Abstract
Objective
To correlate the anatomic and MR imaging characteristics of the area of intersection of the first and the second dorsal extensor tendon compartments (DETC) in the distal forearm in an attempt to improve the design of MR imaging protocols used for the evaluation of intersection syndrome.
Design and patients
Ten forearms of nine cadavers underwent MR imaging in the axial and sagittal-oblique planes before and after tenography with direct injection of a gadolinium-containing contrast agent into the first DETC in four forearms, the second DETC in four forearms, and both compartments in the remaining two forearms. The area of intersection between the first and second DETC was identified in each case as well as its distance from Lister’s tubercle. Subsequently all forearms were sectioned in the axial (8 forearms) or sagittal-oblique planes (2 remaining forearms) to parallel the imaging planes. Detailed examination of each of the anatomic slices was performed in a search for anatomic variations and for possible anatomic connections of the tendons sheaths. One forearm was dissected to identify the area of intersection.
Results
The area of intersection between the first and second DETC occurred between 3.5 cm and 4.8 cm (mean 4.18 cm) proximal to Lister’s tubercle. After tenography, gadolinium solution was noted in the third DETC in two of four specimens in which the second DETC was injected and in one of two specimens in which both the first and second DETC were injected. Extension of the gadolinium solution between the first and second DETC was noted during isolated injections of either compartment, although this finding may have related to iatrogenic injection effects. The axial plane was the most valuable for assessment of the area of intersection of the first and second DETC.
Conclusion
MR imaging is a noninvasive method that can be used for the evaluation of distal forearm and wrist pain. Standard wrist protocols do not include the area of intersection between the first and second DETC and, in those cases in which intersection syndrome is suspected, the MR examination must be tailored to include the forearm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intersection syndrome is an uncommon overuse syndrome of the distal forearm. The area of intersection of the first and second dorsal compartments in the dorsoradial aspect of the distal forearm is the site of abnormality. The etiology of intersection syndrome is still under debate [1]. Standard wrist MR imaging protocols do not include the primary area of abnormality in this condition, which occurs several centimeters proximal to Lister’s tubercle (dorsal tubercle in the distal radius). Our study includes a review of the literature on the subject and detailed MR imaging of this area of the wrist, before and after tenography in cadavers, with correlation with anatomic specimens. As a result an improved MR protocol is suggested, tailored to the evaluation of this syndrome when it is clinically suspected.
Materials and methods
Eleven fresh-frozen forearms of nine cadavers were studied. The cadavers were derived from six men and five women, ages 66―97 years at the time of death (mean 84.2 years). Five were left forearms and six were right forearms.
One forearm was selected randomly for dissection. MR imaging of the other 10 forearms was performed with a 1.5 Tesla unit (GE Medical Systems, Milwaukee, Wis.). The 10 forearms were imaged with a 4.25 inch (11 cm) dedicated wrist solenoid coil, with the forearms being placed in the pronated position. Images were obtained using a special protocol that included modifications in imaging sequences, slice thickness and field of view (FOV) compared with our “standard” wrist protocol. Our standard wrist protocol includes axial images that extend an average of 2.8 cm proximal to Lister’s tubercle, sagittal images that extend an average of 4.9 cm proximal to Lister’s tubercle, and coronal images that extend an average of 5.3 cm proximal to Lister’s tubercle. The average extent of proximal imaging of the forearm used for the current investigation was 7.2 cm in the axial, sagittal, and coronal planes. Spin echo T1-weighted (TR 400/TE 22) images were performed in the axial plane, starting at the level of the radiocarpal joint and extending proximally 7―7.5 cm. Subsequently spin echo T1-weighted (TR 500/TE 15) sagittal-oblique images were obtained using a plane that was parallel to that of the dorsolateral surface of the distal radius (which extends from the dorsal tubercle (Lister’s tubercle) to the radial styloid process) and, consequently is parallel to the intersecting tendons in the dorsoradial aspect of the forearm; this results in an approximately 60° angle with respect to the plane of the table for right forearms and approximately 120° for left forearms. This oblique plane was programmed from the axial images (Fig. 1) and oriented parallel to the dorsolateral surface of the distal radius. An 8 cm FOV and a 512×256 acquisition matrix were utilized for both axial and sagittal T1-weighted sequences. The axial images were performed with a slice thickness of 2 mm and 0.5 mm of interslice gap, resulting in 25―30 images. The sagittal-oblique images were obtained with a slice thickness of 2.5 mm and an interslice gap of 0.5 mm, and were limited to the dorsolateral aspect of the forearm.
The 10 forearms previously imaged were then subject to tenography and underwent repeat MR imaging. Tenography was performed utilizing ultrasound (US) guidance with an ATL 5000 model unit (ATL Ultrasound, Bothell, Wash.) and a high-frequency (12 MHz) linear-array transducer. The tendons of the first or second dorsal compartments, or both, were identified and, under direct US visualization, a 22 gauge needle was inserted into the target compartment(s), just distal to the musculotendinous junction, and an injection of 3―8 cm3 of gadopentetate dimeglumine (Magnevist, Berlex Laboratories, N.J.) solution (2 cm3 Magnevist/250 cm3 0.9% NaCl solution) was conducted. Injections were performed into the first dorsal compartment only in four forearms and into the second dorsal compartment only in four other forearms; in the remaining two forearms, the injection was performed into both the first and second dorsal compartments. Following injection into the tendon sheaths, the 10 forearms were again imaged with MR imaging. Spin echo T1-weighted images without (TR 400/TE 22) and with (TR 500/TE 12) fat suppression were obtained and followed by spin echo T1-weighted sagittal-oblique images without and with fat saturation (TR 400/TE 22, TR 400/TE 12, respectively). The sagittal-oblique images were again performed with a slice thickness of 2.5 mm, while the axial images were performed with a 2 mm slice thickness. All post-tenography series utilized an 8 cm FOV, a 0.5 mm interslice gap, and a matrix of 512×256.
The same 10 forearm specimens were then frozen for more than 96 h at −60 °C and sectioned utilizing a band-saw. Eight of the specimens were sectioned in the axial plane, with a slice thickness of 3 mm. The two remaining forearm specimens were sectioned in the sagittal-oblique plane using a 3 mm slice thickness and the same special oblique plane that was used for MR imaging. The intent was for the anatomic sections to correspond closely with the MR images with respect to orientation and thickness. Each of the slices was then photographed. Detailed examination of each of the anatomic slices was performed and compared with the corresponding MR images.
Axial and sagittal-oblique selected sections of two of the specimen forearms were radiographed with a high-contrast, high-resolution X-ray system (Faxitron; Hewlett-Packard, McMinnville, Ore.).
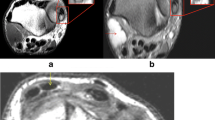
One forearm (not imaged or sectioned) was dissected to specifically demonstrate the area of intersection between the first and second dorsal compartments (Fig. 2).
Dissection of a forearm demonstrates the area of intersection and the relationships between the tendons of extensor carpi radialis longus and brevis muscles, the second dorsal extensor compartment (arrowhead) underneath the musculotendinous junction of the abductor pollicis longus and extensor pollicis brevis, the components of the first dorsal compartment (arrow)
Results
MR images and anatomic sections demonstrated that the area of intersection between the first and second dorsal extensor compartments occurred between 3.5 cm and 4.8 cm (mean 4.18 cm) proximal to Lister’s tubercle.
The axial plane demonstrated the highest degree of anatomic definition in the area of interest and was, in our observations, the most valuable in the assessment of this area of intersection. The sagittal-oblique plane imaging of the region of intersection was less useful than the axial images, as the plane of orientation in that sequence parallels the orientation of the tendons, resulting in a limited number of images of that area and, consequently, less anatomic detail. We believe that this observation can be extrapolated to the coronal plane of imaging.
Post-tenography MR examination of the forearms demonstrated the presence of gadolinium-containing solution within the third dorsal extensor compartment in two of the four forearm specimens in which the second dorsal extensor compartment was injected. Gadolinium-containing solution was present in the third dorsal extensor compartment in one of the two forearm specimens in which both the first and the second dorsal extensor compartments were injected. Extension of contrast material into the third dorsal compartment was not observed after any of the four injections into the first dorsal compartment. These findings are compatible with previously reported observations in the literature that a communication may normally exist between the second, third and fourth dorsal extensor tendon compartments, but these central compartments do not communicate with the first or fifth dorsal extensor tendon compartments. In all specimens gadolinium-containing solution was identified extending through the tendon sheaths to the level of the extensor retinaculum. In a limited number of clinical cases described in the literature tenosynovitis was not present at the level of the extensor retinaculum [9].
Discussion
Intersection syndrome is one of the inflammatory disorders involving the tendons and the soft tissues of the distal forearm and wrist. It was first described in 1841 by Velpeau [1]. It has been encountered in those whose activities involve repetitive wrist flexion and extension, including secretaries, carpenters, and maintenance and filing workers, as well as rice-harvesting workers in Thailand [2, 3]; athletes involved in weightlifting, rowing or canoeing are also affected. It can also be seen with the onset of a new physical activity involving a different pattern of wrist motion [5]. Many terms have been applied to describe this same condition, including peritendinitis crepitans, bugaboo forearm, crossover syndrome, adventitial bursitis, subcutaneous perimyositis, oarsman’s wrist, and abductor pollicis longus syndrome.
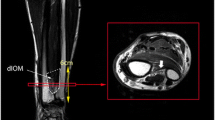
The site of inflammatory changes in this condition is a region located 4―8 cm proximal to Lister’s tubercle where the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) tendons, the components of the second dorsal extensor tendon compartment of the wrist, cross beneath the musculotendinous junction of the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons, the components of the first dorsal extensor tendon compartment [1, 2, 3, 4] (Fig. 3).
Corresponding sequential axial (A1, A2, A3, A4, A5, A6) high-resolution radiographs and gross photographs of the distal forearm from proximal to distal. Images demonstrate the area of intersection between the musculotendinous junction of the first dorsal compartment (arrows) and the tendons of the second dorsal compartment underneath (arrowheads), and the relationships of these tendons and their compartments in the distal aspect of the forearm
The pathophysiology of this disorder remains unknown [1, 2, 5], and has been the source of significant debate [6]. Two theories have been proposed, neither of which is accepted unanimously. Friction between the muscle bellies of the APL and EPB with the tendon sheath containing the ECRL and ECRB tendons was believed to be the cause of the intersection syndrome until the mid-1980s. In 1985 Grundberg and Reagan [4] suggested that the actual cause and site of pathology were stenosis confined to the second dorsal compartment, related to tenosynovitis, and that adjacent swelling occurs subsequently. Idler et al., in1990, furthered the controversy by affirming that in this region these structures are closely approximated by the extensor fascia of the forearm and that the tendons are lined only with peritenon, without tenosynovium [5]. Regardless of the etiology the symptoms include pain, edema, redness, tenderness to palpation, and crackling or crepitance with flexion and extension of the wrist.
The differential diagnosis includes tenosynovitis of the dorsal extensor tendons involving the first compartment (de Quervain’s tenosynovitis), which generally occurs several centimeters distal to the area of pathology encountered in intersection syndrome. It also includes local trauma and entrapment of the superficial radial nerve as it emerges from beneath the brachioradialis tendon (Wartenberg’s syndrome), tenosynovitis of the second and third dorsal compartments of the wrist, as well as wrist ligament sprain, ganglion cyst, and muscle strain [8].
MR imaging findings in intersection syndrome include tendon thickening and loss of the tendon’s comma shape to a more rounded configuration of the tendons, and peritendinous edema and fluid within the tendons sheaths of the first and second dorsal extensor tendon compartments surrounding the area of intersection, suggesting tenosynovitis. After the administration of intravenous gadolinium solution, peritendinous enhancement has been described [9].
In those cases in which intersection syndrome is suspected, the imaging protocol must be tailored to include the forearm, the site of pathology in this condition, as distal tenosynovitis at the level of the extensor retinaculum may not be present in this entity [9]. In order to include the area of intersection between the first and second dorsal compartment tendons, more proximal images must be obtained compared with those obtained in a typical wrist examination. Axial scans are critical for this diagnosis (Fig. 4A). Tailored thin sagittal-oblique images obtained in our study seemed to provide more detailed information of the area of intersection than the sagittal images performed in our standard protocol studies (Fig. 4B, C), although their inclusion as a part of the standard protocol of the forearm has not been investigated.
T1-weighted (TR500/TE12) fat-saturated MR tenography images in the axial (A) and sagittal-oblique (TR400/TE12) (B, C) planes were obtained from a cadaver specimen after injection of a gadolinium solution into the first (arrows) and second (arrowheads) dorsal compartments at the level of the wrist. Sagittal-oblique thin-section imaging provides very good depiction of the structures in the area of intersection of the first and second dorsal extensor compartments
As with other overuse syndromes, intersection syndrome will respond to cessation of provocative activities in the great majority of cases [1, 2, 5]. Modification of work activities, nonsteroidal anti-inflammatory drugs, and immobilization of the wrist with a splint in slight extension are used initially [1, 2, 3, 4, 5]. In cases of failure of conservative treatment after 2 or 3 weeks, anesthetic and steroid therapy or long-acting steroid therapy alone can be used, with injection at the site of maximum swelling [1] or in the second dorsal compartment [4]. Surgery is indicated to decompress the area of intersection in those patients whose findings are refractory to these conservative measures.
Conclusion
MR imaging is a noninvasive method for the evaluation of distal forearm and wrist pain. Intersection syndrome is an underdiagnosed condition, especially when considering MR imaging, probably related to standard wrist protocols which do not include that area, low awareness of this entity and because, in the majority of cases, early relief of symptoms occurs when conservative measures are used. When patients are referred for MR imaging, the diagnosis may not be considered if a standard wrist protocol is used. We recommend that, in those patients in whom the clinical history suggests this entity, a larger portion of the forearm must be assessed. Finally, our impression is that thin sagittal-oblique MR images provide better detail of the first and second dorsal extensor compartments compared with standard sagittal images.
References
Hanlon DP, Luellen JR. Intersection syndrome: a case report and review of the literature. J Emerg Med 1999; 17:969–971.
Pantukosit S, Petchkrua W, Stiens SA. Intersection syndrome in Buriram Hospital: a 4-year prospective study. Am J Phys Med Rehabil 2001; 80:656–661.
Palmer DH, Lane-Larsen CL. Helicopter skiing injuries: a case report of “bugaboo forearm”. Am J Sports Med 1994; 22:148–149.
Grundberg AB, Reagan DS. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg 1985; 10:299–302.
Idler RS, Strickland JW, Creighton Jr JJ. Intersection syndrome. Indiana Med 1990; 83:658–659.
Allison DM. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg 1986; 11:913–914.
Gonzalez MH, Sohlberg R, Brown A, Weinzweig N. The first dorsal extensor compartment: an anatomic study. J Hand Surg [Am] 1995; 20:657–660.
Leslie BM, Ericson Jr WB, Morehead JR. Incidence of a septum within the first dorsal compartment of the wrist. J Hand Surg [Am] 1990; 15:88–91.
Timins ME, O’Connell SE, Erickson SJ, Oneson SR. MR imaging of the wrist: normal findings that may simulate disease. Radiographics 1996; 16:987-995.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Lima, J.E., Kim, HJ., Albertotti, F. et al. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiol 33, 627–631 (2004). https://doi.org/10.1007/s00256-004-0832-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-004-0832-4