displaced three-fragment fracture (arrows) with severe osteoporosis. Three-dimensional volume rendering image (b) clearly demonstrated each of the three fragments such as head and neck (HN), greater trochanter (GT), and lesser trochanter (LT). GT was measured from its top to 7 cm below (c). Volume of each fragment was automatically and manually calculated (d–f). LT/GT ratio in this patient is calculated to be above 0.5, so we considered it as an unstable fracture. Postoperative hip radiograph (g) showed good alignment of femoral head and neck with dynamic compression hip screw (DCS) (arrow) with additional greater trochanter stabilizing (GTS) plate (arrow head)
Fixation failure was defined as the cutting-out of the lag screw from the head, nonunion or excessive sliding of the lag screw more than 25 mm. We also measured neck-shaft angle and sliding length of the leg screw in hip anteroposterior (AP) radiograph. Clinical outcome was compared between two groups by fixation failure and radiological results.
Statistics
SPSS software (version 11.0 for Windows 95, SPSS, Chicago, IL, USA) and the Kruskal-Wallis test, Student’s t-test, and Pearson correlation coefficient analysis were used to analyze the data. A p value of <0.05 was considered statistically significant.
Results
Radiologic measurements by MDCT
The mean volume of the proximal femur (the sum of the volumes of the three fragments) was 157.8 ± 13.2 cm3. The mean volume of the LT was 14.7 ± 4.2 cm3, and the proportion of the LT in the proximal femur was 9.3 ± 2.1%. The mean volume of the GT was 51.5 ± 13.9 cm3, and its proportion in the proximal femur was 32.1 ± 7.9%. The ratio of the LT to the GT was 0.33 (range, 0.13–0.73). The mean volume of the GT was approximately 3 times that of the LT. The mean volume of the HN was 92.0 ± 11.1 cm3, and its proportion in the proximal femur was 58.3 ± 6.1%. The volume of the LT in the proximal femur was inversely correlated with that of the GT (p < 0.001). Also, the proportion of the LT in the proximal femur was significantly correlated with the proportion of the GT or the HN in the proximal femur (p < 0.001). The average ratio of the LT to the GT was 0.33 (range, 0.13–0.73), and the differences in ratio varied 1–6 times. The average ratio of the HN to the GT was 1.99 (range, 1.1–4.1), and the differences in ratio varied 1–4 times. However, the average ratio of the LT to the HN was 0.16 (range, 0.12–0.19), and it was relatively consistent. Patient profile and volumes of each fragment are summarized in Table 1. The volume of the GT was significantly correlated with the ratios of the LT to the GT and of the HN to the GT (p < 0.001). Also, the volumetric proportion of the GT in the proximal femur had a significant inverse correlation with the proportion of the LT in the proximal femur (p < 0.001).
Clinical and radiologic results
There was no definite difference in age and sex between group 1 and 2 (p = 0.21). There was one case of fixation failure in group 1, whereas as in group 2 there were five cases including three cases of cutting-out, one case of nonunion and one case of excessive sliding of lag screw failed (Figs. 1 and 2). Fixation failure is more common in group 2 (p = 0.03). Neck-shaft angle at hip AP radiograph was 134.8° ± 5.3 in group 1 and 131.3° ± 5.1 in group 2 (p = 0.01). The sliding length of lag screw which is measured by Doppelt method [7] was 5.6° ± 2.9 mm in group 1 and 8.3° ± 3.2 in group 2 (p = 0.03). Patients with MDCT had lesser rate of fixation failure and better radiologic results than patients without MDCT.
Boyd-Griffin type 2 intertrochanteric fracture in a 71-year old woman happened by slip. Anteroposterior hip radiograph (a) showed a displaced three-fragment fracture (arrows) with severe osteoporosis. MDCT was not used in this case. Immediate postoperative hip radiograph (b–c) showed good alignment of fracture with using the dynamic compression hip screw (DCS) (arrow). Posteroperative hip radiography (d) after 2 months showed fixation failure (arrow head) with excessive sliding of lag screw (arrow)
Discussion
Despite advances in devices and technologies, fixation failure still remains a problem for patients who have unstable intertrochanteric fractures [4, 6–8, 10]. The preferred treatment for intertrochanteric fractures is internal fixation and early mobilization [4, 8, 9, 13]. Many researchers have investigated the factors essential to avoiding mechanical complications and improving fixation stability. The Evans classification [2] emphasizes the number and pattern of fracture fragments in assessing fracture stability. Efforts to achieve stable fixation of unstable intertrochanteric fractures have included valgus osteotomy [21], medial displacement osteotomy [15], lateral displacement reduction [22], anatomic reduction [2, 15], and the use of adjunctive methylmethacrylate [12]. Kim et al. [7] found that the most important cause of dynamic hip screw failure was fracture instability. Many fracture classifications [2, 13, 20] of intertrochanteric hip fractures have been created to assess fracture stability. However, most divide intertrochanteric fractures into stable and unstable patterns on the basis of appearance on plain radiographs, mainly explained by degree of comminution. They can sometimes provide useful guidelines for surgeons to decide on treatment strategies.
Some of them, however, provide questionable reliability in predicting surgical outcome. The difficulty in predicting the degree of complication risks in fixation prompted us to propose another tool for obtaining more precise information about fracture patterns and their fracture stability. Thomsen et al. [23] found that trabecular bone volume is correlated with bone strength. This is illustrated by the fact that the volume of the GT is related to its ability to provide stability in three-part intertrochanteric fractures. The smaller the LT and the larger the GT, the greater the fracture stability and the lower the risk of fixation failure becomes:
Fracture stability
CT scanning is primarily used in acute trauma, particularly for acetabular fracture or hip dislocation to detect intra-articular fragments and associated articular surface fractures and to better depict fracture patterns for surgical planning. In 1987, Konishi and Sato [24] first described three-dimensional observations of trochanteric fractures to define their exact type and the location of the fracture line. Recently, MDCT has been used to evaluate the relationship between fracture load and regional bone mineral density in hip fractures [25]. MDCT was used to measure the volume of bony fragments in intertrochanteric fractures.
In the treatment of intertrochanteric femoral fractures, the intactness of the posteromedial cortex and of the structural buttressing provided by the GT are thought to be critical to fracture stability. However, the relative roles of the LT and the GT in fracture stability have not yet been established. Posteromedial cortical contact of the fracture fragments is known to be important to allow physiologic distribution of load and to provide resistance to migration of the femoral head and neck into varus angulation and retroversion [3, 15, 16]. Apel et al. [14] conducted biomechanical experiments showing that the size of the posteromedial fragment is important in fracture stability. However, Laros and Moore [9] found that there was no significant correlation between fixation complications and the size of the LT. That finding can be explained, though, by numerous other factors affecting treatment results such as the reduction method, osteoporosis, medical diseases, and surgical techniques. May and Chacha [26] reported the role of the GT in influencing fragment displacement and stability through the posterior soft-tissue hinge. Biomechanical studies [16, 22] have demonstrated that the sliding hip screw acts as a lateral tension band in stable fracture patterns, transmitting force through the medial cortex. If the lateral buttress is lost in an unstable fracture, a compression hip screw alone cannot resist physiologic stress during the fracture healing process. Gotfried [18] has explained the importance of the integrity of the lateral wall for successful treatment of pertrochanteric fractures, especially when treated using dynamic compression hip screws.
We have dealt with delayed fracture of the GT, which protects against excessive sliding of the proximal fragment along the lag screw in Boyd-Griffin type 2 fractures, which eventually results in fixation failure. Using a GT stabilizing plate or intramedullary nailing, or performing a replacement arthroplasty can be a solution when the lateral support is already lost. The use of additional plating or bone cement augmentation decreased the incidence of fixation failure in treatment of unstable intertrochanteric fractures of the femur in our selective cases. But the routine use of them can increase the risk of trochanteric bursitis, longer operation time, and penetration of cement into the joint or fracture interface [2, 19, 22]. Our hypothesis is that the cases with LT/GT volume ratio above 0.5 or the volumetric proportion of GT in total volume of proximal femur below 25% are unstable fractures. The concept implies that the volumetric distribution of each fragment in three-part intertrochanteric fractures can affect the stability of fracture and the importance of the GT volume to resist compressive forces across the fracture site during the healing process when they are fixed by DCS.
Superior clinical and radiological results were obtained by preoperative use of MDCT in unstable intertrochanteric fractures. Also, it is noteworthy that fractures with the same type of fracture patterns have a wide range of volumetric proportions for each fragment which can result in different clinical findings, even though they belong to the same fracture classification system.
In our study, the answer to the question of which fragment, the GT or the LT, is more important to fracture stability in Boyd-Griffin type 2 intertrochanteric fractures could not be established. However, our results suggest that when the LT volume is large, the GT volume becomes small and the fracture stability may worsen. The ratio of the LT to the GT ranged from 0.13 to 0.73. We believe that fractures with the lowest LT-to-GT ratio have greater stability than fractures with the highest such ratio. Additional clinical and biomechanical studies are needed to verify our findings, however. In conclusion, preoperative use of CT in unstable intertrochanteric fractures can provide better and more predictable fixation outcomes, and lower LT-to-GT ratio correlates with more stable fracture.
References
Laskin RS, Gruber MA, Zimmerman AJ. Intertrochanteric fractures of the hip in the elderly: a retrospective analysis of 236 cases. Clin Orthop Relat Res. 1979;141:188–95.
Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Am. 1949;31B(2):190–203.
Koval KJ, Zuckerman JD. Hip fractures: II. Evaluation and treatment of intertrochanteric fractures. J Am Acad Orthop Surg. 1994;2(3):150–6.
Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004;53:441–53.
Dimon JH, Hughston JC. Unstable intertrochanteric fractures of the hip. J Bone Joint Surg Am. 1967;49(3):440–50.
Doppelt SH. The sliding compression screw: today’s best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980;11(3):507–23.
Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001;25(6):360–2.
Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61(2):216–21.
Laros GS, Moore JF. Complications of fixation in intertrochanteric fractures. Clin Orthop Relat Res. 1974;101:110–19.
Whitelaw GP, Segel D, Sanzone CF, et al. Unstable intertrochanteric/subtrochanteric fractures of the femur. Clin Orthop Relat Res. 1990;252:238–45.
Walsh ME, Wilkinson R, Stother IG. Biomechanical stability of four-part intertrochanteric fractures in cadaveric femurs fixed with a sliding screw-plate. Injury. 1990;21(2):89–92.
Bartucci EJ, Gonzalez MH, Cooperman DR, et al. The effect of adjunctive methylmethacrylate on failures of fixation and function in patients with intertrochanteric fractures and osteoporosis. J Bone Joint Surg Am. 1985;67(7):1094–107.
Boyd HB, Griffin LL. Classification and treatment of inter-trochanteric fractures. Arch Surg. 1949;58:853–66.
Apel DM, Patwardhan A, Pinzur MS, Dobozi WR. Axial loading studies of unstable intertrochanteric fractures of the femur. Clin Orthop Relat Res. 1989;246:156–64.
Den Hartog BD, Bartal E, Cooke F. Treatment of the unstable intertrochanteric fracture: effect of the placement of the screw, its angle of insertion, and osteotomy. J Bone Joint Surg Am. 1991;73(5):726–33.
Jacobs RR, McClain O, Armstrong HJ. Internal fixation of intertrochanteric hip fractures: a clinical and biomechanical study. Clin Orthop Relat Res. 1980;146:62–70.
Su ET, DeWal H, Kummer FJ, Koval KJ. The effect of an attachable lateral support plate on the stability of intertrochanteric fracture fixation with a sliding hip screw. J Trauma. 2003;55(3):504–8.
Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;425:82–6.
Waddell JP, Morton J, Schemitsch EH. The role of total hip replacement in intertrochanteric fractures of the femur. Clin Orthop Relat Res. 2004;429:49–53.
Jensen SL. Trochanteric fractures. Acta Orthop Scand. 1981;188(Suppl):1–100.
Sarmiento A, Williams FM. The unstable intertrochanteric fracture: treatment with a valgus osteotomy and I-beam nail plate—a preliminary report of one hundred cases. J Bone Joint Surg Am. 1970;52(7):1309–18.
Kaufer H, Matthews LS, Sonstegard D. Stable fixation of intertrochanteric fractures: a biomechanical evaluation. J Bone Joint Surg Am. 1974;56:899–907.
Thomsen JS, Ebbesen EN, Mosekilde L. Predicting human vertebral bone strength by vertebral static histomorphometry. Bone. 2002;30(3):502–8.
Konishi N, Sato K. Three-dimensional observations of trochanteric fractures of the femur. Nippon Seikeigeka Gakkai Zasshi. 1987;61(2):97–106.
Bessho M, Ohnishi I, Okazaki H, et al. Prediction of the strength and fracture location of the femoral neck by CT-based finite-element study on patients with hip fracture. J Orthop Sci. 2004;9(6):545–50.
May JMB, Chacha PB. Displacements of trochanteric fractures and their influence on reduction. J Bone Joint Surg Br. 1968;50(2):318–23.
Acknowledgements
We thank Katharine O’Moore-Klopf, ELS, for providing editorial assistance.
Conflict of Interest Statement
The authors declare that they have no conflicts of interest, financial or otherwise, to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, SK., Lee, BY., Kim, YS. et al. Usefulness of multi-detector CT in Boyd-Griffin type 2 intertrochanteric fractures with clinical correlation. Skeletal Radiol 39, 543–549 (2010). https://doi.org/10.1007/s00256-009-0795-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-009-0795-6