Abstract
Objective
To compare the diagnostic value of indirect magnetic resonance arthrography (I-MRA) with that of direct MR arthrography (D-MRA) for labral tears, rotator cuff tears, and long head of biceps tendon (LHBT) tears using a 3-T MR unit.
Materials and methods
Institutional review board approval was given; written informed consent was obtained from all patients. From November 2005 to June 2006, 19 patients (eight men and 11 women; mean age, 51 years) who had undergone both I-MRA and D-MRA underwent arthroscopic surgery. Both methods were performed in fat-saturated axial, coronal oblique, and sagittal oblique T1-weighted sequences, as well as axial and coronal oblique T2-weighted sequences. Two radiologists independently and retrospectively evaluated two sets of MRA for the diagnosis of superior and anterior labral tears, subscapularis tendon (SSC), and supraspinatus–infraspinatus tendon (SSP–ISP) tears, and LHBT tears. With the arthroscopic finding as a gold standard, we analyzed statistical differences of sensitivities and specificities between two sets of MRA and inter-observer agreement was evaluated using the kappa value.
Results
The sensitivity and specificity of I-MRA and D-MRA for reader 1 were 79/80% and 71/80%, respectively, for superior labral tears; 100/100% and 100/100%, respectively, for anterior labral tears; 64/75% and 64/100%, respectively, for SSC tears; 100/86% and 100/100%, respectively, for SSP–ISP tears; and 67/100% and 78/100%, respectively, for LHBT tears. Those of I-MRA and D-MRA for reader 2 were 86/80% and 71/100%, respectively, for superior labral tears; 100/83% and 100/100%, respectively, for anterior labral tears; 64/88% and 82/100%, respectively, for SSC tears; 92/86% and 100/100%, respectively, for SSP–ISP tears; and 78/90% and 89/100%, respectively, for LHBT tears. No significant differences were found between the methods. Inter-observer agreements were higher than moderate (κ > 0.41) with both methods.
Conclusions
Based on a relatively small number of patients, no significant difference was detected between I-MRI and D-MRI with regard rotator cuff, labral, and LHBT tears.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Direct magnetic resonance arthrography (D-MRA) of the shoulder has been widely used to evaluate abnormalities of the labroligamentous complex and rotator cuff [1–7]. However, this method is mildly invasive as it exposes patients to ionizing radiation with intra-articular needle placement for joint injection using fluoroscopic guidance [8]. Also, it requires the coordination of scheduling two procedure rooms, which becomes impractical if the fluoroscopy suite is distant from the MRI scanner [8]. It has been shown that the intravenous administration of gadopentetate dimeglumine enhances the joint cavity and thus indirectly produces an arthrographic effect [9–11]. This technique, which is known as indirect MRA (I-MRA), was proposed as a practical alternative to D-MRA [10]. However, to our knowledge, there are no studies in the literature regarding the diagnostic accuracy of labral lesions, rotator cuff tears, and long head of biceps tendon (LHBT) tears using I-MRA compared to D-MRA. The purpose of our study was to compare the diagnostic accuracy of I-MRA to D-MRA with respect to anterior and superior labral tears, subscapularis (SSC) tears, supra- and infraspinatus complex (SSP–ISP) tears, and LHBT tears on a 3-T MR unit.
Materials and methods
Patients
The institutional review board approved this study protocol, and written informed consent was obtained from all patients. From November 2005 to June 2006, 19 symptomatic patients who had undergone D-MRA and planned to undergo arthroscopic surgery of the ipsilateral shoulder at our institution were enrolled in this study. None of the patients had previously undergone surgery on the symptomatic shoulder. All patients underwent I-MRA 1 day before arthroscopic surgery to compare the diagnostic accuracy of I-MRA to D-MRA in the diagnosis of superior and anterior labral tears, SSC tears, SSP–ISP tears, and LHBT tears. D-MRA was performed within 190 days of arthroscopic surgery (mean time interval, 78 days). The patient group included eight men (age range, 25–71 years; mean age, 48.6 years) and 11 women (age range, 27–77 years; mean age, 56.0 years). Five patients presented with recurrent shoulder dislocation, and the remaining 14 patients presented with shoulder pain and motion limitation.
MR imaging protocol
According to the clinical standard protocol of D-MRA, joint injection was performed using an anterior approach with fluoroscopic guidance by the radiologists. A 23-gauge spinal needle was placed in the glenohumeral joint, and 1–3 cc of iohexol (Omnipaque 300 mg/ml, Amersham Health AS, Oslo, Norway) was used to verify the intra-articular injection. A maximum of 15 ml of gadobutrol (Gadovist; Schering AG, Berlin, Germany) at a concentration of 1.0 mol/l diluted 1:250 in normal saline was injected. MR imaging was initiated within 60 min of the intra-articular injection. I-MRA was initiated after intravenous gadolinium injection of gadobutrol (Gadovist; Schering AG, Berlin, Germany; 0.1 mmol/kg body weight) into an antecubital vein. Immediately after the injection of contrast material, patients were instructed to move their shoulder for 15 min.
Both I-MRA and D-MRA were obtained using the following imaging parameters. Fat-suppressed T1-weighted fast spin-echo sequences were obtained in the axial plane (repetition time/echo time [TR/TE], 434–565/18–24 ms; section thickness, 3 mm; field of view [FOV], 15 cm; matrix size, 224/224) and the coronal oblique plane, parallel to the long axis of the supraspinatus tendon (TR/TE, 434–565/20–24 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 224/224) and in the sagittal oblique plane, perpendicular to the long axis of the supraspinatus tendon (TR/TE, 434–561/18–24 ms; section thickness, 4 mm; FOV, 15 cm; matrix size, 224/224). T2-weighted fast spin-echo sequences were obtained in the axial plane (TR/TE, 2,868–3,184/80 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 224/224) and the coronal oblique plane (TR/TE, 2,661–2,906/80 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 256/256). The total scan time was 16 min and 40 s.
Analysis of MR images
MR images were independently and retrospectively analyzed by an experienced musculoskeletal radiologist (Y.C.Y, with 6 years of experience in musculoskeletal MR imaging) and a fellowship-trained musculoskeletal radiologist (J.Y.J, with 1 year and 6 months of experience in musculoskeletal MR imaging) who were blind to the arthroscopy results. The two readers evaluated two sets of MRAs in 2-week intervals. Images were presented in random order at each reading session and evaluated using a picture archiving and communication system (Centricity Radiology RA 1000; General Electric Healthcare, Chicago, IL, USA). The presence or absence of superior and anterior labral tears, SSC tears, SSP–ISP tears, and LHBT tears on all MR images was evaluated.
The MR arthrographic findings of the SSP–ISP and the SSC tendon were classified as no tear, full-thickness tear, or partial-thickness tear. A full-thickness tear was diagnosed if there was high signal intensity involving the entire thickness and tendinous discontinuity with or without retraction of the musculotendinous junction on both T1- and T2-weighted images [1, 12]. A partial-thickness tear of the tendon was diagnosed when a focus of high signal intensity involving either the bursal or the articular surface of the tendon was apparent with surface abnormalities without complete discontinuity of the tendon [1]. For statistical analysis, no attempt was made to differentiate between the types of tears.
The LHBT tears were diagnosed by identifying the presence of an increased intra-substance signal intensity abnormality on both T1- and T2-weighted images or by identifying attenuation or disruption of the tendon [13].
The criteria used to define superior and anterior labral tears were as follows [14–18]: absence, truncation, or fragmentation of the labrum (not meeting criteria for a sublabral recess or foramen at superior labrum); displacement of the labrum from its expected anatomic location; surface irregularity; increased signal intensity (or contrast enhancement) extending to its surface; and identification of contrast material extending into a linear or complex tear cleft within the labrum on D-MRA. When a tear involved both entire superior and anterior-inferior portion of the labrum regardless of its continuity, we regarded it as concomitant superior and anterior labral tears.
For avoiding the magic angle artifacts, when the signal intensity of posterior-superior labrum and critical portion of SSP tendon was increased mildly and indistinctively on T1-weighted sequences, the signal intensity of T2-weighted sequences was regarded as standard for decision.
The arthroscopic finding was regarded as the reference standard. Arthroscopic surgery was performed by one orthopedic surgeon (J.Y.) with 6 years of experience in shoulder surgery. He examined both the subacromial–subdeltoid space and glenohumeral joint routinely by using posterior, anterior portal, and lateral portals.
Statistical analysis
Sensitivity and specificity with their 95% confidence intervals were calculated using a website (http://faculty.vassar.edu/lowry/prop1.html). Agreement between the two readers (inter-observer agreement) in evaluating the D-MRA and I-MRA findings was calculated using κ statistics. Inter-observer agreement is rated as poor for a κ value of less than or equal to 0.20, fair for a κ value of 0.21–0.40, moderate for a κ value of 0.41–0.60, good for a κ value of 0.61–0.80, and excellent for a κ value of 0.81–1.00 [19].
Results
Arthroscopic surgery
Arthroscopic surgery revealed the presence of 14 superior labral tears, seven anterior labral tears, nine LHBT tears (three complete tears, six partial tears), 12 SSP–ISP tears (eight full-thickness tears, one articular-sided partial-thickness tear, three bursal-sided partial-thickness tears), and 11 SSC tears (11 partial-thickness tears).
Diagnostic accuracy
For readers 1 and 2, sensitivity and specificity values with 95% confidence intervals (Tables 1 and 2) for the diagnosis of superior and anterior labral tears, LHBT tears, SSP–ISP tears, and SSC tears using D-MRA and I-MRA were not statistically different.
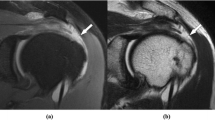
Both readers correctly diagnosed ten of the 14 superior labral tears using D-MRA (Fig. 1). Reader 1 correctly diagnosed 11 lesions and reader 2 correctly diagnosed 12 lesions using I-MRA. Among arthroscopically proven superior labral tears, two lesions on D-MRA (Fig. 2), one lesion on I-MRA, and two lesions on both I-MRA and D-MRA were missed by reader 1, and two lesions on the D-MRA and two lesions on both I-MRA and D-MRA were missed by reader 2. One false positive case for reader 1 was generated by D-MRA, and two false positive cases for both readers were generated by I-MRA.
An arthroscopically proven superior labral tear of the left shoulder in a 70-year-old woman was correctly diagnosed by both MRAs according to two readers. Fat-suppressed T1-weighted fast spin-echo axial images show interposition of contrast media on the D-MRA (a, arrow) and a contrast-enhanced cleft on the I-MRA (b, arrow) between the superior portion of the glenoid labrum and the bony glenoid. T2-weighted fast spin-echo coronal oblique imaging of the D-MRA (c) shows a high signal intensity cleft in the superior portion of the glenoid labrum (arrow)
An arthroscopically proven superior labral tear of the left shoulder in a 43-year-old woman was correctly diagnosed by I-MRA only by reader 1. Fat-suppressed T1-weighted fast spin-echo coronal oblique imaging on the D-MRA (a) shows a normal appearance of the superior portion of the glenoid labrum. Fat-suppressed T1-weighted fast spin-echo coronal oblique imaging on the I-MRA (b) shows linear contrast enhancement (arrow) at the superior portion of the glenoid labrum
All anterior labral tears were correctly diagnosed by both readers using both MRAs (Fig. 3). Two false positive cases for reader 2 were generated by I-MRA only.
An arthroscopically proven anterior labral tear of the right shoulder in a 57-year-old man was correctly diagnosed by both MRAs by both readers. Fat-suppressed T1-weighted fast spin-echo axial imaging of the D-MRA (a) shows interposition of contrast media between the anterior portion of the glenoid labrum and the bony glenoid (arrow). Fat-suppressed T1 weighted fast spin-echo axial imaging of the I-MRA (b) shows linear contrast enhancement between the anterior portion of the glenoid labrum and the bony glenoid (arrow)
Reader 1 correctly diagnosed seven of the 11 SSC tears and reader 2 correctly diagnosed nine of the 11 SSC tears using D-MRA. Meanwhile, both reader 1 and reader 2 correctly diagnosed seven SSC tears using I-MRA. Among arthroscopically proven SSC tears, two lesions on D-MRA, two lesions on I-MRA, and two lesions on both I-MRA and D-MRA were missed by reader 1, while one lesion on D-MRA, three lesions on I-MRA, and one lesion on both I-MRA and D-MRA were missed by reader 2. Two false positive cases for reader 1 and one false positive case for reader 2 were generated by I-MRA.
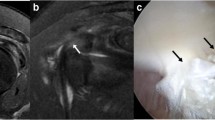
Reader 1 correctly diagnosed seven of the nine LHBT tears and reader 2 correctly diagnosed eight lesions using D-MRA. Reader 1 correctly diagnosed six lesions and reader 2 correctly diagnosed seven lesions using I-MRA. Among arthroscopically proven LHBT tears, one lesion on D-MRA (Fig. 4), two lesions on I-MRA and one lesion on both D-MRA and I-MRA were missed by reader 1, while one lesion on I-MRA and one lesion on both D-MRA and I-MRA were missed by reader 2. One false positive LHBT tear was generated by I-MRA for reader 2.
An arthroscopically proven complete tear of the long head of the biceps tendon of the left shoulder in a 76-year-old woman was correctly diagnosed on both MRAs by reader 2 and on I-MAR by reader 1 but was missed by D-MRA by reader 1. Fat-suppressed T1-weighted fast spin-echo axial images on the D-MRA (a) and the I-MRA (b) show medial subluxation of attenuated LHBT (arrows)
All cases of SSP–ISP tears were correctly diagnosed by reader 1 using both D-MRA and I-MRA. One arthroscopically proven SSP–ISP tear was missed on I-MRA by reader 2, while D-MRA yielded entirely correct diagnoses. One false positive case of SSP–ISP tear was generated by I-MRA for each reader (Fig. 5). All cases of full-thickness tears were correctly diagnosed by both readers on both MRAs (Fig. 6). One arthroscopically proven articular-sided partial-thickness tear was correctly diagnosed by both MRAs for reader 1 and by D-MRA for reader 2. Two of three bursal-sided partial-thickness tears for reader 1 and three lesions for reader 2 were correctly diagnosed by both MRAs. One arthroscopically proven bursal-sided partial-thickness tear was missed on both MRAs by reader 1.
An arthroscopically proven calcific tendinitis of SSP–ISP without tear of the left shoulder in a 46-year-old woman was misinterpreted as a bursal-sided partial-thickness tear of SSP–ISP on I-MRA by two readers. Fat-suppressed T1-weighted fast spin-echo coronal oblique image on the D-MRA (a) shows intact SSP–ISP. Fat-suppressed T1-weighted fast spin-echo coronal oblique images on the I-MRA (b, c) show contrast enhancement of mainly bursal-sided SSP–ISP (b, arrow) and a calcification with surrounding enhanced tissue (c, arrow)
An arthroscopically proven full-thickness tear of SSP–ISP of the right shoulder in a 77-year-old woman was correctly diagnosed on both MRAs by both readers. Fat-suppressed T1-weighted fast spin-echo coronal oblique images on the D-MRA (a) and the I-MRA (b) show a tendinous discontinuity with retraction of the musculotendinous junction at SSP–ISP (arrows)
Inter-observer agreement
Inter-observer agreement was best for the evaluation of SSP–ISP tears and anterior labral tears with the use of D-MRA (κ value = 1.00, Table 3). Inter-observer agreement was worst for the evaluation of SSC tears with the use of I-MRA (κ value = 0.47, Table 3). Inter-observer agreement was higher than moderate agreement for all lesions on both MRAs.
Discussion
I-MRA is based on the premise that intravenous contrast material will diffuse into the joint space over time, so that arthrography-like T1-weighted images can be obtained. The intravascular paramagnetic contrast material that leaks from the capillary bed into interstitial space and diffuses from the synovium into the joint space is responsible for the arthrographic effect of the intravenous technique. The rate and amount of diffusion are increased by any exercise of the joint after injection [10, 20]. Several advantages of I-MRA over D-MRA are that intra-articular injection under fluoroscopic guidance is not required and that imaging can be performed during off hours or offsite [8].
In a previous study, the sensitivity and specificity of the detection of rotator cuff tears using I-MRA were reported as 100% and 78–89%, respectively [21]. Moreover, another study employing I-MRA reported the sensitivity and specificity of full-thickness rotator cuff tears to be 80–95% and 100%, respectively, and those for partial-thickness rotator cuff tears to be 50–71% and 88%, respectively [22]. Additionally, sensitivity and specificity using conventional MRI for full-thickness tears of rotator cuff were reported as 89% and 93%, and those for partial-thickness tears of the rotator cuff were reported to be 44% and 90% [23]. For diagnosis of full-thickness tears of the rotator cuff using D-MRA, the previously reported sensitivity and specificity were 96% and 99%, respectively, while those for articular-sided partial-thickness tears were 80–84% and 96–97%, respectively [24, 25]. In a previous report, the sensitivity was 91% and the specificity was 86% for the detection of SSC tendon tears using D-MRA [26]. In our results, the sensitivity and specificity of SSP–ISP tears and the specificity of SSC tears using I-MRA and D-MRA were comparable to the published data, aside from our sensitivity of SSC tears using D-MRA (64% for reader 1, 82% for reader 2) which was lower than that of previous reports. The reported sensitivity and specificity for detecting LHBT tears using D-MRA are 71–86% and 86–97%, respectively, [27] and 52% and 86%, respectively, when using unenhanced MRI [13]. To our knowledge, no data exist regarding the diagnostic accuracy of I-MRA for assessing LHBT tears. Using I-MRA and D-MRA, the sensitivity and specificity for detecting LHBT tears in our results were comparable to the published data, except for the sensitivity when using I-MRA for reader 1. For the diagnosis of superior labral lesions using I-MRA, the reported sensitivity and specificity are 84–91% and 58–71%, respectively [28]. In previous reports, D-MRA showed a sensitivity of 82–89% and a specificity of 90–99% for the overall detection of superior labral anterior–posterior (SLAP II–IV) lesions [29–31], and a sensitivity of 88–96% and a specificity of 91–100% for the detection of anterior labral pathology [32–34]. In our results, the sensitivity and specificity of anterior labral tears when using D-MRA and I-MRA were comparable to the published data. Furthermore, the sensitivity and specificity of superior labral tears were comparable to the published data, except for the sensitivity of both MRAs for reader 1, the sensitivity of D-MRA for reader 2, and the specificity of D-MRA for reader 1. However, this could be due to the small number of lesions. Among false negative cases, one arthroscopically proven superior labral tear with a co-existing anterior labral tear was interpreted as an anterior labral tear with superior extension on both D-MRA and I-MRA by both readers. Among false positive cases, reader 1 interpreted a sublabral recess as a labral tear on D-MRA, and one case that was arthroscopically proven as SLAP I lesions was interpreted as labral tears by I-MRA for both readers.
The magic angle effect may be responsible for false positive results in the evaluation of the SSP and the superior labrum. However, this effect was identical for both I-MRA and D-MRI.
Contrary to D-MRI, in I-MRA, not only the glenohumeral joint space is enhanced but also all structures covered by a synovial membrane [35]. As a consequence, contrast material in the subacromial–subdeltoid bursa cannot be considered an indirect sign of a full-thickness tear on I-MRA, and this makes it easier to delineate bursal-sided partial tears [36]. Another difference is that every abnormality or vascularized structure will enhance on I-MRA [37]. Therefore, the correct interpretation of an area of increased signal intensity within the tendon can be problematic, because the same signal intensity can be caused by tendinopathy or enhancement of fibrovascular tissue in a partial tear [10, 21]. In a false positive case, the rotator cuff may be enhanced because of inflammation or granulation tissue and scarring. In our results, false positive cases on I-MRA were seen more often than those on D-MRA with regards to the detection of SSC tears. Also, one false positive diagnosis of a bursal-sided partial-thickness tear was made by both readers based on I-MRA though this may have been due to underlying calcific tendinitis. A potential challenge in the diagnostic interpretation of I-MRA is determining whether labral enhancement reflects normal vascularity, degenerative changes, or an underlying injury [38]. In addition, structures that depend on distention for visualization—in particular, the labrum—are poorly seen [39]. In our results, false positive cases on I-MRA were more abundant than those on D-MRA for the detection of superior and anterior labral tears for reader 2.
Study limitations include, first of all, the relatively small number of patients. In addition, there was a possible bias because patients were included based on the fact that arthroscopy had been performed. Also, the radiologists evaluating the images were aware that the patients had undergone arthroscopy. The time interval between D-MRI and surgery was far longer than the time elapsed between I-MRI and surgery. The fact that T2-weighted images were available may have masked differences between D-MRI and I-MRI. However, this reproduces the situation of routine work.
In conclusion, based on a relatively small number of patients, no significant difference was detected between I-MRI and D-MRI with regard rotator cuff, labral, and LHBT tears.
References
Hodler J, Kursunoglu-Brahme S, Snyder SJ, et al. Rotator cuff disease: assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology 1992; 182: 431–436.
Chandnani VP, Gagliardi JA, Murnane TG, et al. Glenohumeral ligaments and shoulder capsular mechanism: evaluation with MR arthrography. Radiology 1995; 196: 27–32.
Massengill AD, Seeger LL, Yao L, et al. Labrocapsular ligamentous complex of the shoulder: normal anatomy, anatomic variation, and pitfalls of MR imaging and MR arthrography. Radiographics 1994; 14: 1211–1223.
Beltran J, Rosenberg ZS, Chandnani VP, Cuomo F, Beltran S, Rokito A. Glenohumeral instability: evaluation with MR arthrography. Radiographics 1997; 17: 657–673.
Park YH, Lee JY, Moon SH, et al. MR arthrography of the labral capsular ligamentous complex in the shoulder: imaging variations and pitfalls. AJR Am J Roentgenol 2000; 175: 667–672.
Shankman S, Bencardino J, Beltran J. Glenohumeral instability: evaluation using MR arthrography of the shoulder. Skeletal Radiol 1999; 28: 365–382.
Palmer WE, Brown JH, Rosenthal DI. Rotator cuff: evaluation with fat-suppressed MR arthrography. Radiology 1993; 188: 683–687.
Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics 2002; 22: 1223–1246.
Winalski CS, Aliabadi P, Wright RJ, Shortkroff S, Sledge CB, Weissman BN. Enhancement of joint fluid with intravenously administered gadopentetate dimeglumine: technique, rationale, and implications. Radiology 1993; 187: 179–185.
Vahlensieck M, Peterfy CG, Wischer T, et al. Indirect MR arthrography: optimization and clinical applications. Radiology 1996; 200: 249–254.
Drape JL, Thelen P, Gay-Depassier P, Silbermann O, Benacerraf R. Intraarticular diffusion of Gd-DOTA after intravenous injection in the knee: MR imaging evaluation. Radiology 1993; 188: 227–234.
Schweitzer ME, Magbalon MJ, Fenlin JM, Frieman BG, Ehrlich S, Epstein RE. Effusion criteria and clinical importance of glenohumeral joint fluid: MR imaging evaluation. Radiology 1995; 194: 821–824.
Beall DP, Williamson EE, Ly JQ, et al. Association of biceps tendon tears with rotator cuff abnormalities: degree of correlation with tears of the anterior and superior portions of the rotator cuff. AJR Am J Roentgenol 2003; 180: 633–639.
Cartland JP, Crues JV 3rd, Stauffer A, Nottage W, Ryu RK. MR imaging in the evaluation of SLAP injuries of the shoulder: findings in 10 patients. AJR Am J Roentgenol 1992; 159: 787–792.
Legan JM, Burkhard TK, Goff WB 2nd, et al. Tears of the glenoid labrum: MR imaging of 88 arthroscopically confirmed cases. Radiology 1991; 179: 241–246.
Probyn LJ, White LM, Salonen DC, Tomlinson G, Boynton EL. Recurrent symptoms after shoulder instability repair: direct MR arthrographic assessment—correlation with second-look surgical evaluation. Radiology 2007; 245: 814–823.
Smith DK, Chopp TM, Aufdemorte TB, Witkowski EG, Jones RC. Sublabral recess of the superior glenoid labrum: study of cadavers with conventional nonenhanced MR imaging, MR arthrography, anatomic dissection, and limited histologic examination. Radiology 1996; 201: 251–256.
De Maeseneer M, Van Roy F, Lenchik L, et al. CT and MR arthrography of the normal and pathologic anterosuperior labrum and labral–bicipital complex. Radiographics 2000;20 Spec No:S67-81.
Seigel DG, Podgor MJ, Remaley NA. Acceptable values of kappa for comparison of two groups. Am J Epidemiol 1992; 135: 571–578.
Vahlensieck M, Sommer T, Textor J, et al. Indirect MR arthrography: techniques and applications. Eur Radiol 1998; 8: 232–235.
Yagci B, Manisali M, Yilmaz E, et al. Indirect MR arthrography of the shoulder in detection of rotator cuff ruptures. Eur Radiol 2001; 11: 258–262.
Herold T, Bachthaler M, Hamer OW, et al. Indirect MR arthrography of the shoulder: use of abduction and external rotation to detect full- and partial-thickness tears of the supraspinatus tendon. Radiology 2006; 240: 152–160.
Shahabpour M, Kichouh M, Laridon E, Gielen JL, De Mey J. The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. Eur J Radiol 2008; 65: 194–200.
Waldt S, Bruegel M, Mueller D, et al. Rotator cuff tears: assessment with MR arthrography in 275 patients with arthroscopic correlation. Eur Radiol 2007; 17: 491–498.
Meister K, Thesing J, Montgomery WJ, Indelicato PA, Walczak S, Fontenot W. MR arthrography of partial thickness tears of the undersurface of the rotator cuff: an arthroscopic correlation. Skeletal Radiol 2004; 33: 136–141.
Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology 1999; 213: 709–714.
Zanetti M, Weishaupt D, Gerber C, Hodler J. Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography. AJR Am J Roentgenol 1998; 170: 1557–1561.
Dinauer PA, Flemming DJ, Murphy KP, Doukas WC. Diagnosis of superior labral lesions: comparison of noncontrast MRI with indirect MR arthrography in unexercised shoulders. Skeletal Radiol 2007; 36: 195–202.
Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, Woertler K. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR Am J Roentgenol 2004; 182: 1271–1278.
Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology 2001; 218: 127–132.
Bencardino JT, Beltran J, Rosenberg ZS, et al. Superior labrum anterior–posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology 2000; 214: 267–271.
Palmer WE, Caslowitz PL. Anterior shoulder instability: diagnostic criteria determined from prospective analysis of 121 MR arthrograms. Radiology 1995; 197: 819–825.
Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 2005; 237: 578–583.
Palmer WE, Brown JH, Rosenthal DI. Labral–ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology 1994; 190: 645–651.
Carrino JA, Smith DK, Schweitzer ME. MR arthrography of the elbow and wrist. Semin Musculoskelet Radiol 1998; 2: 397–414.
Vahlensieck M, Sommer T. Indirect MR arthrography of the shoulder. An alternative to direct MR arthrography? Radiologe 1996; 36: 960–965.
Burstein D, Velyvis J, Scott KT, et al. Protocol issues for delayed Gd(DTPA)(2-)-enhanced MRI (dGEMRIC) for clinical evaluation of articular cartilage. Magn Reson Med 2001; 45: 36–41.
Kreitner KF, Botchen K, Rude J, Bittinger F, Krummenauer F, Thelen M. Superior labrum and labral–bicipital complex: MR imaging with pathologic–anatomic and histologic correlation. AJR Am J Roentgenol 1998; 170: 599–605.
Wagner SC, Schweitzer ME, Morrison WB, Fenlin JM Jr, Bartolozzi AR. Shoulder instability: accuracy of MR imaging performed after surgery in depicting recurrent injury—initial findings. Radiology 2002; 222: 196–203.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jung, J.Y., Yoon, Y.C., Yi, SK. et al. Comparison study of indirect MR arthrography and direct MR arthrography of the shoulder. Skeletal Radiol 38, 659–667 (2009). https://doi.org/10.1007/s00256-009-0660-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-009-0660-7