Abstract
Objective
This study was undertaken to evaluate the use of digital tomosynthesis (tomogram) for diagnosis of suspected fracture neck of femur (NOF). We hypothesised that the use of cross-sectional imaging (MRI/CT) could be reduced by using tomogram to separate the patients with suspected NOF fractures that require MRI/CT scan from those who do not.
Materials and method
Forty-one patients with a clinically suspected NOF fracture, following trauma, with negative AP and lateral hip X-rays, underwent a hip tomogram examination. Patients with a negative tomogram and clinically moderate to high probability of a hip fracture underwent MRI/CT within 48 h.
Result
Tomogram identified fracture NOF in six patients, who underwent appropriate surgical treatment without needing further imaging. Fifteen patients, with negative tomogram examinations for fracture NOF and a low clinical probability of a fracture did not undergo additional MRI/CT scanning. At 6 months of follow-up, none of the patients returned to the hospital with complications. Twenty patients with moderate to high clinical probability of fracture NOF with negative or inconclusive tomogram underwent additional MRI/CT scanning (19 MRI, 1 CT). Two patients showed fracture NOF, and one patient with greater trochanter fracture on tomogram showed fracture NOF on MRI scan. Seventeen patients showed soft tissue injury, bone oedema or pubic rami/acetabular fractures on MRI scan.
Conclusion
Tomogram is a reliable imaging modality that can be used to select the patients who will need additional MRI/CT scan following negative or equivocal plain X-ray in patients with suspected hip fractures following fall.
Level of evidence
III
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neck of femur (NOF) fracture is a common and serious injury affecting mainly the elderly population following simple falls. With increasing life expectancy throughout the globe, the number of elderly individuals is increasing in every geographical region. It is estimated that the incidence of hip fractures will rise from 1.66 million in 1990 to 6.26 million by 2050 [1–4]. The diagnosis of these fractures is usually straightforward with the use of anteroposterior (AP) and lateral radiographs. In small number of patients, these standard radiographs can be inconclusive or normal even in the presence of fracture [5]. If these fractures remain undiagnosed, the risk of morbidity, mortality and prolonged hospitalisation increases, with a delay of 2 days in surgical treatment for an acute hip fracture doubling the mortality [1, 6]. In addition, a missed undisplaced fracture may displace, resulting in a change in management or outcome and leading to prolonged rehabilitation [7–10].
The incidence of occult hip fractures is reported to be 2–37 % [11]. Detection of these fractures can be difficult as most of the patients are elderly, and it may be difficult to obtain optimal hip radiographs [3, 5, 12, 13]. Osteoporosis and advanced osteoarthritis both increase the probability of equivocal radiographs in this patient group [14–16]. Up to 12 % radiographs may be reported as definite or possible hip fracture, where subsequent MRI scan was negative [17]. In practice, a suspicion of fracture NOF, despite negative plain X-ray studies, usually prompts additional imaging to detect or exclude the pathology. Magnetic resonance imaging (MRI) is the gold standard in detecting occult hip fractures [1, 14, 18, 19]. MRI scanning is an expensive and time-consuming imaging modality, which is not readily available, in most hospitals especially after working hours. Other imaging modalities that can be used to identify an occult NOF include computerised tomography (CT) scans [20, 21] and isotope bone scanning [22, 23].
Digital tomosynthesis (tomograms) uses a standard linear accelerator and X-ray system to create a sequence of tomographic planes by a single sweep of the X-ray tube. It works similar to linear tomography, but instead of accumulating the total exposure and reconstructing a single image, as with linear tomography, a series of individual images, each with very low dose, is taken during the sweep of the tube. This series of images of the patient’s body from different angles is used in reconstruction algorithm (filtered back-projection), similar to the algorithm in CT, to create images of different planes through the patient body. A number of images with planes parallel to the detector with a distance of 1 mm (or several mm) can be reconstructed from the same set of acquired projection images. For hip joint imaging, a series of 60 projection images over an angle of 40° (±20°) is taken during a time of approximately 10 s. The motion of the tube is linear and continuous. The radiation dose is significantly smaller than a CT scan of the given area.
The uses of tomograms have been described previously as an imaging modality for a variety of clinical indications, including extremity fracture detection, arthroplasty imaging and chest abnormalities [10, 15, 17, 24–26]. It has never been described for use in identifying neck of femur fractures. The purpose of this study is to review the utility of tomogram in the diagnosis of occult hip fractures. In addition, this study will evaluate whether the use of tomograms in a NOF pathway can be useful to reduce the need for MRI or CT scanning for patients with suspected NOF fracture.
Materials and methods
Study design
The study protocol was approved by the local ethics committee. From February 2012 to March 2014, all patients with clinically suspected NOF fractures following trauma and negative AP and lateral hip X-rays underwent hip tomograms. Patients in whom tomogram identified fracture NOF underwent standard treatment for fracture NOF. Those patients who had a negative tomogram were reassessed by senior orthopaedic clinician and were separated into two categories: (1) patients with clinically moderate to high probability of NOF fracture went on to have MRI/CT scan within 48 h and (2) patients with low clinical probability of NOF fracture did not undergo MRI/CT scan.
Patient selection
Forty-three patients with suspected fracture NOF and negative AP and lateral hip radiographs were imagined with tomogram. Two patients were excluded from the study because of delayed MRI scan (4 days) as the delay of more than 48 h was out of recommendations. Forty-one patients were included in the trial, 13 male and 28 female, with an average age of 83 years (range 69–97 years). Informed consent was not required since the tomogram is indicated for human imaging and clinical trial maintained the recommended standard of clinical practice of MRI/CT scan for clinically moderate to high probability of suspected NOF fractures.
Imaging
All 41 patients had initial AP and lateral digital hip radiographs. The enrolled patients had radiographs showing no apparent NOF fractures. They went on to have a tomogram examination on a GE Definium 8000 system with VolumeRAD digital tomosynthesis (GE Healthcare, Chalfont St Giles, England), which was reviewed by a musculoskeletal consultant radiologist who is familiar with tomogram interpretation. There is a small learning curve to interpret the tomogram because the image interpretation has similarities to the old analogue tomography. Orthopaedic surgeons and A&E physicians can learn to interpret the tomogram easily as the imaging is done in the coronal plane similar to the plain radiographs.
Patients who had a confirmed NOF fracture on their tomogram examination were treated according to standard clinical practice for NOF fractures without additional imaging. Patients who had no obvious hip fracture on their tomogram examination were reassessed clinically by the referring orthopaedic surgeon and divided into two groups, one with moderate/high clinical probability of NOF fracture and second with low clinical probability of NOF fracture. Those patients who could not perform SLR (straight leg raise) and/or weight-bear were deemed to have moderate to high clinical probability of NOF fracture and went on to have additional imaging either MRI or CT scan. Patients who did not fit into the above criteria were considered to have low probability of NOF fracture. Patients who had no obvious hip fracture on their tomogram, along with low clinical suspicion of hip fractures, did not have further imaging. These patients were followed up for 6 months post-injury to identify any missed fractures (Fig. 1).
All patients with a negative tomogram but with moderate to high clinical probability of a NOF fracture had an MRI on GE Healthcare Optima 1.5-T system (GE Healthcare, Chalfont St Giles, England), with the exception of one patient who required a CT Scan on GE Healthcare Light Speed 64 slice system (GE Healthcare, Chalfont St Giles, England) using the standard low-dose pelvic bone protocol scan. In this case, MRI was contraindicated by the presence of a pacemaker. Initially, the MRI protocol was coronal and axial T1-weighted (T1W) and proton density (PD) fat-suppressed (FS) MRI sequences, although later in the trial only coronal T1W and PD FS scans were obtained because of the limited value of the axial scans. All MRI and CT scans were read by a consultant radiologist.
Results
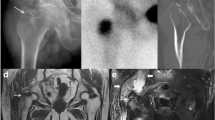
Forty-one patients with negative AP and lateral hip X-rays for fracture neck of femur following fall were prospectively included in the trial over 26-month period. All 41 patients underwent tomography, which identified six patients with fracture neck of femur (Fig. 2a, b). The remaining 35 patients were divided into two groups on repeat clinical examination.
From the first group of 15 patients with low probability of fracture neck of femur, four patients were found to have fractured pubic ramus or acetabulum (Fig. 3a, b) and one had fracture greater trochanter, as identified in tomogram. Ten patients did not have any fractures, and they were discharged home without any further imaging. In one patient, tomogram helped in excluding the NOF fracture suspected on plain X-ray. Fifteen patients were followed up for 6 months, and none of these patients had a missed injury.
All patients in the second group (20 patients) who had high probability of fracture NOF on clinical examination underwent MRI or CT within the next 48 h. One patient who had pacemaker and was not suitable for MRI had a CT scan, which identified undisplaced acetabulum fracture. Two patients in this group who had tomogram suggestive, but not conclusive of fracture neck of femur were confirmed to have fracture NOF on MRI (Fig. 4a–c). One patient who had greater trochanter fracture as identified on X-ray and tomogram was found to have intertrochanteric extension of fracture on MRI scan (Fig. 6a–c) and went on to have surgical intervention, while the remaining 17 patients (85 %) were identified as having either soft tissue injury (Fig. 5), undisplaced acetabulum fracture or pubic rami fracture to account for their signs and symptoms. Patient management in these 17 patients did not change secondary to the MRI findings.
With these initial results, the sensitivity of the tomogram for detecting occult neck of femur fractures is 67 % (95 % CI 30–92 %) with a specificity of 100 % (95 % CI 89–100 %) (Table 1; Fig. 6).
An 85-year-old female unable to weight-bear following a fall. Plain radiograph a did not show a fracture. DTS b of the right hip demonstrated break of the lateral cortex of the femoral neck base, with no intertrochanteric extension. MRI of the right hip T1W scan c demonstrated intertrochanteric fracture
Discussion
Confirmation or exclusion of the fracture neck of femur is very important as it changes the management of the patient with a history of fall and equivocal standard AP and lateral hip radiographs. The prevalence of occult hip fracture is estimated to be around 3–4 % and can be up to 9 % in some series [1]. Delay in the treatment for unidentified fracture neck femur can be devastating with a risk of increasing morbidity and mortality [1–4]. Identification of the undisplaced or impacted fracture neck of femur can be difficult and poses a diagnostic challenge, which needs further imaging. Previous studies summarised within recent NICE guidance have found MRI to have the highest accuracy (100 % sensitivity and 93–100 % specificity) depending on the skill and experience of the radiologist interpreting the images. If MRI is not available within 24 h or is contraindicated, CT scan is recommended based on current expert consensus [1]. Radionuclide bone scan (RNS) and ultrasound (US) scan are other modalities of investigations that can be used to diagnose the occult NOF fracture. However, both are not recommended within NICE guidance as they have low sensitivity and specificity [1].
In most UK hospitals, MRI scanning facility is not available out of hours or over the weekend. Even during normal working hours, it is not always possible to arrange the scan immediately for these patients requiring admission as an inpatient. One day cost as an inpatient in an acute bed is approximately £250. The cost of MRI scan is about £125. There has been increasing use of CT scans in cases of suspected NOF fracture in elderly [11, 27, 28]. Tomogram imaging shares a similar image acquisition system to CT scans, uses a significantly smaller dose of radiation, consumes less time and is potentially available in most hospitals. It is easier to learn to interpret tomograms in comparison with CT scans as the imaging is done in the coronal plane, similar to plain radiographs though there is a small learning curve required for the radiologists to interpret the tomograms.
The effective radiation dose is very low for tomogram imaging as compared to CT scanning, and it takes about 10 s to expose and obtain tomogram images. The effective dose for tomogram and conventional X-ray exposures was estimated from dose area product (DAP) values using PCXMC [29] Monte Carlo dose modelling software. The effective dose for the CT exposure was estimated from dose length product (DLP) values using the ImPACT CT Patient Dosimetry Calculator [30]. The tomogram of the hip joint resulted in about 1.2 times higher effective dose than that for conventional two-view hip X-rays and 16 times lower than that for the CT scan (Table 2).
There are some limitations to our study. The interpretation of the tomogram requires a small learning curve. The number of the patients involved in this pilot study is low, but the result is encouraging and would warrant a larger prospective multi-centre trial. The group of patients with low probability of fracture NOF did not have any radiological or clinical analysis to exclude the diagnosis of NOF fracture. This was assumed on survey of the radiological information system at 6 months as none of the patients in this group returned with a diagnosis of NOF fracture. Any of these patients could have gone to another hospital with a NOF fracture that would not necessarily have been reported back to this study.
All patients in our study underwent tomogram examination after inconclusive standard AP and lateral hip radiographs. Tomogram readily demonstrated fracture NOF in six patients who did not require further imaging. Tomogram also excluded neck of femur fracture in one patient which was suspected in plain X-rays. In the second group of patients, out of 20, MRI scan identified fracture neck of femur in three patients where the tomogram images were inconclusive but there was high clinical probability for fracture neck of femur.
As it is demonstrated in our study, tomogram can be used as a screening procedure with high specificity to reduce the need for resource-intensive imaging. When tomogram imaging is combined with further clinical assessment, low to moderate or high risk, the sensitivity improves to 100 % (95 % CI 66.2–100 %) and a specificity to 100 % (95 % CI 89.1–100 %). By using this system of acquiring a tomogram and additional clinical risk stratification, MRI or CT was avoided in 21 patients (51 %). This represents a significant resource saving and allows earlier confirmation or exclusion of the diagnosis of fracture NOF.
In conclusion, tomogram can readily be used for radiological assessment of suspected NOF fractures in patients with negative or equivocal plain film findings and to identify those patients who need additional cross-sectional imaging.
References
NICE.org.uk [clinical guideline CG124]. National Institute for Health and Care Excellence (2011) [updated Jun 2011; cited Mar 2014]. http://guidance.nice.org.uk/CG124
Boyce WJ, Vessey MP (1985) Rising incidence of fracture of the proximal femur. The Lancet 325(8421):150–151
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Smith P, Ariti C, Bardsley M (2013) Focus on hip fracture: trends in emergency admissions for fractured neck of femur, 2001 to 2011. The Health Foundation and the Nuffield Trust, London, pp 4–25
Hossain M, Akbar SA, Andrew G (2010) Misdiagnosis of occult hip fracture is more likely in patients with poor mobility and cognitive impairment. Acta Orthop Belg 76:341–346
Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH (1995) Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am 77:1551–1556
Dominguez S, Liu P, Roberts C, Mandell M, Richman PB (2005) Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs—a study of emergency department patients. Acad Emerg Med 12:366–369
Perron AD, Miller MD, Brady WJ (2002) Orthopedic pitfalls in the ED: radiographically occult hip fracture. Am J Emerg Med 20:234–237
Chiang CC, Wu HT, Lin CF et al (2012) Analysis of initial injury radiographs of occult femoral neck fractures in elderly patients: a pilot study. Orthopaedics 35(5):e621–e627
Göthlin JH, Geijer M (2013) The utility of digital linear tomosynthesis imaging of total hip joint arthroplasty with suspicion of loosening: a prospective study in 40 patients. Biomed Res Int 2013, Article ID 594631
Hakkarinen DK, Hanh KV, Hendey GW (2009) Magnetic resonance imaging identifies occult hip fractures missed by 64-slice computed tomography. J Emerg Med 37(2):144–152
Guanche CA, Kozin SH, Levy AS, Brody LA (1994) The use of MRI in the diagnosis of occult hip fractures in the elderly: a preliminary review. Orthopedics 17:327–330
Cooper C, Campion G, Melton Iii LJ (1992) Hip fractures in the elderly: a world-wide projection. Osteoporosis Int 2:285–289
Pandey R, McNally E, Ali A, Bulstrode C (1998) The role of MRI in the diagnosis of occult hip fractures. Injury 29:61–63
Chana R, Noorani A, Ashwood N, Chatterji U, Healy J, Baird P (2006) The Role of MRI in the diagnosis of proximal femoral fractures in the elderly. Injury 37(2):185–189
Hossain M, Barwick C, Sinha AK, Andrew JG (2007) Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury 38(10):1204–1208
Kirby M, Spritzer C (2010) Radiographic detection of hip and pelvic fractures in the emergency department. Am J Roentgenol 194:1054–1060
Oka M, Monu JU (2004) Prevalence and patterns of occult hip fractures and mimics revealed by MRI. Am J Roentgenol 182(2):283–288
Galloway HR, Meikle GR, Despois M (2004) Patterns of injury in patients with radiographic occult fracture of neck of femur as determined by magnetic resonance imaging. Australas Radiol 48(1):21–24
Collin D, Dunker D, Göthlin JH, Geijer M (2011) Observer variation for radiography, computed tomography, and magnetic resonance imaging of occult hip fractures. Acta Radiol 52(8):871–874
Hakkarinen DK, Banh KV, Hendey GW (2012) Magnetic resonance imaging identifies occult hip fractures missed by 64-slice computed tomography. J Emerg Med 43(2):303–307
Fairclough J, Colhoun E, Johnston D, Williams LA (1987) Bone scanning for suspected hip fractures. A prospective study in elderly patients. J Bone Joint Surg Br 69(2):251–253
Evans PD, Wilson C, Lyons K (1994) Comparison of MRI with bone scanning for suspected hip fracture in elderly patients. J Bone Joint Surg Br 76(1):158–159
Geijer M, Börjesson AM, Göthlin JH (2011) Clinical utility of tomosynthesis in suspected scaphoid fracture. A pilot study. Skeletal Radiol 40(7):863–867
Machida H, Yuhara T, Sabol JM, Tamura M, Shimada Y, Ueno E (2011) Postoperative follow-up of olecranon fracture by digital tomosynthesis radiography. Jpn J Radiol 29(8):583–586
Ottenin MA, Jacquot A, Grospretre O et al (2012) Evaluation of the diagnostic performance of tomosynthesis in fractures of the wrist. Am J Roentgenol 198(1):180–186
Heikal S, Riou P, Jones L (2014) The use of computed tomography in identifying radiologically occult hip fractures in the elderly. Ann R Coll Surg Engl 96(3):234–237
Jordan R, Dickenson E, Westacott D, Baraza N, Srinivasan K (2012) A vast increase in the use of CT scans for investigating occult hip fractures. J Emerg Med 43(2):303–307
PCXMC 2.0: A PC-based Monte Carlo program for calculating patient doses in medical X-ray examinations; www.stuk.fi/sateilyn-hyodyntaminen/ohjelmat/PCXMC/en_GB/pcmxc/
Impact CT patient dosimetry calculator, Version 2011: www.impactscan.org/index.htm
Acknowledgments
The authors would like to thank following persons for their suggestions and support during the study and review of the article. Mr. M. Floyd, Mr. I. Mcllquham, Mr. G. Brunst, Mr. J. Sabol, Dr. S. Phillips, Mr. Anthony G. Martin. The authors would also like to thank the two anonymous reviewers for their helpful and constructive comments.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical standard
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All the laws of UK in this regard have been observed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Namir Al-Mokhtar and Jaydeep Shah have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Al-Mokhtar, N., Shah, J., Marson, B. et al. Initial clinical experience of the use of digital tomosynthesis in the assessment of suspected fracture neck of femur in the elderly. Eur J Orthop Surg Traumatol 25, 941–947 (2015). https://doi.org/10.1007/s00590-015-1632-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1632-3