Abstract
Talo-calcaneal coalitions may be intra-articular or extra-articular in position and may be classified as fibrous, cartilaginous or osseous in morphology. Fibrous coalitions, particularly extra-articular talo-calcaneal coalitions, may have cross-sectional imaging findings that resemble normal anatomic variants, particularly the medial talo-calcaneal ligament and to a lesser extent the presence of an accessory articular facet between the posterior margin of the sustentaculum and postero-medial process of the talus. Typically, in the adult fibrous coalition, there will be some osseous deformity at the entheses, allowing differentiation from a medial talo-calcaneal ligament. The anatomy of the subtalar joint and its ligamentous supports, normal anatomic variations and their corresponding imaging appearance are reviewed in the first part of this article. In the second part, the various forms of talo-calcaneal coalition and their imaging appearance are reviewed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The subtalar region is a common site of anatomic variation, particularly with respect to ligamentous structures and, to a lesser extent, osseous morphology. Awareness of the normal range of anatomic variation is critical in being able to differentiate between normal anatomic variation and the presence of a talo-calcaneal coalition, particularly fibrous coalitions. In the senior author’s experience, misinterpretation of anatomic variations and failure to observe subtle tarsal coalitions can adversely affect patient management. The scope of this article is firstly to discuss the variations in normal talo-calcaneal anatomy and secondly to describe the typical patterns of talo-calcaneal coalition, using examples drawn from the senior author’s routine clinical experience over the last 10 years, during which time approximately 100 tarsal coalitions or variations in talo-calcaneal ligamentous anatomy have been observed.
Part 1: Anatomy and anatomic variations
Posterior subtalar joint
The posterior subtalar joint is the articulation between the postero-inferior aspect of the talar body and the postero-superior aspect of the calcaneus. It is a complex planar joint, oriented approximately in the horizontal plane and lying immediately posterior to the sinus tarsi.
The posterior subtalar joint has both intra-capsular and extra-capsular ligamentous supports. The intra-capsular ligamentous supports include the posterior talo-calcaneal ligament, lateral talo-calcaneal ligament and anterior capsular ligament of the posterior subtalar joint. The extra-articular ligamentous supports include the calcaneo-fibular ligament, superficial deltoid ligament and the interosseous talo-calcaneal and cervical ligaments. The variably present medial talo-calcaneal ligament is extra-articular and provides ligamentous support to the posterior subtalar joint [1]. The inferior extensor retinaculum also imparts stability to the posterior subtalar joint.
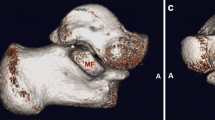
There are a number of variations in subtalar joint articular facet anatomy, including medial extension of the articular surfaces to involve the posterior margin of the sustentaculum and the antero-inferior margin of the postero-medial process of the talus [2]. Anteriorly, there may be extension of the articular facets to involve the base of the anterior process of the calcaneus and the anterior margin of the lateral process of talus and talar body [1] (Fig. 1).
Variations in posterior subtalar joint ligamentous anatomy
-
(a)
Medial talo-calcaneal ligament
The variably present medial talo-calcaneal ligament is perhaps of greatest importance with respect to potential confusion between normal anatomy and a fibrous extra-articular talo-calcaneal coalition. The medial talo-calcaneal ligament courses from the antero-inferior margin of the postero-medial process of talus to insert on the posterior margin of the sustentaculum tali [1, 3] (Fig. 2).
The medial talo-calcaneal ligament is in the senior author’s experience visualised on magnetic resonance imaging (MRI) in approximately 2% of cases and is best seen on sagittal and coronal proton density (PD) images due to the high contrast resolution between the ligament, adjacent adipose tissue, cortical bone and articular cartilage. The ligament may be a narrow bundle [4] or multi-fascicular in morphology. The cortical attachments of the ligament are smooth (Fig. 3). A variation in the medial talo-calcaneal ligament includes an insertion on the talus just anterior to the postero-medial process of the talus (Fig. 4).
The medial talo-calcaneal ligament may be confused with an extra-articular fibrous coalition (Fig. 5). One differentiating feature in the adult is the absence of associated bony deformity at the insertions of the medial talo-calcaneal ligament. Osseous deformity is typically present at the attachments of a fibrous coalition in an adult, speculated to be due to the abnormal forces transmitted through the coalition [5].
-
(b)
Anterior capsular ligament of the posterior subtalar joint
Dissection of the anterior capsular ligament of the posterior subtalar joint (white arrows) seen laterally (a) and diagrammatic representation from a posterior perspective with the talus removed (b). The anterior capsular ligament of the posterior subtalar joint (black arrow) lies lateral and posterior to the interosseous talo-calcaneal ligament
The anterior capsular ligament of the posterior subtalar joint is a thickening of the anterior capsule, relatively vertical in orientation, situated lateral and just posterior to the course of the interosseous talo-calcaneal ligament (ITCL; Fig. 6). On MRI, the anterior capsular ligament is best visualised on sagittal and coronal PD sequencing. The ligament is of variable thickness, ranging from being barely perceptible to 2–3 mm in thickness (Fig. 7). Thickening of the anterior capsule of the posterior subtalar joint may be seen medial to the normal site of the anterior capsular ligament, also reflecting anatomic variation (Fig. 8).
-
(c)
Interosseous talo-calcaneal ligament
Sagittal proton density MRI demonstrating a thickened anterior capsule of the posterior subtalar joint at the anterior margin of the interval between the sustentaculum and postero-medial process talus (black arrow) can mimic an extra-articular fibrous talo-calcaneal coalition. Note, however, the absence of bony deformity and secondary changes of a fibrous coalition
a Diagrammatic representation of the tarsal canal and apex of the sinus tarsi, after removing the posterior half of the talus, demonstrating the interosseous talo-calcaneal ligament (black arrow). b Diagram demonstrating the calcaneal attachment of the ITCL between the middle and posterior calcaneal facets
The ITCL is also known as the ligament of the tarsal canal, reflecting its position at the apex of the sinus tarsi. It lies medial and just distal to the anterior capsular ligament of the posterior subtalar joint and is oblique in orientation, coursing from the talar neck to the dorsum of the calcaneus. It inserts antero-medial to the posterior calcaneal facet and postero-lateral to the middle calcaneal facet [3] (Fig. 9).
Jotoku et al. [6] reviewed the morphology of the interosseous talo-calcaneal ligament in 40 cadaveric specimens. A flat and thick band type was present in 37 of 40 cadavers. A fan-type ligament with broad talar origin and tapered calcaneal insertion was present in two of 40 cadavers and a multi-fascicular- or multi-ligament-type morphology was present in one specimen (Fig. 10).
a Sagittal and b coronal proton density MRIs demonstrating a thick posterior capsule of the middle subtalar joint (black arrow) that can mimic an extra-articular fibrous talo-calcaneal coalition or a normal interosseous talo-calcaneal ligament. Note the absence of bony deformity at the insertions. A separate hypoplastic ITCL (black arrowhead) is demonstrated more laterally
The interosseous talo-calcaneal ligament should not be confused with an extra-articular fibrous coalition on sagittal MRI sequencing. The oblique orientation of the ligament fibres from supero-medial to infero-lateral is a distinguishing feature from a coalition which tends to course in a straight sagittal plane.
Middle subtalar joint
The middle subtalar joint is formed by the sustentacular articular facet of the calcaneus and the middle talar articular facet of the talus, the latter part situated at the plantar, proximal margin of the talar head. The joint is in communication with the talo-navicular joint and has thus been termed the talo-navicular middle subtalar joint complex. Middle talar articular facet anatomy is relatively constant. Occasionally, the middle and anterior calcaneal and talar articular facets may be contiguous.
The posterior capsule of the middle subtalar joint may be of variable thickness, occasionally being relatively thick, potentially mimicking a fibrous coalition or the interosseous talo-calcaneal ligament. The ITCL may be hypoplastic in the setting of a thick posterior capsule of the middle subtalar joint (Fig. 11).
Anterior subtalar joint
The anterior subtalar joint is variably present and is the smallest of the three subtalar joints. It is situated anterior and lateral to the middle subtalar joint and is formed by the plantar, lateral margin of the talar head and an articular facet at the supero-medial border of the anterior process of the calcaneus.
Part 2: Talo-calcaneal tarsal coalition
Tarsal coalition is a congenital bridging of two or more tarsal bones of the foot [7]. It commonly presents in childhood and adolescence and is the most common cause of peroneal spastic flatfoot [8]. The coalition may be fibrous (syndesmosis), cartilaginous (synchondrosis) or osseous (synostosis) [9, 10]. Osseous coalitions in the adult are usually obvious on cross-sectional imaging. As a guiding principle, cartilaginous or fibrous coalitions presenting in adulthood will have some osseous deformity at the coalition margins [5, 11]. This is helpful when attempting to distinguish between a coalition and the anatomical variants described above, particularly the medial talo-calcaneal ligament.
The incidence of tarsal coalition is traditionally quoted at approximately 1% [12, 13]. However, this figure is likely to be an underestimation as it disregards asymptomatic coalitions. Cadaver dissection studies have reported an incidence of 6% to 9% [14, 15] and studies of first-degree relatives of patients with symptomatic tarsal coalition have reported an asymptomatic coalition in 39% [16]. Tarsal coalitions, particularly incomplete and extra-articular types, are increasingly being recognised in asymptomatic or minimally symptomatic adult patients [15, 17].
Tarsal coalitions are thought to arise due to a failure of mesenchymal differentiation and segmentation with resultant lack of joint formation [7, 18, 19]. During normal foetal ankle development, mesenchyme forms a cartilaginous bridge between the talus and calcaneus postero-medially, at approximately the 8-week stage. During normal development, resorption of the cartilaginous bridge results in a non-cartilaginous and non-fibrous interval between the posterior border of the sustentaculum and the postero-medial process of the talus at eight and a half weeks [20].
Kawashima and Uhthoff [20] described variation in morphology of the postero-medial talo-calcaneal interval in a study of foetal cadaveric ankles. There may be a persistent extra-articular cartilaginous talo-calcaneal bridge in this area at 9 weeks or sometimes a persistent cartilaginous bridge with extra-articular and intra-articular components, the latter component at the level of the middle subtalar joint. Kawashima and Uhthoff typically saw these changes in the 9- to 12-week foetus. Additionally, they observed in two of 43 foetuses a fibrocartilaginous extra-articular talo-calcaneal bridge between the posterior margin of the sustentaculum and the postero-medial process of the talus, in the 13–21-week foetus. Whether these were destined to become extra-articular coalitions or there would have been subsequent ligamentous differentiation to form a medial talo-calcaneal ligament is open to speculation.
It has been theorised that the pathogenesis of tarsal coalition may involve abnormality at the neural crest level. The evidence to support this theory is derived from studies of individuals with multiple tarsal coalitions such as those seen in the type 0 fibular hemimelia spectrum in which there is a normal fibula, absent fifth ray and multiple coalitions in an S2 sclerotomal distribution [21].
Classification of talo-calcaneal coalition
Talo-calcaneal coalitions are common. They account for approximately 48% of cases of coalition [13]. Their location and morphology are variable [22]. They are classified as intra-articular or extra-articular [23] and according to their morphology as fibrous, cartilaginous or osseous coalitions [9, 10].
Intra-articular talo-calcaneal coalitions most commonly involve the middle subtalar joint [15, 24] and usually involve the entire joint. Intra-articular posterior subtalar joint coalitions are unusual [25] and, typically, involve only the postero-medial margin of the joint. Anterior subtalar joint coalitions are extremely uncommon as isolated findings [15]. When present, they usually also involve the middle subtalar joint. Extra-articular talo-calcaneal coalitions usually involve the interval between the posterior margin of the sustentaculum and the postero-medial process of the talus.
Osseous talo-calcaneal coalitions typically ossify when patients are approximately 12 to 16 years old [26]. Patients will often present in adolescence when subtalar motion becomes restricted and the foot becomes symptomatic, often following minor trauma or activity [27, 28].
Role of imaging in tarsal coalition and imaging technique
The role imaging in tarsal coalition is to identify and characterise the coalition, including its extent and nature (osseous, cartilaginous or fibrous), and to identify, when present, complicating ganglion formation. It is also important to identify the occasionally present second site of tarsal coalition that should be taken into account when contemplating surgical intervention.
Specific plain radiographic views that provide assessment for talo-calcaneal tarsal coalition may include Harris–Beath views. This view is performed with the patient prone and ankle dorsi-flexed and slightly internally rotated. It will demonstrate the middle and posterior subtalar joint spaces.
Computerised tomographic (CT) assessment for tarsal coalition should be performed with a helical acquisition, with 2–3-mm reconstructions in the sagittal, coronal and axial plane. The coronal reconstructions are best plotted off a sagittal image, perpendicular to the longitudinal axis of the middle subtalar joint. CT will demonstrate osseous anatomy in exquisite detail and has reasonable accuracy in the detection of tarsal coalition. However, CT does not have sufficient contrast resolution to demonstrate the fibrous component of a tarsal coalition and relies on the demonstration of osseous deformity at the attachments of the fibrous coalition to allow diagnosis. In addition, CT will not demonstrate bone marrow oedema at the margins of a coalition that may be seen on MRI. In the senior author’s practice, CT is reserved for clarifying osseous detail that is not clearly characterised on an MRI.
MRI assessment for tarsal coalition will usually entail a standard ankle MRI protocol, unless otherwise directed by the clinical history. The senior author’s standard ankle magnetic resonance (MR) protocol is performed on a quadrature coil with a chimney construct. The examination consists of: (1) sagittal fat-suppressed proton density; (2) high-resolution sagittal proton density; (3) high-resolution coronal proton density; (4) reverse angle coronal PD sequencing through the talar dome, (5) axial proton density and (6) fat-suppressed T2 sequencing (Table 1).
Middle facet talo-calcaneal coalition
An osseous middle facet talo-calcaneal coalition is present in the adult when there is continuous fatty marrow bridging the talus and calcaneus at the middle facet level with no intervening joint space present [7]. Typically, there is associated broadening of the transverse dimensions of the middle subtalar interval.
The diagnosis maybe evident on plain radiography by virtue of the absence of visualisation of the middle subtalar joint (Fig. 12) [29]. Secondary radiographic signs have been described, including the talar beak, the “C-sign” and the ball and socket ankle joint [30–34]. Talar beaking is related to chronic traction stress at the talar head insertion of the dorsal talo-navicular joint capsule, with resultant superiorly directed bony spur that is readily visualised on a lateral radiograph of the ankle [31]. This finding may also been seen in the setting of a calcaneo-navicular coalition and does not indicate the presence of osteoarthritis [35, 36]. A talar beak has no prognostic significance with respect to surgical excision of a coalition or predicting secondary degenerative changes. The C-sign consists of visualisation of a continuous C-shaped cortical line on a lateral radiograph of the ankle, formed by the medial outline of the talar dome and the inferior outline of the sustentaculum tali. The C-sign is of limited sensitivity and may be present in the setting of a valgus hindfoot alone [32]. The ball and socket ankle joint consists of an abnormally rounded contour talar dome on an antero-posterior ankle radiograph, with corresponding somewhat rounded contour of the malleolar articular facets. It relates to modelling deformity at the talo-crural joint due to rigidity of the hindfoot as a result of a tarsal coalition. Osseous talo-calcaneal coalitions are readily diagnosed on CT or MRI (Fig. 13).
Cartilaginous middle facet talo-calcaneal coalition (white arrow) seen on sagittal proton density (a), fat-saturated sagittal proton density (b) and coronal proton density (c) MRIs. Note abnormal morphology of the middle facets, abnormal subchondral plate and cartilage, cystic change and bone marrow oedema at the coalition margins. The morphology of the sustentacular facet on coronal cross section has been described as the “drunken waiter sign” (black arrow)
In a cartilaginous middle facet talo-calcaneal coalition, there is some differentiation of mesenchyme towards an articulation, without formation of hyaline articular cartilage and subchondral plate. The typical imaging findings consist of abnormally oriented, broadened facets, deficient subchondral plate and abnormal-appearing variable-thickness cartilage [37]. The deformity is readily appreciated on coronal MR or CT images (Figs. 14 and 15). The broadened medially down-sloping sustentacular facet [34] has been described as being reminiscent of a “drunken waiter” [38] (Fig. 14). Cystic change is commonly seen at the margins of a cartilaginous talo-calcaneal coalition in the adult (Figs. 14 and 15) due to chronic repetitive abnormal stresses across the synchondrosis [11].
Fibrous middle facet talo-calcaneal coalitions are less common than cartilaginous coalitions. There is a variably widened interval between the rudimentary middle talar and calcaneal facets, with bridging fibrous tissue seen as low-signal intensity on all MRI pulse sequences (Fig. 16). The middle facets typically demonstrate abnormal morphology, particularly in coronal cross section (Fig. 17). Cystic change and bone marrow oedema may be present at the coalition margins.
Sagittal proton density (a, b), coronal proton density (c), axial proton density (d) and fat-saturated axial proton density (e) MRIs demonstrating incomplete cartilaginous posterior facet talo-calcaneal coalition which involves the postero-medial aspect of the posterior subtalar joint (white arrow). Note abnormal cartilage compared with normal hyaline articular cartilage anteriorly. Bony overgrowth postero-medially results in protrusion into the tarsal tunnel (thin white arrow), with mild resultant displacement of the medial plantar nerve. Postero-superiorly directed bony spur arising from the posterior calcaneal facet results in humpback-type deformity (black arrow)
Posterior facet talo-calcaneal coalition
Posterior facet talo-calcaneal coalitions are uncommon [39, 40]. They are typically cartilaginous in nature and involve the postero-medial aspect of the posterior subtalar joint, usually with associated bony overgrowth in the transverse plane and resultant osseous protrusion into the tarsal tunnel. In addition, there is frequently superior overgrowth of the posterior margin of the posterior calcaneal facet (Fig. 18), with resultant humpback-type deformity [39]. Occasionally, these deformities may be misinterpreted as being purely degenerative in aetiology.
Anterior facet talo-calcaneal coalition
Anterior facet talo-calcaneal coalitions are rare [15] and are usually associated with a middle facet coalition (Fig. 19).
Fibrous extra-articular talo-calcaneal coalition (white arrows) on sagittal proton density (a) and (b) and coronal proton density (c) MR images. Note osseous deformity at coalition margins (white arrowheads) and hypoplastic middle subtalar joint (black arrow). Interosseous talo-calcaneal ligament (black arrowhead) is evident as a separate structure anterior to the coalition
Extra-articular talo-calcaneal coalition
Extra-articular talo-calcaneal coalitions occur posterior to the sustentaculum, with an associated variable bony deformity and a normal or relatively normal middle subtalar joint [12]. In the case of an extensive extra-articular talo-calcaneal coalition, the middle subtalar joint may be hypoplastic (Fig. 20).
Cartilaginous extra-articular talo-calcaneal coalition. Lateral plain radiograph (a) demonstrates prominence of the postero-medial process of the talus and narrow interval between the postero-medial process and the posterior margin of the sustentaculum (black arrowheads). Sagittal PD (b), fat-suppressed proton density (c) and coronal proton density (d) MRIs demonstrate abnormal cartilaginous tissue at the interval, mildly irregular osseous margins (white arrows) and mild adjacent bone marrow oedema and cystic change (thin black arrow). Axial proton density (e) MRI demonstrates the prominent postero-medial process protruding into the tarsal tunnel, displacing the medial plantar nerve which demonstrates mild neural oedema (black arrow)
In cartilaginous extra-articular talo-calcaneal coalitions, cartilaginous tissue is variably evident at the synchondrosis, with broadening of the osseous interval at the margins of the synchondrosis in the transverse plane and usually in the sagittal plane, with somewhat irregular osseous margins. There is often associated osseous protrusion into the tarsal tunnel, predisposing to medial plantar nerve irritation (Fig. 21). Ganglions may arise from the coalition and decompress into the tarsal tunnel (Fig. 22) causing tarsal tunnel syndrome [41]. In this setting, the senior author has seen several cases in which the underlying coalition has not been identified on MRI, precluding definitive excision of the ganglion and coalition.
Sagittal fat-suppressed proton density (a) MRI demonstrating fibrous extra-articular talo-calcaneal coalition (white arrow), with adjacent intra-osseous cystic change and bone marrow and soft tissue ganglion cyst (white arrowheads) protruding into the tarsal tunnel. Axial PD image (b) demonstrating the extent of the ganglion cyst and displacement of the medial and lateral plantar nerves (black arrows)
In fibrous extra-articular talo-calcaneal coalition, the osseous deformity is often more subtle. No cartilaginous tissue is evident at the syndesmosis. There may be associated hypoplasia of the interosseous talo-calcaneal ligament (Fig. 23).
Fibrous extra-articular talo-calcaneal coalition (white arrows) on sagittal proton density (a) and coronal proton density (b) images, situated slightly anterior to the coalition seen in Fig. 20. Note osseous deformity (thin white arrow) at coalition margins (a) and (b) and hypoplastic interosseous bifascicular talo-calcaneal ligament on coronal proton density MR image (c) (black arrows)
Occasionally, a patient with a peroneal spastic flat foot may have a tarsal coalition as the underlying cause of the peroneal spasm (Fig. 24). Typically, this occurs in the adolescent or young adult patient [42, 43]. Other causes of peroneal spastic flat foot are more common. In the senior author’s experience, the majority of patients with peroneal spastic flat foot do not have a coalition when evaluated on MRI.
Sagittal fat-suppressed proton density (a) MRI demonstrating fibrous extra-articular talo-calcaneal coalition (white arrows). Note the narrowed sinus tarsi (thin white arrow) and bone marrow oedema in the anterior talar body, lateral process of the talus and at the base of the anterior process of the calcaneus, consistent with abutment associated with peroneal spasm. Sagittal proton density (b) and coronal proton density (c) MRIs demonstrating a fibrous extra-articular talo-calcaneal coalition (white arrows), with subtle bony deformity at the coalition margins. Note interosseous talo-calcaneal ligament (black arrow) medial to the coalition
Conclusion
As illustrated, there is variation in talo-calcaneal anatomy and in the site, extent and morphology of talo-calcaneal coalitions. A detailed knowledge of variations in talo-calcaneal anatomy and in the variable morphology of talo-calcaneal coalitions will aid the radiologist in accurately identifying and interpreting pathology and anatomic variation in the subtalar region. Whilst osseous and extensive cartilaginous coalitions are usually obvious on cross-sectional imaging, fibrous coalitions, particularly extra-articular talo-calcaneal coalitions, may have less conspicuous cross-sectional imaging findings that may resemble normal anatomic variants, particularly the medial talo-calcaneal ligament. As a guiding principle, it is reasonable to expect that in the adult fibrous coalition there will be some osseous deformity at the entheses secondary to the abnormal forces transmitted by the coalition.
References
Gray H. Anatomy of the human body. Philadelphia: Lea & Febiger; 1918.
Lee MS, Harcke HT, Kumar SJ, Bassett GS. Subtalar joint coalition in children: new observations. Radiology 1989; 172: 635–639.
Sarrafian SK. Anatomy of the foot and ankle: descriptive, topographic, functional. Philadelphia: Lippincott, William and Wilkins; 1993.
de Palma L, Santucci A, Ventura A, Marinelli M. Anatomy and embryology of the talocalcaneal joint. Foot Ankle Surg 2003; 9: 7–18.
Kumai T, Takakura Y, Akiyama K, Higashiyama I, Tamai S. Histopathological study of nonosseous tarsal coalition. Foot Ankle Int 1998; 19: 525–531.
Jotoku T, Kinoshita M, Okuda R, Abe M. Anatomy of ligamentous structures in the tarsal sinus and canal. Foot Ankle Int 2006; 27: 533–538.
Harris RI, Beath T. Etiology of peroneal spastic flatfoot. J Bone Jt Surg Br Vol 1948; 30: 624–634.
Kulik SA Jr, Clanton TO. Tarsal coalition. Foot Ankle Int 1996; 17: 286–296.
Cowell HR. Talocalcaneal coalition and new causes of peroneal spastic flatfoot. Clin Orthop Relat Res 1972; 85: 16–22.
Scranton PE. Treatment of symptomatic talocalcaneal coalitions. J Bone Jt Surg Am Vol 1987; 69A: 533–539.
Sijbrandij ES, van Gils AP, de Lange EE, Sijbrandij S. Bone marrow ill-defined hyperintensities with tarsal coalition: MR imaging findings. Eur J Radiol 2002; 43: 61–65.
Kumar SJ, Guille JT, Lee MS, Couto JC. Osseous and non-osseous coalition of the middle facet of the talocalcaneal joint. J Bone Joint Surg Am 1992; 74: 529–535.
Stormont DM, Peterson HA. The relative incidence of tarsal coalition. Clin Orthop Relat Res 1983; 28–36.
Solomon LB, Ruhli FJ, Taylor J, Ferris L, Pope R, Henneberg M. A dissection and computer tomograph study of tarsal coalitions in 100 cadaver feet. J Orthop Res 2003; 21: 352–358.
Mosier KM. Tarsal coalitions and peroneal spastic flat foot—a review. J Bone Jt Surg Am Vol 1984; 66A: 976–984.
Leonard MA. The inheritance of tarsal coalition and its relationship to spastic flat foot. J Bone Joint Surg Br 1974; 56B: 520–526.
Vamer KE, Michelson JD. Tarsal coalition in adults. Foot Ankle Int 2000; 21: 669–672.
Harris BJ. Anomalous structures in the developing human foot. Anat Rec 1955; 121: 399.
Gardner E, Gray DJ, Orahilly R. The prenatal development of the skeleton and joints of the human foot. J Bone Jt Surg Am Vol 1959; 41: 847–876.
Kawashima T, Uhthoff HK. Prenatal development around the sustentaculum tali and its relation to talocalcaneal coalitions. J Pediatr Orthop 1990; 10: 238–243.
Searle CP, Hildebrand RK, Lester EL, Caskey PM. Findings of fibular hemimelia syndrome with radiographically normal fibulae. J Pediatr Orthop B 2004; 13: 184–188.
Scranton PE Jr, McDermott JE. Pathologic anatomic variations in subtalar anatomy. Foot Ankle Int 1997; 18: 471–476.
Downey MS. Tarsal coalitions. A surgical classification. J Am Podiatr Med Assoc 1991; 81: 187–197.
Conway JJ, Cowell HR. Tarsal coalition: clinical significance and roentgenographic demonstration. Radiology 1969; 92: 799–811.
Bohne WH. Tarsal coalition. Curr Opin Pediatr 2001; 13: 29–35.
Cowell HR, Elener V. Rigid painful flatfoot secondary to tarsal coalition. Clin Orthop Relat Res 1983: 54–60.
Jayakumar S, Cowell HR. Rigid flatfoot. Clin Orthop Relat Res 1977: 77–84.
Jack EA. Bone anomalies of the tarsus in relation to peroneal spastic flat foot. J Bone Jt Surg Br Vol 1954; 36: 530–542.
Liu PT, Roberts CC, Chivers FS, et al. “Absent middle facet”: a sign on unenhanced radiography of subtalar joint coalition. Am J Roentgenol 2003; 181: 1565–1572.
Beckly DE, Anderson PW, Pedegana LR. The radiology of the subtalar joint with special reference to talo-calcaneal coalition. Clin Radiol 1975; 26: 333–341.
Resnick D. Talar ridges, osteophytes, and beaks: a radiologic commentary. Radiology 1984; 151: 329–332.
Lateur LM, Van Hoe LR, Van Ghillewe KV, Gryspeerdt SS, Baert AL, Dereymaeker GE. Subtalar coalition: diagnosis with the C sign on lateral radiographs of the ankle. Radiology 1994; 193: 847–851.
Pistoia F, Ozonoff MB, Wintz P. Ball-and-socket ankle joint. Skeletal Radiol 1987; 16: 447–451.
Crim JR, Kjeldsberg KM. Radiographic diagnosis of tarsal coalition. AJR Am J Roentgenol 2004; 182: 323–328.
Pachuda NM, Lasday SD, Jay RM. Tarsal coalition: etiology, diagnosis, and treatment. J Foot Surg 1990; 29: 474–488.
O’Neill DB, Micheli LJ. Tarsal coalition. A follow up of adolescent athletes. Am J Sports Med 1989; 17: 544–549.
Masciocchi C, D’Archivio C, Barile A, et al. Talocalcaneal coalition: computed tomography and magnetic resonance imaging diagnosis. Eur J Radiol 1992; 15: 22–25.
Nalaboff KM, Schweitzer ME. MRI of tarsal coalition: frequency, distribution, and innovative signs. Bull NYU Hosp Jt Dis 2008; 66: 14–21.
Moe DC, Choi JJ, Davis KW. Posterior subtalar facet coalition with calcaneal stress fracture. AJR Am J Roentgenol 2006; 186: 259–264.
Brekke MK, Lieberman R, Wright E, Green DR. Posterior facet talocalcaneal coalition. J Am Podiatr Med Assoc 2001; 91: 422–426.
Takakura Y, Kumai T, Takaoka T, Tamai S. Tarsal tunnel syndrome caused by coalition associated with a ganglion. J Bone Joint Surg Br 1998; 80: 130–133.
Percy EC, Mann DL. Tarsal coalition: a review of the literature and presentation of 13 cases. Foot Ankle 1988; 9: 40–44.
Rankin EA, Baker GI. Rigid flatfoot in young adults. Clin Orthop Relat Res 1974: 244–248.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linklater, J., Hayter, C.L., Vu, D. et al. Anatomy of the subtalar joint and imaging of talo-calcaneal coalition. Skeletal Radiol 38, 437–449 (2009). https://doi.org/10.1007/s00256-008-0615-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-008-0615-4