Abstract
Objectives
To compare the accuracy of indirect magnetic resonance arthrography and noncontrast magnetic resonance imaging for diagnosing rotator cuff tears.
Materials and methods
In total, 333 patients who underwent noncontrast magnetic resonance imaging or indirect magnetic resonance arthrography were included retrospectively. Two musculoskeletal radiologists evaluated the images for the presence of supraspinatus-infraspinatus and subscapularis tendon tears. The overall diagnostic performance was calculated using the arthroscopic findings as the reference standard. Statistical differences between the diagnostic performances of the two methods were analyzed.
Results
Ninety-six and 237 patients who underwent noncontrast magnetic resonance imaging and indirect magnetic resonance arthrography were assigned into groups A and B, respectively. Sensitivity for diagnosing articular-surface partial-thickness supraspinatus-infraspinatus tendon tear was slightly higher in group B than in group A. Statistical significance was confirmed by multivariate analysis using the generalized estimating equation (p = 0.046). The specificity for diagnosing subscapularis tendon tear (85 % vs. 68 %, p = 0.012) and grading accuracy (57 % vs. 40 %, p = 0.005) was higher in group B than in group A; the differences were statistically significant for one out of two readers. Univariate analysis using the generalized estimating equation showed that the accuracy for diagnosing subscapularis tendon tear in group B was higher than in group A (p = 0.042). There were no statistically significant differences between the diagnostic performances of both methods for any other parameters.
Conclusion
Indirect magnetic resonance arthrography may facilitate more accurate diagnosis and grading of subscapularis tendon tears compared with noncontrast magnetic resonance imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Following its initial description by Winalski [1] and Drape [2] in 1993, indirect magnetic resonance (MR) arthrography has been used for the diagnosis of intra-articular abnormalities without invasive procedures and coordination of additional scheduling [3–8]. Since it produces arthrogram-like effects, several investigators have emphasized that indirect MR arthrography may have the potential to replace direct MR arthrography for the evaluation of shoulder pathologies [3, 8]. A comparison study revealed that there was no significant difference between indirect and direct MR arthrography with regard to rotator cuff, labral, and long head of biceps tendon tears [9]. When compared with noncontrast MR imaging (MRI), a number of authors have observed improved sensitivity in the diagnosis of glenoid labral lesions with indirect MR arthrography in a relatively small number of populations [6, 10, 11]. Although there have been several reports concerning the diagnostic performance of indirect MR arthrography for rotator cuff tears [4, 12–15], the incremental value of intravenous paramagnetic contrast media injection for the diagnosis of rotator cuff tears in comparison with noncontrast MRI remains unclear. Therefore, the purpose of this study was to compare the diagnostic accuracy of indirect MR arthrography with that of noncontrast MRI for the diagnosis of rotator cuff lesions in a large population using a 3.0 T MR scanner.
Materials and methods
Patients
This retrospective study was approved by the institutional review board of our institution and the requirement for patient informed consent was waived. Medical and arthroscopic surgical records were available for a total of 420 consecutive patients who underwent arthroscopic surgery after noncontrast MRI or indirect MR arthrography evaluation for shoulder discomfort, between March 2011 and September 2013. At our institution, patients who are suspected of having rotator cuff lesions based on clinical history or physical examination undergo noncontrast MRI or indirect MR arthrography. Indirect MR arthrography was performed according to our orthopedic surgeon’s policy if the initial outside hospital’s MR image was of poor quality, or if it was examined more than 6 months ago, or if the surgery was planned on the following day. Among these patients, 68 were excluded because the interval between the MRI and arthroscopic surgery exceeded 30 days. Seventeen patients with a history of previous surgery on the ipsilateral shoulder and two patients who underwent surgery for infection were also excluded. Consequently, a total of 333 patients with shoulder MR examinations were included in this study; 96 and 237 patients who had undergone noncontrast MRI and indirect MR arthrography were assigned into groups A and B, respectively. Group A was comprised of 46 men (age range, 22–80 years; mean age, 55.6 years) and 50 women (age range, 29–74 years; mean age, 61.4 years), while group B was comprised of 114 men (age range, 17–77 years; mean age, 51.0 years) and 123 women (age range, 21–78 years; mean age, 61.0 years). The mean interval between MR examination and arthroscopic surgery was 9 days for group A (range, 0–29 days) and less than 1 day for group B (range, 0–23 days). Primary patient complaints were shoulder pain with or without limitation of movement, shoulder dislocation, and motor weakness.
MRI protocol
All MR examinations were performed on 3.0 T scanners (Gyroscan Intera Achieva, Philips Medical Systems, Best, The Netherlands) with a dedicated receive-only shoulder coil. Patients were positioned with their humerus in a neutral position and their thumb pointing upward. For noncontrast MRI, axial gradient echo sequence using summated multi-echo fast-field-echo technique with three echoes, proton density-weighted fat-saturated fast spin-echo (FSE) images in the axial and oblique coronal planes, T2-weighted (T2W) FSE sequences in the oblique coronal and oblique sagittal planes were obtained. For indirect MR arthrography, 0.1 mmol/kg of gadopentetate dimeglumine (Gd-DTPA, Magnevist, Bayer Schering Pharma AG, Berlin, Germany) was injected into the antecubital vein. Immediately after the injection of contrast material, patients were instructed to exercise their shoulder for 15 min. Following this, fat-saturated T1-weighted (T1W) and T2W FSE sequences in the axial, oblique coronal, and oblique sagittal planes were obtained. Table 1 shows MRI protocol details. Total imaging times were 19 min 8 s and 23 min 46 s for noncontrast MRI and indirect MR arthrography, respectively.
Image analysis
All MR images were analyzed independently and retrospectively by two radiologists with 10 and 7 years of experience in musculoskeletal MRI and who were blinded to the arthroscopic results. As supraspinatus (SSP) and infraspinatus (ISP) tendons overlap and fuse together on their footprints [16–18], we used combined assessment of SSP and ISP tendon tears together to improve the accuracy of correlation between MR and arthroscopic findings. The readers evaluated the presence of SSP-ISP tendon tears and subscapularis (SSC) tendon tears. A three-point scale was used for the grading of SSP-ISP tendons: 0, no tear; 1, partial-thickness tear; and 2, full-thickness tear. A partial-thickness tear was further classified as an articular- or bursal-surface tear. Similarly, the SSC tendons were graded using a five-point scale according to Yoo and Rhee classification [19] as follows: 0, normal; 1, fraying or longitudinal split of SSC leading edge tendon (type I); 2, less than 50 % SSC tendon detachment to first facet (type IIA); 3, greater than 50 % detachment without complete disruption of lateral hood (type IIB); and 4, tear involving the entire first facet of the lesser tuberosity or more (type III-V). Grading scores between 2 and 4 were regarded as a SSC tendon tear.
Images were presented in random order at each reading session and evaluated using a picture archiving and communication system (Centricity Radiology RA 1000; GE Healthcare, Chicago, IL, USA). A full-thickness tear was diagnosed if there was complete discontinuity in the tendon and if signal abnormality extended from the articular surface of the cuff to the subacromial/subdeltoid bursa, with or without retraction of the musculotendinous junction [20, 21]. A partial-thickness tear was diagnosed when a focal region of fiber discontinuity filled with abnormal signal intensity involving either the articular or the bursal surface (though not through the entire thickness of the tendon) was observed [20, 21]. Ancillary signs such as surface fraying or changes in tendon caliber were also considered [21]. If an intratendinous high signal intensity that did not extend to the articular or bursal surface (potentially indicating an intrasubstance tear) was observed, it was not scored as a tear because intrasubstance partial-thickness tear cannot be accurately correlated with arthroscopy. The imaging criterion of a SSC tendon tear was as follows: discontinuity and/or retraction of the tendon, signal abnormality filling a gap over the lesser tuberosity, atrophy of the subscapularis, or malposition of the tendon of the long head biceps brachii [20, 21]. Signal abnormality of the tendon was defined as high signal intensity on T2W images with a similar intensity to fluid. For indirect MR arthrography, bright signal intensity on T1W images was also classed as a tendon signal abnormality.
Arthroscopic surgery
The arthroscopic findings were utilized as the reference standard. The arthroscopic surgeries were performed by an orthopedic surgeon who had 10 years of experience in shoulder surgery and was not blinded to the MRI findings. The surgeon recorded the presence or absence of SSP-ISP and/or SSC tendon tears. The SSP-ISP tendon tears were categorized as full-thickness or partial-thickness tears and partial-thickness tears were further classified as articular- or bursal-surface tears. All SSP-ISP and SSC tendons were graded using the three- and five-point scales in the same manner by the two readers.
Statistical analysis
Pearson’s chi-squared test and Mann-Whitney’s U test were carried out to detect significant differences in qualitative and categorical data between the two groups. Categorical data included the prevalence of rotator cuff tears, types of SSP-ISP tendon tears and grading of SSC tendons, as well as patient age and sex. In addition, the sensitivity, specificity, and accuracy of the two readers for detecting the presence of SSP-ISP tendon tears, without considering the grades of the tears, was calculated for both groups. The sensitivity, specificity, and accuracy in evaluating full- or partial-thickness tears of the SSP-ISP tendon were calculated using the tear grades—for instance, if an arthroscopically confirmed full-thickness tear had been interpreted as a partial-thickness tear, it was considered as an incorrect diagnosis. Similarly, the side of a partial-thickness tear was also considered in calculating the sensitivity, specificity, and accuracy for articular- and bursal-surface partial-thickness tears. The sensitivity, specificity, and accuracy for detecting SSC tendon tears were calculated without considering the tear grades. Statistically significant differences in the sensitivities, specificities, and accuracies between groups A and B, for both readers, were analyzed using the Fisher’s exact test or Pearson’s chi-squared test. To evaluate diagnostic performances of the two readers together, a generalized estimating equation model was used; adjustment of patient age and sex was performed for multivariate analysis.
To compare the concordance rate (regarding grading of SSP-ISP and SSC tendons) between the MR and arthroscopic findings in the two groups, the concordance rates according to three- and five-point scales for SSP-ISP and SSC tendon tears, respectively, were calculated for the two readers. A Pearson’s chi-squared test was used for the statistical comparison between the two groups.
Inter-observer agreement for the presence of SSP-ISP and SSC tendon tears, and their grading using a non-weighted and weighted κ statistics, respectively, were also evaluated. Agreement was classified as “excellent” for a κ value of 0.81–1.0, “substantial” for a κ value of 0.61–0.80, “moderate” for a κ value of 0.41–0.60, “fair” for a κ value of 0.21–0.40, “slight” for a κ value of 0–0.20, and “poor” for a κ value of less than 0. Statistical analysis was performed using Statistical Analysis Software (version 9.3, SAS Institute, Cary, NC, USA), SPSS Statistics Standard (version 18.0.0, IBM, Chicago, USA), and R 3.0.2 (Vienna, Austria; http://www.R-project.org/). A p value of less than 0.05 was considered significant.
Results
General characteristics of patients in two groups
Patient characteristics are presented in Table 2; in comparison with group B, patients in the group A had a higher prevalence of tears in the SSP-ISP tendon (p = 0.032). The prevalence of full-thickness SSP-ISP tendon tear was also higher in group A (59 %) than in group B (48 %); however, the difference between the groups was not statistically significant (p = 0.053; Fig. 1). There was no significant difference in the prevalence of partial-thickness of SSP-ISP tendon tear, SSC tendon tear, or the age and sex of the patients, between groups A and B.
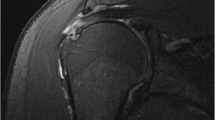
Noncontrast MR images of the left shoulder in a 43-year-old man with arthroscopically proven full-thickness tear of the supraspinatus-infraspinatus tendon. Oblique coronal images with fat-saturated proton density-weighted (a) and T2-weighted (b) sequences show a tendon discontinuity involving the full-thickness of the supraspinatus-infraspinatus tendon (arrows) with medial retraction of the myotendinous junction. Both readers interpreted the images as a full-thickness tear of the supraspinatus-infraspinatus tendon
Diagnostic performance
The overall diagnostic performance for the detection of SSP-ISP and SSC tendon tears are summarized in Table 3. With regard to diagnosis of articular-surface partial-thickness tear of SSP-ISP tendon, sensitivities were generally higher in group B than in group A (80 % vs. 60 % for reader I, and 70 % vs. 40 % in reader II, respectively), but the difference was not statistically significant (p values > 0.05; Fig. 2). However, multivariable analysis using the generalized estimating equation after adjusting patient age and sex, revealed that sensitivity was higher in group B than in group A (p = 0.046). In reader I, the specificity for diagnosing SSC tendon tear was higher in group B than in group A (85 % vs. 68 %; p = 0.012; Figs. 3 and 4). Univariable analysis using the generalized estimating equation demonstrated that the accuracy for diagnosing SSC tendon tear was higher in group B than in group A (p = 0.042). There was no statistical significant difference in any of the other parameters relating to the diagnoses of SSP-ISP and SSC tendon tears.
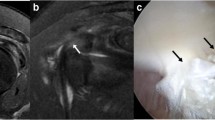
Indirect MR arthrography of the left shoulder in a 45-year-old man with arthroscopically proven articular-surface partial-thickness tear of the supraspinatus-infraspinatus tendon. Oblique coronal images with fat-saturated T1-weighted (a) and T2-weighted (b) sequences demonstrate a small defect with an irregular, indistinct margin at the articular surface of supraspinatus-infraspinatus tendon (arrows). This is more clearly delineated on fat-saturated T1-weighted sequence with contrast material filling the tendon defect (a). Associated linear low signal intensity and bone marrow edema are evident (arrowheads). Both readers correctly interpreted the images as an articular-surface partial-thickness tear of the supraspinatus-infraspinatus tendon
Noncontrast MR images of the right shoulder in a 63-year-old man with arthroscopically proven intact subscapularis tendon. Axial fat-saturated proton-density (a) and oblique sagittal T2-weighted (b) images show a small high signal intensity area at the articular surface of the subscapularis tendon cranial portion (arrows). Both readers false positively scored this lesion as a grade 2 tear of the subscapularis tendon. A full-thickness tear of the supraspinatus-infraspinatus tendon is also seen (arrowhead)
Indirect MR arthrography of the right shoulder in a 63-year-old woman with arthroscopically proven grade 2 tear of the subscapularis tendon. Fat-saturated T1-weighted images in the axial (a) and oblique sagittal (b) planes show focal irregularity with contrast accumulation in an articular fiber of the subscapularis tendon cranial portion (arrows). Both readers correctly interpreted the images as a grade 2 tear of the subscapularis tendon. Subacromial-subdeltoid bursitis is associated (arrowheads)
Concordance rate of SSC tendon tears by reader I was higher in group B compared with group A (57 % vs. 40 %, p = 0.005). Concordance rate of SSC tendon tears by reader II was also higher in group B than in group A, but this difference was statistically not significant (47 % vs. 40 %, p = 0.228). There was no other statistically significant differences in concordance rates between the two groups (Table 4).
Interobserver agreement
Regarding the interobserver agreement for the presence of SSP-ISP tendon tears, the agreement for group A was substantial (0.78; 95 % CI, 0.603–0.966), while that for group B was excellent (0.87; 95 % CI, 0.799–0.946); however, there was no statistically significant difference between the two groups (p = 0.381). Weighted κ values for evaluating the grade of SSP-ISP tendons showed excellent agreement between the two readers in group A (0.83; 95 % CI, 0.743–0.921) and in group B (0.85; 95 % CI, 0.794–0.898), similarly there were also no statistically significant differences between the two groups (p = 0.796).
Interobserver agreements relating to the presence of SSC tendon tears were substantial in group A (0.69; 95 % CI, 0.544–0.831) and group B (0.73; 95 % CI, 0.643–0.817). Agreements relating to the grade of SSC tendons were also substantial in groups A (0.66; 95 % CI, 0.556–0.758) and B (0.63; 95 % CI, 0.562–0.689). There were no significant differences between the two groups for the tear presence (p = 0.619) and grade (p = 0.599) in SSC tendons.
Discussion
Indirect MR arthrography, as described by Vahlensieck et al. [3, 8], is a technique which utilizes intravenous injection of paramagnetic contrast material to achieve arthrogram-like images similar to those obtained in direct MR arthrography. Several investigators have described indirect MR arthrography as a highly accurate and sensitive technique for detecting labral pathology [6, 9, 22, 23]. A comparison study between noncontrast MRI and indirect MR arthrography by Dinauer et al. [6] revealed a higher sensitivity of indirect MR arthrography for the diagnosis of superior glenoid labral lesions. However, to our best knowledge, there have been relatively few studies comparing the rotator cuff tear diagnostic abilities of noncontrast MRI and indirect MR arthrography. While Yagci et al. [4] analyzed the efficacy of indirect MR arthrography and noncontrast MRI for suspected rotator cuff abnormalities, the study was based on a small number of patients, without statistical comparison between the two techniques (except for the interobserver agreement). Previous studies have revealed that indirect MR arthrography is highly accurate in diagnosing overall and full-thickness tears of SSP-ISP tendons [4, 9, 12–14, 24]. In contrast, the correct diagnoses of a partial-thickness tear remains difficult despite the use of intravenous contrast media [12, 14, 24].
In the present study, the correct detection rate of indirect MR arthrography did not statistically differ from that of noncontrast MRI in terms of sensitivity. Although bright signal intensity of the joint fluid due to the paramagnetic contrast material was expected to improve the visualization of small tendon defects, no diagnostic gain was identified (compared with the usual T2-hyperintense fluid on noncontrast MRI). One possible explanation is that the contrast between the torn tendon and joint fluid filling the tendon defect was sufficient to enable the detection of SSP-ISP and SSC tendon tears without the aid of intravenous contrast material injection. The high diagnostic performance in both readers for the noncontrast MRI group, particularly for diagnosing full-thickness tears of SSP-ISP tendons, may support this explanation. Similarly, there was no statistically significant difference between the two groups observed in cases of partial-thickness tears. While it appears that the sensitivities for the detection of articular-surface partial-thickness tears using indirect MR arthrography were higher than those using noncontrast MRI for both readers, the difference was not statistically significant except for multivariate analysis. These results are in contrast to the findings of Yagci et al. [4] and Vahlensieck et al. [25], which suggested that paramagnetic contrast material in the bursal and articular surface of the rotator cuff tendon leaks into partial tears, enabling the visualization of the tear directly and consequently facilitating a more accurate diagnosis. In the present study, there were only five cases of articular-surface partial-thickness tears in the noncontrast MRI group; therefore, the power of statistical analysis may have been limited, impeding the detection of true differences between the two groups.
There are several drawbacks of indirect MR arthrography such as the enhancement of extra-articular, synovial, vascularized structures, lack of joint capsule distension, and the risk of side effects due to intravenously administered contrast medium [3, 5, 8]. Among these, enhancement of extra-articular structures has been suggested to be responsible for false-positive interpretations [4], although it can be helpful in detecting inflamed tissue such as adhesive capsulitis [26]. In the present study, however, the specificities for diagnosing rotator cuff tendon tears were not significantly different between both groups. Since the two readers were well experienced with the indirect MR arthrography technique, this potential drawback was considered to be overcome through the recognition of different signal intensities, morphology, and the location of the enhancing area between normal anatomy and rotator cuff pathology, in accordance with Vahlensieck et al. [3].
In one of the readers, indirect MR arthrography enabled a more specific diagnosis of SSC tendon tears and a more accurate prediction of tear grades with statistical significance when compared with noncontrast MRI. In addition, univariate analysis using the generalized estimating equation suggested that indirect MR arthrography was also superior in terms of diagnostic accuracy. Both fat-saturated T1W and T2W sequences are obtained in the oblique sagittal plane for indirect MR arthrography, while only the T2W sequence was included as the oblique sagittal plane in noncontrast MRI. Therefore, it could be inferred that the addition of fat-saturated T1W oblique sagittal sequence after intravenous paramagnetic contrast material injection improved diagnostic performance, suggesting the importance of the oblique sagittal plane for the diagnosis of SSC tendon tear. This has also been discussed by Pfirrmann et al. [27], who reported higher specificity and grading accuracy for SSC tendon abnormalities with parasagittal images compared with transverse images. We hypothesized that the contrast between the SSC tendon and surrounding structures is increased on indirect MR arthrography, consequently reducing false-positive interpretations and aiding correct tear grading. In particular, the enhancement of rotator interval, with chronic inflammation and fibrosis, may help distinguish these structures from the cranial part of the SSC tendon, which is often difficult with noncontrast T2W sequences (Fig. 5). Therefore, these results suggest that indirect MR arthrography could be advantageous for more accurate diagnosis of SSC tendon tears and for the prediction of tear grading. Since substantial SSC tendon tears have been underestimated, and their inadequate repair may result in decreased glenohumeral joint stability, accurate preoperative detection of SSC tears is important and the use of indirect MR arthrography could be helpful in this [28–30]. However, in contrast, the sensitivities between the two methods did not statistically differ in this study. Similar to the SSP-ISP tendon, this may be explained by the fact that the paramagnetic contrast material, which diffused into the intra-articular cavity, has no definite added diagnostic gain compared to the T2-hyperintense fluid on noncontrast MRI.
Indirect MR arthrography of the left shoulder in a 63-year-old woman with arthroscopically proven fraying of the subscapularis tendon. Oblique sagittal images with fat-saturated T1-weighted (a) and T2-weighted (b) sequences reveal subtle indistinct margin at the cranial portion of the subscapularis tendon (arrows). Abnormally thickened soft tissue, causing fat obliteration in the rotator interval is visible, suggesting adhesive capsulitis (arrowheads). The border between the cranial portion of subscapularis tendon and inflamed rotator interval is more clearly demarcated with better soft tissue contrast on fat-saturated T1-weighted image (a) when compared with T2-weighted image (b). Both readers correctly scored the subscapularis tendon as grade 1 (fraying). Subacromial-subdeltoid bursitis is visible (black arrows)
There were several limitations of our study. Firstly, the MR images were analyzed retrospectively in this non-randomized study, and the surgeon was not blinded to the MRI findings. Secondly, direct comparison between the two techniques in the same patient was not possible because noncontrast MRI and indirect MR arthrography were performed on different patient populations. Also, the number and type of sequences were different besides the addition of postcontrast fat-saturated T1WI sequences. In particular, the lack of axial T2WI for noncontrast MRI may underscore the accuracy of this technique, especially for subscapularis tendon evaluation. Thirdly, the overall prevalence of SSP-ISP tendon tears was significantly higher in the noncontrast MRI group than in the indirect MR arthrography group, which may overestimate the diagnostic performance of noncontrast MRI. In addition, the mean interval between MR examination and arthroscopic surgery was shorter in the indirect MR arthrography group although only patients who underwent surgery within the 30-day period after MR examination were included in this study. Fourthly, as this study was conducted entirely with patients who underwent arthroscopic surgery, the possibility of selection bias, which may result in overestimation of sensitivities and underestimation of specificities, cannot be excluded. Fifthly, intratendinous tears were not evaluated. Although they cannot be scored on arthroscopy, it is an important drawback of assessing the potential added value of indirect arthrography as intratendinous tears are clinically relevant. One final limitation is that there were relatively few patients with articular-surface partial-thickness tear of SSP-ISP tendon, particularly in the noncontrast MRI group (only five patients).
In conclusion, indirect MR arthrography was not superior to noncontrast MRI for the diagnosis of SSP-ISP tendon tears, except for a tendency for a slightly higher sensitivity for diagnosing articular-surface partial-thickness tears. However, improved accuracy may be expected for preoperative diagnosis and for the grading SSC tendon tears using indirect MR arthrography.
References
Winalski CS, Aliabadi P, Wright RJ, Shortkroff S, Sledge CB, Weissman BN. Enhancement of joint fluid with intravenously administered gadopentetate dimeglumine: technique, rationale, and implications. Radiology. 1993;187(1):179–85.
Drape JL, Thelen P, Gay-Depassier P, Silbermann O, Benacerraf R. Intraarticular diffusion of Gd-DOTA after intravenous injection in the knee: MR imaging evaluation. Radiology. 1993;188(1):227–34.
Vahlensieck M, Sommer T, Textor J, et al. Indirect MR arthrography: techniques and applications. Eur Radiol. 1998;8(2):232–5.
Yagci B, Manisali M, Yilmaz E, et al. Indirect MR arthrography of the shoulder in detection of rotator cuff ruptures. Eur Radiol. 2001;11(2):258–62.
Bergin D, Schweitzer ME. Indirect magnetic resonance arthrography. Skelet Radiol. 2003;32(10):551–8.
Dinauer PA, Flemming DJ, Murphy KP, Doukas WC. Diagnosis of superior labral lesions: comparison of noncontrast MRI with indirect MR arthrography in unexercised shoulders. Skelet Radiol. 2007;36(3):195–202.
Lee MJ, Motamedi K, Chow K, Seeger LL. Gradient-recalled echo sequences in direct shoulder MR arthrography for evaluating the labrum. Skelet Radiol. 2008;37(1):19–25.
Vahlensieck M, Peterfy CG, Wischer T, et al. Indirect MR arthrography: optimization and clinical applications. Radiology. 1996;200(1):249–54.
Jung JY, Yoon YC, Yi SK, Yoo J, Choe BK. Comparison study of indirect MR arthrography and direct MR arthrography of the shoulder. Skelet Radiol. 2009;38(7):659–67.
Sommer T, Vahlensieck M, Wallny T, et al. Indirect MR arthrography in the diagnosis of lesions of the labrum glenoidale. Röfo. 1997;167(1):46–51.
Wagner SC, Schweitzer ME, Morrison WB, Fenlin Jr JM, Bartolozzi AR. Shoulder instability: accuracy of MR imaging performed after surgery in depicting recurrent injury—initial findings. Radiology. 2002;222(1):196–203.
Van Dyck P, Gielen JL, Veryser J, et al. Tears of the supraspinatus tendon: assessment with indirect magnetic resonance arthrography in 67 patients with arthroscopic correlation. Acta Radiol. 2009;50(9):1057–63.
Lee JH, Yoon YC, Jee S. Diagnostic performance of indirect MR arthrography for the diagnosis of rotator cuff tears at 3.0 T. Acta Radiol. 2015;56(6):720–6.
Herold T, Bachthaler M, Hamer OW, et al. Indirect MR arthrography of the shoulder: use of abduction and external rotation to detect full- and partial-thickness tears of the supraspinatus tendon. Radiology. 2006;240(1):152–60.
Allmann K-H, SCHÄFER O, Hauer M, et al. Indirect MR arthrography of the unexercised glenohumeral joint in patients with rotator cuff tears. Investig Radiol. 1999;34(6):435.
Clark J, Harryman D. Tendons, ligaments, and capsule of the rotator cuff. J Bone Joint Surg Am. 1992;74(5):713–25.
Minagawa H, Itoi E, Konno N, et al. Humeral attachment of the supraspinatus and infraspinatus tendons: an anatomic study. Arthrosc: J Arthrosc Relat Surg. 1998;14(3):302–6.
Mochizuki T, Sugaya H, Uomizu M, et al. Humeral insertion of the supraspinatus and infraspinatus: new anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008;90(5):962–9.
Yoo JC, Rhee YG, Shin SJ, et al. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. 2015;31(1):19–28.
Opsha O, Malik A, Baltazar R, et al. MRI of the rotator cuff and internal derangement. Eur J Radiol. 2008;68(1):36–56.
Kassarjian A, Bencardino JT, Palmer WE. MR imaging of the rotator cuff. Radiol Clin N Am. 2006;44(4):503–23. vii-viii.
Razzano A, Morscher M, Jones K, Eghbal A. Indirect shoulder MR arthrography: a novel technique for identifying labral pathology in young patients. Orlando, FL: American Academy of Pediatrics National Conference and Exhibition; 2013. p. 26–9.
Fallahi F, Green N, Gadde S, Jeavons L, Armstrong P, Jonker L. Indirect magnetic resonance arthrography of the shoulder: a reliable diagnostic tool for investigation of suspected labral pathology. Skelet Radiol. 2013;42(9):1225–33.
Oh DK, Yoon YC, Kwon JW, et al. Comparison of indirect isotropic MR arthrography and conventional MR arthrography of labral lesions and rotator cuff tears: a prospective study. AJR Am J Roentgenol. 2009;192(2):473–9.
Vahlensieck M, Sommer T. Indirect MR arthrography of the shoulder. An alternative to direct MR arthrography? Radiologe. 1996;36(12):960–5.
Song KD, Kwon JW, Yoon YC, Choi SH. Indirect MR arthrographic findings of adhesive capsulitis. AJR Am J Roentgenol. 2011;197(6):W1105–9.
Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology. 1999;213(3):709–14.
Lo IK, Burkhart SS. The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy. 2003;19(10):1142–50.
Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–93.
Morag Y, Jamadar DA, Miller B, Dong Q, Jacobson JA. The subscapularis: anatomy, injury, and imaging. Skelet Radiol. 2011;40(3):255–69.
Acknowledgements
The authors thank to Keumhee Cho and Min-Ji Kim, the staff of Biostatistics and Clinical epidemiology Center, for their contribution to the analysis and design for the statics.
Conflict of interest
The authors declare that they have no conflict of interest.
IRB statement
Approved
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.H., Yoon, Y.C., Jung, J.Y. et al. Rotator cuff tears noncontrast MRI compared to MR arthrography. Skeletal Radiol 44, 1745–1754 (2015). https://doi.org/10.1007/s00256-015-2228-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2228-z