Abstract
Objective
The symptoms and physical findings of intersection syndrome have been well described in the clinical medical literature. However, the magnetic resonance imaging (MRI) findings in patients with intersection syndrome of the forearm have only recently been described in a small number of patients. We review our experience with imaging of intersection syndrome, describe previously unreported MRI findings, and emphasize modifications to MRI protocols for its evaluation.
Materials and methods
Institutional review board approval was obtained for this retrospective review of patients with MRI findings consistent with intersection syndrome of the forearm during the period from January 2004 to September 2006. Six patients were identified, three males and three females, with an average age of 39.3 years. The MRI examinations were reviewed to assess signal abnormalities within and adjacent to the first and second dorsal extensor tendon compartments (DETC): tendinosis, peritendinous edema or fluid, muscle edema, subcutaneous edema, and juxtacortical edema. The overall longitudinal extent of signal alterations was measured as well as the distance from Lister’s tubercle to the crossover of the first and second DETC.
Results
Review of the MRIs showed increased intrasubstance tendon signal suggesting tendinosis in two of the six patients, peritendinous edema or fluid in all six patients, muscle edema in five of the six patients, and subcutaneous edema in three of the six patients. Juxtacortical edema was seen in one patient. Peritendinous edema or fluid extended distally beyond the radiocarpal joint in three of the six patients. The average distance from Lister’s tubercle to the crossover of the first and second DETC was 3.95 cm, in keeping with recently published data.
Conclusion
Intersection syndrome is an uncommon MRI diagnosis. In addition to the previously described MRI findings of edema adjacent to the first or second DETC, possibly with proximal extension and subcutaneous edema, we have identified additional abnormalities: tendinosis, muscle edema, and juxtacortical edema. In addition, our review shows that first and second DETC signal abnormalities in patients with intersection syndrome are not necessarily limited to the site of crossover but can extend distally beyond the radiocarpal joint. As standard wrist protocols may not include the area of intersection between the first and second DETC, coverage may need to be extended to the mid-forearm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intersection syndrome is a well-described overuse syndrome of the distal forearm. It is a noninfectious inflammatory process located at the area of intersection of the first (abductor pollicis longus (APL) and extensor pollicis brevis) and second (extensor carpi radialis longus and extensor carpi radialis brevis) dorsal extensor tendon compartments (DETC) in the dorsoradial aspect of the distal forearm, located approximately 4 cm proximal to Lister’s tubercle. The typical symptoms include pain, erythema, edema, tenderness to palpation, and crepitance with flexion and extension of the wrist.
The differential diagnosis includes de Quervain’s tenosynovitis or other inflammatory tenosynovitis, wrist ligament sprain, muscle strain, ganglion cyst, infection, soft tissue neoplasm, or entrapment of the dorsal radial sensory nerve as it emerges beneath the brachioradialis (Wartenberg’s syndrome) [1]. The possibility of cellulitis is sometimes raised due to the swelling and erythema sometimes associated with intersection syndrome. Magnetic resonance imaging (MRI) can be diagnostic in uncertain clinical cases.
We review our experience with imaging of intersection syndrome, describe additional MRI findings of intersection syndrome that have not been previously reported, and emphasize modifications to MRI protocols for its evaluation. We also include a brief review of the literature concerning this entity.
Methods
We retrospectively reviewed the clinical and MRI findings consistent with intersection syndrome of the distal forearm at our institution and affiliated hospitals during the period from January 2004 to September 2006. The patients were selected by a radiology information system search of all MRIs of the forearm or wrist reported by our home institution, local regional practice, and national teleradiology practice. The total number of MRI examinations of the forearm or wrist over this period was 1,289 (359 cases in 2004, 516 cases in 2005, and 414 cases in 2006 up until September). Subsequently, a keyword search was performed using “intersection,” “crossover,” “pollicis,” and “radialis”. The selected reports were then reviewed for MRI features of intersection syndrome and then correlated with the clinical findings. This selection methodology yielded six cases. The incidence of intersection syndrome in our referral population for MRI was 0.47% (6/1,289).
Four of the MRIs of the forearm or wrist were performed on 1.5-T MRI scanners. The two remaining patients were imaged with 1.0- and 0.9-T MRI scanners. Due to the varying institutions in which the scans were performed, various technical parameters for these MRI examinations were employed. The commonality that all six patients shared was fluid-sensitive sequences performed in the coronal and axial planes (fat-saturated T2 or STIR), which we feel are the most vital sequences necessary in order to image and diagnose intersection syndrome.
The six scans were evaluated in consensus by two radiologists experienced in musculoskeletal MRI. The MRI examinations were reviewed to assess signal abnormalities within and adjacent to the first and second DETC: tendinosis, peritendinous edema or fluid, muscle edema, subcutaneous edema, and juxtacortical edema. In addition, the overall longitudinal extent of signal alterations was measured as well as the distance from Lister’s tubercle to the crossover of the first and second DETC. Tendinosis was determined by noting increased intrasubstance signal within the tendon. Peritendinous edema, muscle edema, and subcutaneous edema were subjectively graded as mild, moderate, and severe.
We used the fluid-sensitive sequences in the axial plane primarily to determine the signal abnormalities within and adjacent to the first and second compartments and the longitudinal planes to measure the overall longitudinal extent of signal abnormalities
Results
The MRI findings and clinical histories of the six patients with intersection syndrome were reviewed. The patients included three males (ages 28, 33, and 45) and three females (ages 31, 43, and 56) with a mean age of 39.3 years. Results are summarized in Table 1.
All six patients were referred for MRI for pain and swelling in the distal forearm. In four of six patients, there was clinical concern for mass. None carried the clinical diagnosis of intersection syndrome. The first patient (Fig. 1) noted an increase in the size of the left forearm with discomfort and pain that bothered her when she typed on the computer, with a soft and fluctuant mass on examination that felt like a lipoma. The second patient had an injury at work 2 weeks prior to the initial MRI examination and developed left wrist and forearm pain, with a painful mass approximately 10 cm proximal to the wrist. The third patient (Fig. 2) presented 15 days prior to the MRI with left distal forearm pain after laying brick work all day. The fourth patient (Fig. 3) had been having chronic pain for several months in the distal left forearm in which she had been suspected of having “chronic de Quervain’s tenosynovitis” versus a forearm mass. The fifth patient (Fig. 4) developed right forearm pain and swelling after skiing. The sixth patient (Fig. 5) presented with a “soft tissue lump” over the distal radial forearm with pain and swelling in which tenosynovitis versus ganglion cyst were of clinical concern.
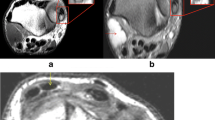
Patient 1. A 1.56-year-old female who presented with palpable soft and fluctuant mass. a Contrast-enhanced axial fat-saturated T1-weighted image (TR/TE, 550/14) at a level just proximal to the intersection of the first and second DETC. Enhancing juxtacortical edema (arrow) is seen along the dorsum of the distal radius. The musculotendinous junction of the first extensor compartment is seen just dorsal to the radius at the 12 o’clock position. Peritendinous edema is noted involving the second DETC. b Contrast-enhanced fat-saturated T1-weighted image (550/14) at a level just distal to the intersection of the first and second DETC. There is increased intrasubstance signal in the first DETC consistent with tendinosis. Peritendinous edema is again seen involving the second DETC. c Axial fat-saturated T2-weighted image (4,050/81) at a level just proximal to the intersection of the first and second DETC. There is a mild juxtacortical edema along the dorsum of the distal radius, peritendinous edema, and mild subcutaneous edema (arrows). The first DETC tendons are seen at the 1 o’clock position of the distal radius. The second DETC tendons are seen overlapping each other at the 3 o’clock position of the distal radius
Patient 3. A 33-year-old male who presented with left distal forearm pain and swelling after laying brick work all day. Axial fat-saturated turbo spin echo T2-weighted image (4,460/83) at a level just proximal to the intersection of the first and second DETC. A marker indicates the area of concern (asterisk). Mild peritendinous edema is noted in the second DETC with moderate subcutaneous edema. There is also mild intramuscular and perimuscular edema in the first extensor compartment muscles
Patient 4. A 31-year-old female with several months of chronic distal forearm pain. Contrast-enhanced coronal fat-saturated T1-weighted image (508/14) demonstrates severe peritendinous, muscle, and subcutaneous edema. One of the tendons of the first extensor compartment is seen distally on the radial side. Proximally, the second extensor compartment muscles and tendons are seen
Patient 5. A 43-year-old female with right forearm pain and swelling after a skiing injury. Axial fat-saturated turbo spin echo T2-weighted image (2,660/108) at a level near the intersection of the first and second DETC shows moderate muscle edema (asterisk) within the first extensor compartment muscles. Mild peritendinous edema is also depicted
Patient 6. A 45-year-old male with “soft tissue lump” over the distal radial forearm with pain and swelling. Proton-density images are shown for better anatomy (T2 images show similar findings). a Sagittal fat-saturated proton-density image (4,140/15) shows mild peritendinous edema of the extensor carpi radialis longus tendon of the second extensor compartment extending distal to the radiocarpal joint (bold arrow) and mild muscle edema proximally (thin arrows). b Axial fat-saturated proton-density image (3,300/14) demonstrates mild peritendinous edema involving the first and second DETC, with flattening and increased intrasubstance signal indicating tendinosis involving the first DETC (abductor pollicis longus and extensor pollicis brevis)
Four patients had radiographs of the wrist or forearm just prior to the MRI, which all revealed unremarkable findings.
Review of the MRIs showed increased intrasubstance tendon signal suggesting tendinosis in the first and sixth patient (2/6 = 33%; Figs. 1b and 5b). Both patients demonstrated mild tendinosis in the first DETC; however, the sixth patient also had flattening and attenuation of the first DETC. At least mild peritendinous edema at the site of intersection of the first and second DETC was universally seen in all six patients (6/6 = 100%), with the first patient showing moderate peritendinous edema and the fourth showing severe peritendinous edema. At least mild muscle edema (Figs. 3 and 4) was seen in the first or second dorsal extensor compartment muscles in five of the six patients (5/6 = 83%), with the second patient demonstrating no appreciable muscle edema. The first and fifth patient subjectively had moderate muscle edema and the fourth patient had severe muscle edema. Subcutaneous edema (Figs. 1c, 2, and 3) was seen in three of the six patients (3/6 = 50%). Mild subcutaneous edema was seen in the first patient; moderate subcutaneous edema was seen in the third patient, and severe subcutaneous edema was seen in the fourth patient. Juxtacortical edema (Fig. 1a,c) was observed in the first patient (1/6 = 17%).
Peritendinous edema or fluid extended distally beyond the radiocarpal joint (Fig. 5a) in the fourth, fifth, and sixth patients (3/6 = 50%). The overall longitudinal extent of the peritendinous edema in descending order of the six patients measured 6.8, 1.6, 5.2, 12.2, 10.7, and >8.7 cm (mean > 7.5 cm). The most proximal extent of involvement was incompletely imaged in the sixth patient; therefore, the measurement of 8.7 cm may be underestimated.
The first and fourth patients had MRI examinations before and after intravenous contrast. The areas of enhancement found in both patients who received IV contrast correlated to the areas of edema and inflammation seen on fluid-sensitive sequences (Fig. 1a,c).
The average distance from Lister’s tubercle to the crossover of the first and second DETC was 3.95 cm, in keeping with recently published data [2]. Of note, the second patient had an initial MRI of the wrist utilizing a standard wrist protocol that did not extend proximally enough to cover the area of intersection between the first and second DETC. The patient came back 1 week later for reimaging of the distal forearm, which revealed signal changes at the intersection between the first and second DETC, 4.9 cm proximal to Lister’s tubercle, consistent with intersection syndrome.
Discussion
Intersection syndrome is a relatively common overuse disorder of the forearm, thought to result from friction or entrapment between the musculotendinous junction of the first extensor compartment and the tendons of the second extensor compartment [3]. The intersection occurs at an angle of approximately 60°. This overuse syndrome has been reported in rowing, canoeing, racket sports, weight lifting, skiing, and other sports that involve repetitive use of the wrist [4, 5]. It has also been reported in agricultural workers who do much of the cultivation by hand [6]. It is most commonly seen in workers whose activities involve repetitive flexion and extension of the wrist. However, it tends to occur with the onset of a new activity rather than a condition that develops from prolonged exposure to activities involving repetitive wrist motion [1].
The name “intersection syndrome” was first introduced by Dobyns et al. [7] but was first described by Velpeau in 1841. It has also been referred to in the literature as peritendinitis crepitans, crossover syndrome, oarsmen’s wrist, squeaker’s wrist, bugaboo forearm, adventitial bursitis, subcutaneous perimyositis, and APL syndrome [8, 9]. It is distinct from the recently reported “distal intersection tenosynovitis” of the wrist which occurs more distally, at the level of the carpus, at the site of crossover between the second and third DETC [10].
Intersection syndrome is usually managed conservatively. Initially, treatment includes modification of work activities to reduce stress on the wrist and splinting [11]. Oral nonsteroidal anti-inflammatory medication or topical ice-pack placement can also provide relief. If symptoms persist, a long-acting steroid can be injected into the second dorsal compartment [8]. Surgery to decompress the area of intersection is usually performed only as a last resort in those patients whose symptoms are refractory to conservative measures [4].
A recent original report of MRI features of intersection syndrome of the forearm reviewed three patients with intersection syndrome [9]. Similar to our study, all of their three patients showed peritendinous edema around the first and second DETC, which is the most important finding in making the MRI diagnosis of intersection syndrome. Proximal extension of peritendinous edema as well as mild subcutaneous edema was also reported [9].
Additional MRI findings reported in intersection syndrome include tendon thickening and loss of the tendon’s comma shape to a more rounded configuration of the tendons [2]. We were unable to confidently distinguish these changes from the normal morphologic alterations in tendon shape at the point of crossover in our series.
In this report, we have described and illustrated MRI abnormalities that can be seen in intersection syndrome which have not yet been reported: tendinosis, muscle edema, and juxtacortical edema.
A recent study by de Lima et al. examined 11 fresh-frozen forearms of nine cadavers (mean age 84.2 years). They demonstrated that the area of intersection between the first and second DETC occurred between 3.5 and 4.8 cm (mean 4.18 cm) proximal to Lister’s tubercle [2]. Our study correlates to this study with the site of crossover measuring an average distance of 3.95 cm proximal to Lister’s tubercle.
The study by de Lima also performed tenography with direct injection of a gadolinium-containing contrast agent into the first and second DETC. The injections were performed under direct US visualization just distal to the musculotendinous junction. They found that in all 11 forearms, gadolinium-containing solution was identified extending through the tendon sheaths to the level of the extensor retinaculum. Our review shows that peritendinous edema or fluid in the first or second extensor compartments in patients with intersection syndrome is not necessarily limited to the site of crossover or limited by the extensor retinaculum but can even extend distally beyond the radiocarpal joint. The implication is that the tendon sheaths of the first and second extensor compartments are not bound by the extensor retinaculum. Although intersection syndrome is principally a peritendinous phenomenon, associated reactive tenosynovitis can occur over long distances and, in our study, measuring a distance of up to 12.2 cm (mean > 7.5 cm).
Although two of the six patients received IV gadolinium for their MRI examination, we do not feel that contrast-enhanced imaging is necessary or particularly helpful in the diagnosis of intersection syndrome. We believe that contrast should only be given in cases only where there is a high clinical suspicion for abscess or soft tissue neoplasm. In our study, areas of enhancement simply matched areas of edema or inflammation seen on the fluid-sensitive sequences. None showed mass-like enhancement.
With respect to MRI technique, fluid-sensitive sequences are the key to identifying the findings of intersection syndrome. We again emphasize the importance of increasing the longitudinal coverage to include the mid-forearm in anyone with clinical findings suggesting intersection syndrome. Most of the six patients imaged had skin markers placed at the site of clinical concern therefore ensuring that MRI would cover the appropriate area. However, our case in point is the second patient (who did not have a skin marker placed initially), in whom the initial standard wrist protocol MRI failed to cover the area of intersection. Only after additional imaging proximally was the diagnosis of intersection syndrome made.
There were a few limitations to this study. The prevalence of intersection syndrome in this study (0.47%) was determined by taking all the wrist and forearm MRIs performed over almost a 3-year period with MRI and clinical findings consistent with intersection syndrome. The true incidence and prevalence of intersection syndrome in the US is unknown. We realize that patients with a high clinical index of suspicion for intersection syndrome probably would not go on to get an MRI and therefore our overall incidence for the condition is likely underestimated.
Correlating the MRI imaging findings with the clinical findings made our diagnosis of intersection syndrome. There was a selection bias because only the radiology reports that contained the key words included in our selection criteria were chosen for our study. We understand that many additional cases of intersection syndrome could easily have bypassed our selection methodology.
In conclusion, intersection syndrome has characteristic findings on MRI. Our hope is to bring these new MRI findings associated with intersection syndrome to the forefront, so that radiologists are more aware of the condition and are less inclined to attribute abnormal findings to other differential possibilities. Finally, we recommend that a larger area of coverage be employed to at least the mid-forearm in cases where the clinical history suggests DETC abnormality, intersection syndrome, or when extensor changes are identified at the wrist without obvious etiology to ensure coverage of the site of intersection of the second and third DETC.
References
Idler RS, Strickland JW, Creighton JJ Jr. Intersection syndrome. Indiana Med 1990; 83: 658–659.
de Lima JE, Kim HJ, Albertotti F, Resnick D. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiol 2004; 33: 627–631.
Browne J, Helms CA. Intersection syndrome of the forearm. Arthritis Rheum 2006; 54: 2038.
Servi JT. Wrist pain from overuse: detecting and relieving intersection syndrome. Phys Sportmed 1997; 25: 41–44.
Palmer DH, Lane-Larsen CL. Helicopter skiing wrist injuries. A case report of “bugaboo forearm”. Am J Sports Med 1994; 22: 148–149.
Pantukosit S, Petchkrua W, Stiens SA. Intersection syndrome in Buriram Hospital: a 4-yr prospective study. Am J Phys Med Rehabil 2001; 80: 656–661.
Dobyns JH, Sim FH, Linscheid RL. Sports stress syndromes of the hand and wrist. Am J Sports Med 1978; 6: 236–254.
Hanlon DP, Luellen JR. Intersection syndrome: a case report and review of the literature. J Emerg Med 1999; 17: 969–971.
Costa CR, Morrison WB, Carrino JA. MRI features of intersection syndrome of the forearm. AJR Am J Roentgenol 2003; 181: 1245–1249.
Parellada AJ, Gopez AG, Morrison WB, Sweet S, Leinberry CF, Reiter SB, Kohn M. Distal intersection tenosynovitis of the wrist: a lesser-known extensor tendinopathy with characteristic MR imaging features. Skeletal Radiol 2007; 36: 203–208, Epub 2006 Dec 20.
Grundberg AB, Reagan DS. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg [Am] 1985; 10: 299–302.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, R.P., Hatem, S.F. & Recht, M.P. Extended MRI findings of intersection syndrome. Skeletal Radiol 38, 157–163 (2009). https://doi.org/10.1007/s00256-008-0587-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-008-0587-4