Abstract
Background
A variant form of subtalar coalition isolated to the posterior sustentaculum has been previously described, though its prevalence is not known and its relationship to the middle facet has not been characterized.
Objective
To determine the prevalence and morphological alterations of isolated posteromedial subtalar coalitions.
Materials and methods
Computed tomography (CT) images of the foot or ankle performed from 2004 to 2012 were reviewed and 97 patients (mean age: 13.3+/-2.9 years; range: 9-19 years) with subtalar coalition were identified. In 41 (42%) of these, the condition was bilateral, yielding a total of 138 subtalar coalitions. In the 33 patients where CT demonstrated isolated posteromedial subtalar coalitions, multiplanar reformats along the long axis of the sustentaculum tali were generated, from which the anteroposterior dimensions of the sustentaculum tali and middle facet were measured. Posterior sustentaculum measurements defining the posterior extension of the sustentaculum beyond the middle facet were directly measured by two radiologists. Ratios of middle facet to posterior sustentaculum measurements were calculated. Thirty-three patients undergoing CT for ankle fracture served as controls.
Results
Ninety-seven of 138 coalitions (70.2%) affected the middle facet and 2/138 (1.4%) involved the posterior facet. There were 39 (28.2%) posteromedial subtalar coalitions in 33 patients. Mean AP measurements of the middle facet and posterior sustentaculum in patients with posteromedial subtalar coalitions were 12.6 mm and 18.2 mm, respectively, compared to 16.6 mm and 9.2 mm in controls (P<0.001). Mean middle facet/posterior sustenaculum (MF/PS) ratios were 0.74 for posteromedial subtalar coalitions vs. 1.92 for controls (P<0.001).
Conclusion
Posteromedial subtalar coalitions comprise more than one-quarter of subtalar coalitions, and are associated with an intact, but shorter, middle facet and longer sustentaculum tali. This observation may aid in accurate diagnosis and management of this relatively common disorder.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tarsal coalition is a congenital condition characterized by abnormal bridging between two or more tarsal bones, which often leads to heel valgus deformity, pain and peroneal muscle spasm [1, 2]. Tarsal coalitions may exist in isolation and may also be associated with other conditions and syndromes, including carpal coalition, symphalangism, phocomelia, fibular hemimelia and Nievergelt syndrome [3]. The most common types of tarsal coalition are subtalar and calcaneonavicular, with other types occurring infrequently [1, 4]. The subtalar joint consists of a posterior facet immediately posterior to the sinus tarsi, and a middle facet formed by the sustentaculum tali and the articulating facet/s of the talus [5]. An anterior articular facet is variably present and is the smallest of the three facets [5]. The sinus tarsi and the tarsal canal form a cone-shaped region between the posterior and middle subtalar joint, which is larger laterally than medially, and courses from posteromedial to anterolateral (Fig. 1) [6]. Classic teaching and review of the literature indicate that subtalar coalitions are primarily an abnormality of the middle facet [1, 5, 7–9], though coalitions involving the posterior and anterior facets occur in rare cases [5]. A recent classification scheme for subtalar coalitions has been described in adults, though it does not address which articular facets are involved [10]. Middle facet subtalar coalitions are often associated with a more severe valgus deformity of the foot than other tarsal coalitions [1, 11]. There are reported cases of subtalar coalitions involving the sustentaculum tali posterior to and sparing the middle facet [5, 12, 13], though the prevalence of this type has not been established. Furthermore, coalitions in this location have been given a variety of names in the literature, including “posteromedial” [13], “extra-articular” [5], “extra-articular with or without os sustentaculum” [14], “posterior to sustentaculum tali” [12], “peripheral posterior” [15] and even “posterior facet” [16], revealing the confusion surrounding the location of these coalitions with respect to the middle and posterior facets, and the nomenclature used to define them. Recognition of the location and morphology of this type of tarsal coalition is important for accurate diagnosis and treatment. Computed tomography (CT) with both two-dimensional (2-D) and three-dimensional (3-D) reconstructions allows for excellent anatomical delineation of coalitions, which is valuable for surgical decision-making [15]. Coronal CT images through a posteromedial subtalar coalition demonstrate the normal middle and posterior facets, as the coalition is isolated from the sustentaculum posterior to the middle facet, a feature that may be better appreciated on sagittal images (Fig. 2) or 3-D reconstructions (Fig. 3). The surgical resection of a posteromedial subtalar coalition may be greatly simplified when the coalition is well-characterized preoperatively with CT [15]. The purpose of this study was to determine the prevalence of posteromedial subtalar coalitions (those exclusively posterior to the middle facet) in children, explore the associated morphological abnormalities of the middle facet and sustentaculum tali in this condition, and propose an effective marker for diagnosis.
Normal anatomy. a Three-dimensional reconstructed CT image of a calcaneus in a 14-year-old boy as viewed from above demonstrates the posterior facet (PF), middle facet (MF) and anterior facet (AF). The tarsal canal courses posteromedially from the sinus tarsi to posterior to the sustentaculum tali (double-headed arrow in a; * in b, c). Three-dimensional reconstructed image of the subtalar joint as viewed medially (b) and anterolaterally (c) in the same patient demonstrates MF, PF and tarsal canal (*). The patient was undergoing CT for evaluation of a tibial fracture. M medial, L lateral, P posterior, A anterior
CT images from a 10-year-old girl with posteromedial subtalar coalition. a Sagittal reformatted image demonstrates a non-osseous coalition (white arrow) posterior to the middle facet (black arrow). b, c Coronal reformatted images demonstrate the normal middle facet (b, black arrow) and the coalition (c, white arrow), which lies medial to the posterior facet (arrowheads)
Three-dimensional reconstructed CT images illustrate the articular surface of the calcaneus as viewed from above from a 12-year-old girl (a) with posteromedial subtalar coalition and a 16-year-old boy (b) with triplane fracture. The tarsal canal is denoted by the black arrows. The coalition in patient (a) is posterior to the tarsal canal and spares the middle facet. The white arrowheads denote the posterior sustentaculum. The middle facet (MF) comprises a much smaller portion of the sustentaculum tali in the patient with coalition (a) compared to the patient with triplane fracture (b). A anterior, P posterior, M medial, L lateral
Materials and methods
Patient populations
This HIPAA-compliant, retrospective cross-sectional study was conducted at a large urban pediatric hospital. It was approved by the Institutional Review Board and informed consent was waived. A search of the picture archiving and communication system (PACS) for all ankle/hindfoot CT scans performed between January 2004 and May 2012 in patients 0-20 years old generated a list of 1,352 examinations. CT images were reviewed by one pediatric musculoskeletal radiologist (S.D.B., with 7 years’ experience) who noted the presence or absence of subtalar coalition. Patients were excluded if the images did not extend through the entirety of the subtalar joint, or if there was a prior history of foot or ankle surgery.
Ninety-seven patients (49 male, 48 female; mean age: 13.3+/-2.9 years; range: 8-19 years) with subtalar coalition were identified. Review of the electronic medical record for each patient confirmed the presence of foot or ankle pain in all patients as the indication for imaging. Imaging included both feet and ankles in 95 patients with non-traumatic pain and clinical concern for tarsal coalition, and unilateral imaging for two patients with pain after trauma and suspected tibia fracture on radiographs. Forty-one patients had bilateral and 56 patients had unilateral coalitions. CT images of the 138 coalitions in these patients were reviewed further by the same radiologist who performed the initial image review with note of the laterality of the coalition, whether it was osseous or non-osseous, and the location of the coalition. Coalitions were defined as one of three types, according to the involvement of the posterior facet, posterior sustentaculum or middle facet. Involvement of the anterior facet was not recorded given the variability of the normal anterior facet anatomy in the population and the high prevalence of conjoined anterior and middle facets [17].
A subset of the coalition population with posteromedial subtalar coalition was identified, consisting of 39 ankles in 33 patients (18 male, 15 female; mean age: 13.62+/-2.60 years; range: 9-19 years). In addition to the six patients with bilateral posteromedial subtalar coalitions, four of the patients in this cohort had contralateral middle facet coalitions that were not included in the cohort. All other patients had unilateral coalition. This cohort was involved in further quantitative assessment as detailed below. The patients with middle facet coalition were not involved in further quantitative assessment given that the location of the coalition would preclude accurate measurement of the middle facet.
A control group of patients with distal tibial fractures was also selected from the same parent set of 1,352 CTs. Three hundred and seven cases were identified and 33 age- and gender-matched patients (18 male, 15 female; mean age: 13.7+/-1.8 years; range: 10-18 years) were randomly selected.
Image acquisition
The CT techniques for the 33 patients with posteromedial subtalar coalition and the 33 control patients varied over the study period. Three studies were performed on a single-detector CT (HiSpeed; GE Medical Systems, Milwaukee, WI) with images acquired helically at 1-mm slice thickness. Twenty-five studies were performed on a 16-detector scanner (Lightspeed Pro, GE Medical Systems), and 18 studies were performed on a 32-detector scanner (Lightspeed Pro, GE Medical Systems). These images were acquired helically at 0.625-mm slice thickness and were reconstructed to 1.25 mm using a bone algorithm. Eleven studies were acquired helically on a Somatom Sensation 40 scanner (Siemens Corporation, Erlangen, Germany) using a slice thickness of 0.75 mm reconstructed to 1.0 mm using a bone algorithm, and 9 studies were performed helically on a Somatom Sensation 64 scanner (Siemens) with slice thickness of 0.60 mm reconstructed to 1.0 mm using a bone algorithm. For patients with suspected tarsal coalition, both feet were placed in the gantry with the knees and hips bent and the feet plantar flexed on the table surface. For patients with distal tibial fractures, the knees and hips were extended and the ankles were maintained in neutral position. Images were acquired perpendicular to the long axis of the foot for suspected coalition and parallel to the long axis of the foot for patients with distal tibial fracture. All patients were scanned without intravenous contrast material.
Image interpretation
CT scans were reviewed on a PACS workstation by a second pediatric radiologist (P.K.K., with 33 years’ experience) to confirm signs of subtalar coalition. Coalitions were defined as osseous or non-osseous based on established CT criteria, including demonstration of an osseous bar between the talus and calcaneus for osseous coalitions [18–20], or the presence of articular narrowing with cystic joint irregularity or subchondral sclerosis for non-osseous coalitions [18–20]. The tarsal canal was defined as the landmark separating the middle facet from the posterior sustentaculum. In normal ankles, the tarsal canal is an anatomical structure that extends medially from the tarsal sinus at a 45-degree angle posterior to the middle facet and the sustentaculum tali (Fig. 1) [6, 21, 22]. Coalitions were defined as middle facet, posteromedial subtalar or posterior facet. Middle facet coalitions were defined by a coalition that involved the middle facet of the subtalar joint with or without obliteration of the tarsal canal (Fig. 4). Posteromedial subtalar coalitions were defined as a coalition posterior to the tarsal canal and separate from (medial to) the posterior facet with a normal middle facet (Fig. 5). Posterior facet coalitions were defined as lateral to the sustentaculum, entirely confined to the posterior facet, with a normal middle facet and sustentaculum tali.
Middle facet coalition. Sagittal reformatted image from a CT of the right ankle in an 11-year-old boy with ankle pain demonstrates a non-osseous coalition extending the length of the sustentaculum (black arrows). The tarsal canal is obliterated and the posterior sustentaculum is involved in the coalition
Posteromedial subtalar coalition. Sagittal reformatted CT image through the sustentaculum tali in a 10-year-old girl with hindfoot pain. The middle facet is normal (black arrows), the tarsal canal is visualized (white arrowhead) and the non-osseous coalition is confined to the posterior sustentaculum (black arrowhead)
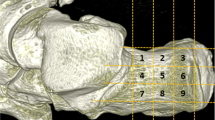
Multiplanar reformatting was performed on the subset of study patients with posteromedial subtalar coalitions and on control patients. Reformatted planes were aligned along the axis of the sustentaculum tali (Fig. 6). The reformats were performed by one radiologist (S.D.B.) using Synapse 3-D software (Fujifilm Corp., Tokyo Japan). Images were reformatted to 1.0-mm-thick sections using a bone algorithm. These images were transferred to a PACS workstation for review. The AP dimensions of the middle facet and sustentaculum tali were recorded independently by two pediatric radiologists (S.D.B. and D.Y.J., with 7 and 5 years’ experience, respectively) using electronic calipers. Measurements were acquired directly from sagittal reformatted images, and axial images were available at the PACS workstation for reference purposes during measurements. The dimension of the posterior sustentaculum was measured from the sagittal reformatted images as that portion of the sustentaculum tali lying posterior to the middle facet (Fig. 7). Reader 1 (S.D.B.) performed two sets of measurements for each patient in both study and control populations for assessment of intrareader variability, separated by 3 months to avoid recall bias. A ratio of the length of the middle facet over the length of the posterior sustentaculum and a ratio of the length of the middle facet to the length of the sustentaculum tali were determined.
Posteromedial subtalar coalition. Sagittal reformatted image through the sustentaculum tali in a 12-year-old boy with posteromedial subtalar coalition illustrates measurement technique. The white double-headed arrow delineates the AP measurement of the middle facet, and the longer black double-headed arrow denotes the length of the entire sustentaculum tali. The shorter black double-headed arrow denotes the AP dimension of the posterior sustentaculum
Statistical analysis
Group differences with respect to gender and age were compared using the GENMOD procedure of SAS using logit, identity and identity links, respectively (SAS Institute Inc. 2011. SAS/STAT® 9.3 User’s Guide). The difference between posteromedial subtalar coalitions and middle facet coalitions was compared with respect to the odds of being osseous via a random effects logistic model using the NLMIXED procedure of SAS.
The comparison between study (posteromedial subtalar coalition) and control (tibial fracture) groups was based on 72 ankles from 66 patients. Gamma multiplicative models with log links and estimated by generalized estimating equation methods were used to compare groups with respect to the following outcomes: middle facet, sustentaculum tali, posterior sustentaculum, middle facet/sustentaculum tali (MF/ST), and middle facet/posterior sustentaculum (MF/PS). These models provided estimates of group means, and ratios of means adjusting for gender, age and CT section thickness. Corresponding 95% confidence intervals, and P-values for tests of group equality, were calculated. Models were fit using the GENMOD procedure of SAS using a robust variance matrix based on a working independence correlation structure.
For each marker, empirical receiver operator characteristic (ROC) curves and the area under them (AROC) were calculated by the logistic procedure of SAS. Ninety-five percent confidence intervals for AROC were calculated by the percentile bootstrap method using 10,000 bootstrap samples. Resampling was done within cohort. ROC curves were compared using the method proposed by DeLong et al. [23]. For the purpose of ROC analysis, the 72 ankles were treated as independent ankles. Intraobserver reliability (repeatability) between two measurements from a single reader was estimated via a components of variance model. This method was also used to estimate interobserver reliability (reproducibility) between the two readers. Models were fit using the NLMIXED procedure of SAS.
Results
Involvement of the posterior facet, posterior sustentaculum and middle facet in the 138 coalitions is presented in Table 1. Thirty-nine of 138 (28.2%) of subtalar coalitions were of the posteromedial subtalar type. Thirty-three of 138 (24%) of all subtalar coalitions were defined as osseous and 105/138 (76%) were non-osseous. The percent of the ankles that were osseous was 0% (0/39) with posterior subtalar coalition and 34% (33/97) with a coalition involving the middle facet (P<0.001).
The subset of 33 patients with 39 posterior subtalar coalitions (27 unilateral, 6 bilateral) was not statistically different from the control population of 33 patients with respect to age or gender (Table 2).
The mean anteroposterior measurements of the middle facet, sustentaculum tali and the posterior sustentaculum in study and control groups are shown in Table 3. The mean middle facet was shorter and the mean sustentaculum tali longer in posteromedial subtalar coalition patients compared to controls. The mean posterior sustentaculum was longer in posteromedial subtalar coalition patients compared to controls (Table 3). ROC curves for middle facet and the ratio of the middle facet over the sustentaculum tali (MF/ST) measurements demonstrate that while both measurements are able to distinguish between cohorts, the ratio is more effective (Fig. 8). Areas under the ROC curves were 0.87 for middle facet and 0.97 for MF/ST ratio. These areas estimate the probability of correctly classifying a random pair of patients, one from each cohort, and thus the corresponding odds of correct classification were 6.57 for middle facet and 38.60 for MF/ST ratio giving an odds ratio in favor of the ratio of 5.87 (P=0.002).
Receiver operator characteristic curves for measurements of the medial facet (red, area under the ROC curve [AROC] = 0.87, 95% confidence interval [CI] = [0.80, 0.93]) and medial facet/sustentaculum talus (MF/ST) (blue, AROC = 0.97, 95% CI = [0.95, 0.99]) demonstrate that while both measurements are effective at distinguishing between cohorts (controls vs. posteromedial subtalar coalition), the MF/ST measurement is more effective
Interobserver correlations between measurements by two readers were 0.85, 0.88 and 0.88 for middle facet, sustentaculum tali and posterior sustentaculum, respectively. Intraobserver correlations between measurements were 0.95, 0.96 and 0.97, respectively.
Discussion
Posteromedial subtalar coalitions were described more than 60 years ago by Harris and Beath [11]. Once considered an uncommon variant of subtalar coalition [13], Lee et al. [12] found posterior sustentaculum coalitions to be the most common type of coalition, occurring in 17 of 29 pediatric patients. The authors reported that the sustentaculum tali was qualitatively hypoplastic [12]. Our results also indicate that in more than one-quarter of patients with subtalar coalition the middle facet is spared, as evidenced by the visualization of the tarsal canal anterior to the coalition and posterior to the facet.
The dimensions of the middle facet and the sustentaculum tali in patients with posteromedial subtalar coalitions have not yet been systematically studied. Although the facet may appear normal in these patients on CT, our quantitative analysis reveals that it is hypoplastic compared to normal controls. An apparently normal middle facet may confound the diagnosis of coalition if the posterior sustentaculum is not carefully scrutinized for evidence of coalition. The relative size of the middle facet compared to the sustentaculum tali is a helpful marker of posteromedial subtalar coalition. Likewise, comparing the anteroposterior dimension of the middle facet to the anteroposterior dimension of the posterior sustentaculum may provide a helpful diagnostic clue to the presence of a posteromedial subtalar coalition, particularly when the CT findings are subtle. The middle facet in patients with posteromedial subtalar coalition is usually smaller than the posterior sustentaculum, whereas the middle facet is approximately twice as large as the posterior sustentaculum in normal patients. These observations may have important clinical and prognostic implications, particularly in patients for whom surgery is planned [15].
While non-osseous coalitions comprised 76% of the total number of subtalar coalitions, 100% of our posteromedial subtalar coalitions were non-osseous. This finding is in keeping with previous reports in the literature. Kumar et al. [24] reported that most osseous coalitions involved the middle facet while all fibrous coalitions were located in the posterior aspect of the middle facet or posterior to the sustentaculum tali. Lee et al. [12] reported only 1 osseous posteromedial subtalar coalition in 17 patients vs. 3 osseous coalitions in the remaining 12 patients with a coalition involving one or more facets. Our findings substantiate these previous reports suggesting that osseous posteromedial subtalar coalitions are less common than osseous middle facet coalitions.
This study has several limitations. The control population of patients with tibial fractures was presumed to be asymptomatic prior to injury. Given the traumatic nature of their injuries, the patients may not have been questioned about symptoms prior to their injury. Our study population was derived from patients undergoing CT of the feet and ankles, and does not reflect the true prevalence of asymptomatic subtalar coalition in the population. There may have been an element of recall bias by having only one reader perform two sets of measurements. This effect may be mitigated by separating the readings by a span of 3 months. Though readers were blinded to diagnosis, the features of coalition were often present on the reformatted images evaluated for measurement. We attempted to address this potential bias by imposing strict measurement guidelines.
Conclusion
Posteromedial subtalar coalitions are a relatively under-recognized form of subtalar coalitions in children. While subtalar coalitions are thought to represent a primary abnormality of the middle facet, the middle facet is not uniformly involved in patients with coalition. Despite sparing of the middle facet with posteromedial subtalar coalitions, the dimensions of the middle facet are abnormal. In our population of symptomatic children, posteromedial subtalar coalitions constituted more than one-quarter of all subtalar coalitions, and had a higher prevalence of being non-osseous (100%) compared to coalitions involving the middle facet (74%). The length of the posterior sustentaculum was twice as large in posteromedial subtalar coalition patients compared to controls. The dimensions of the middle facet and sustentaculum tali help aid in diagnosing posteromedial subtalar coalitions, as the middle facet is hypoplastic relative to the elongated sustentaculum tali. Given that these patients have an intact, albeit small, middle facet, it is conceivable that these patients may have improved function and stability postoperatively compared to patients with a coalition extending into the middle facet if the resection can be limited to the precise area of the coalition. CT with 2-D and 3-D reconstructions delineating the coalition can provide valuable pre-operative information to the surgeon to aid in the surgical approach [15]. Future prospective studies will be important in determining whether posteromedial subtalar coalitions represent a variant of middle facet coalition versus a distinct entity, and whether these anatomical differences correlate with clinical outcomes.
References
Mosier KM, Asher M (1984) Tarsal coalitions and peroneal spastic flat foot. J Bone Joint Surg Am 66A:976–984
Harris RI (1965) Retrospect-peroneal spastic flat foot (rigid valgus foot). J Bone Joint Surg Am 47:1657–1667
Kernbach KJ (2010) Tarsal coalitions: etiology, diagnosis, imaging, and stigmata. Clin Podiatr Med Surg 27:105–117
Stormont DM, Peterson HA (1983) The relative incidence of tarsal coalition. Clin Orthop Relat Res 181:28–36
Linklater J, Hayter CL, Vu D et al (2009) Anatomy of the subtalar joint and imaging of talo-calcaneal coalition. Skeletal Radiol 38:437–449
Klein MA, Spreitzer AM (1993) MR imaging of the tarsal sinus and canal: normal anatomy, pathologic findings, and features of the sinus tarsi syndrome. Radiology 186:233–240
Chew F (2003) Developmental and congenital conditions. In: Musculoskeletal imaging. Lippincott Williams & Wilkins, Philadelphia, pp 432-433
Laor T (2008) Congenital malformations of bone. In: Slovis TL (ed) Caffey’s pediatric diagnostic imaging, 11th edn. Mosby, Philadelphia, pp 2602–2603
Cass AD, Camasta CA (2010) A review of tarsal coalition and pes planovalgus: clinical examination, diagnostic imaging, and surgical planning. J Foot Ankle Surg 49:274–293
Lim S, Lee HK, Bae S et al (2013) A radiological classification system for talocalcaneal coalition based on a multi-planar imaging study using CT and MRI. Insights Imaging 4:563–567
Harris RI, Beath T (1948) Etiology of peroneal spastic flat foot. J Bone Joint Surg (Br) 30:624–634
Lee MS, Harcke HT, Kumar SJ et al (1989) Subtalar joint coalition in children: new observations. Radiology 172:635–639
McNally EG (1999) Posteromedial subtalar coalition: imaging appearances in three cases. Skeletal Radiol 28:691–695
Yun SJ, Jin W, Kim GY et al (2015) A different type of talocalcaneal coalition with os sustentaculum: the continued necessity of revision of classification. AJR Am J Roentgenol 205:W612–W618
Rosanzky A, Varley E, Moor M et al (2010) A radiologic classification of talocalcaneal coalitions based on 3D reconstruction. J Child Orthop 4:129–135
Staser J, Karmazyn B, Lubicky J (2007) Radiographic diagnosis of posterior facet talocalcaneal coalition. Pediatr Radiol 37:79–81
Hyer CF, Lee T, Block AJ et al (2002) Evaluation of the anterior and middle talocalcaneal articular facets and the Evans osteotomy. J Foot Ankle Surg 41:389–393
Newman JS, Newberg AH (2000) Congenital tarsal coalition: multimodality evaluation with emphasis on CT and MR imaging. Radiographics 20:321–332
Emery KH, Bisset GS 3rd, Johnson ND et al (1998) Tarsal coalition: a blinded comparison of MRI and CT. Pediatr Radiol 28:612–616
Wechsler RJ, Schweitzer ME, Deely DM et al (1994) Tarsal coalition: depiction and characterization with CT and MR imaging. Radiology 193:447–452
Cahill DR (1965) The anatomy and function of the contents of the human tarsal sinus and canal. Anat Rec 153:1–17
Jotoku T, Kinoshita M, Okuda R et al (2006) Anatomy of ligamentous structures in the tarsal sinus and canal. Foot Ankle Int 27:533–538
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operator characteristic curves: a non-parametric approach. Biometrics 44:837–845
Kumar SJ, Guille JT, Lee MS et al (1992) Osseous and non-osseous coalition of the middle facet of the talocalcaneal joint. J Bone Joint Surg Am 74:529–535
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Bixby, S.D., Jarrett, D.Y., Johnston, P. et al. Posteromedial subtalar coalitions: prevalence and associated morphological alterations of the sustentaculum tali. Pediatr Radiol 46, 1142–1149 (2016). https://doi.org/10.1007/s00247-016-3584-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3584-0