Abstract
Objective
The aim of the study was to evaluate long-term damage in the internal structures of the knee joints of recreational long-distance runners.
Materials and methods
Ten years after their participation in a baseline study concerning their knee joints, seven long-distance runners and one who had given up long-distance running were invited to participate in a repeat magnetic resonance imaging (MRI) investigation. The same evaluation criteria and the same technical equipment were used, and the results of the two investigations were compared.
Result
No adverse long-term consequences were observed in six of the seven active runners, regardless of pre-existing damage at the baseline investigation. In one case the arthrotic changes were progressive in nature. The person who had given up running presented with severe deterioration of the internal structures of the knee joint.
Conclusion
Non-physiological maximal loads secondary to the marathon race do not cause any permanent damage in the internal structures of the knee joint in individuals without significant pre-existing damage. A disposition for premature arthrosis was not registered in the population investigated. A protective value of long distance running on the internal structures of the knee joint is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-distance running is an increasingly popular sport. Little is known about its long-term sequelae on the joints of marathon runners. Schmitt et al. showed that competitive marathon runners experienced no serious damage to the knee joint. Indeed, the authors postulated a certain protective effect on the hip joint [1]. Several studies [2–4] have shown that marathon races cause no major short-term or medium-term damage, provided that there was no evidence of pre-existing damage. Immediate relevant damage to internal structures has not been reported in any peer-reviewed literature. Using high-field magnetic resonance imaging (MRI) scanners for investigation, recent studies conducted by Hohmann et al. [2] and Schueller-Weidekamm et al. [3] have largely confirmed the previous conclusions drawn by Krampla et al. [4] that long-distance running causes neither edema in the medullar cavity nor joint effusion. In general, Caselli and Longobardi [5] observed mild transient discomfort, such as foot blisters or muscle cramps. They also reported that such phenomena were experienced more commonly in poorly trained runners. These studies also revealed no new defects in cartilage or the meniscus. In our study the knee joints of leisure-time runners were re-investigated 10 years after initial investigations, using the same MRI protocol. Such a long-term follow-up has not been undertaken previously. Eight of the ten individuals who had participated in the initial MRI examination in the study conducted in 1997 [4] participated in our investigation. Seven had remained active runners and had taken part in all the examinations in the first study. Current MRI investigations were compared with baseline investigations.
Materials and method
Only those who had participated in the previous study (study 1) in 1997 [4] could be included in this investigation (study 2). In study 1 ten participants in the Vienna city marathon were investigated initially. The only criterion they had to fulfill was that they considered themselves to be sufficiently fit to complete the run. In study 1 they had been examined three times: prior to the race, within 24 h of running, and approximately 6 weeks later. One participant ended up not participating in the marathon after having undergone the initial MRI scan and gave up long-distance running following a partial tear of the patellar tendon. This person was excluded from study 1 but re-examined in study 2 and is mentioned as “runner” no.8, although he cannot be considered as a long-distance runner. One person did not attend for MRI scans numbers 2 and 3 after the race in 1997 and also had to be excluded from study 1. (According to the official results of the run, he finished the marathon in 3 h 17 min. This person refused to participate in the recent study and gave no clinical information about his health.) This left eight participants in the initial trial, of whom seven fulfilled the inclusion criteria for study 2 and were prepared to participate in it. Person number 8 (see above) also participated in study 2. We could not contact the last person.
Informed consent was obtained from the seven study 1 participants who were eligible for inclusion in study 2. The age range of the probands at the 10-year follow-up examination was 37 years to 55 years [mean 50 years, standard deviation (SD) 7.1 years). All participants were male and had been pursuing long-distance running for 15 to 30 (mean 20, SD 4,8) years. Since the last study, the runners had covered a distance of 4,000 to 25,000 (mean 14,500, SD 6,872) km. All participants were trained leisure-time runners. The sports activities undertaken by the participants are summarized in Table 1.
The same knee joint investigated in study 1 was examined in study 2 (in study 1 the participants had been permitted to select one side). At both time points, measurements were performed with the same 1.0 T Siemens Impact MRI unit with the identical parameters, so that optimal comparability would be achieved. The scanner had remained unchanged since study 1.
Using a flex-surface coil, the following sequences were obtained:
-
1.
Sagittal proton-density-weighted fast spin-echo dataset [time to repeat (TR) 1,200 ms, time to echo (TE) 12 ms; slice thickness 3.0 mm; matrix 378 pixels × 256 pixels),
-
2.
Sagittal gradient-echo dataset: double-echo steady state three-dimensional (DESS 3D) (TR 26.8 ms, TE 9 ms; flip angle 40°; slice thickness 2.8 mm; matrix 197 pixels × 256 pixels)
-
3.
Coronal fat-suppressed inversion recovery sequence: fast-STIR (TR 5,100 ms, TE 30 ms, TI 150 ms, slice thickness 4.0 mm, matrix 210 pixels × 256 pixels).
Assessment of the knee was the same in study 1 and study 2.
The following were assessed:
Menisci
Grading of lesions: grade I, non-linear signal alteration on proton-density-weighted images; grade II, linear signal on proton-density-weighted images within the meniscus but not reaching the surface; grade III, linear signal alterations reaching the meniscal surface; grade IIIA reaching one surface, and IIIB reaching the upper and lower surface of the meniscus (representing a meniscal tear reaching one or two surfaces).
Cartilage
Grading of lesions: grade I, increased signal, smooth surface; grade II, irregular surface but lesion not reaching the bone; grade III, ulceration reaching the bone; grade IV, wide denudation of the bone.
Bone marrow
The presence of bone marrow edema was defined as an area of high signal intensity on T2-weighted images, especially the turbo-inversion recovery magnitude (TIRM) sequence, and low signal intensity on proton-density-weighted images. Where present, it was classified as diffuse or localized signal changes. Localized bone marrow edema was correlated with meniscal and cartilaginous signal alterations.
Joint fluid
Normal or increased (consensus of interpreting radiologists).
Patellar tendon
Signal alterations and thickening.
Cruciate ligaments
Signal alterations, integrity and thickening.
Medial and lateral collateral complexes
Signal alterations, integrity and thickening.
The assessment in study 2 was first made by two radiologists, independently, who then reached a consensus. The reading of the studies was first carried out without knowledge of the previous examination. The readers were aware of the date of the study. After having read the initial MRI scans prior to the marathon in 1997 and the recent MRI scans of study 2, the readers compared the images of study 1 and 2, and potential changes were registered. The consensus decisions are mentioned in Table 2, whereas Table 3 shows the individual ratings prior to the consensus. One reader (R1 in Table 2) was a senior staff radiologist with 16 years of experience in musculoskeletal MRI. This reader also did the interpretation in study 1. The second reader in study 1 was no longer a member of staff and had been replaced by reader R2 (in Tables 2 and 3). He was a junior staff radiologist who has been doing skeletal MRI for 8 years. Both ratings were weighted equally.
Reader R2 also rated the baseline study. Reader R1 also re-read the studies from 1997 in order to rule out an influence of the additional 10 years of experience. Both readers evaluated independently the changes between the baseline examination and the 10-year follow-up examination. These changes are listed in Table 2.
The ratings were discussed in a separate session until a consensus was found (Table 2). The evaluation was performed on a state-of-the-art Sienet Magicview 1000 workstation on high-resolution black-and-white thin film transistor (TFT) flat screen monitors.
Results
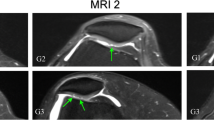
Study 1 and study 2 results registered at the menisci and the joint cartilage are summarized in Table 2. One grade II cartilage lesion had deteriorated to grade III. This runner had already had severe damage at study 1 (Fig. 1) in terms of a medial meniscal tear grade IIIB and a subtotally resected lateral meniscus. This person had developed a subchondral cyst between the run and the 6-week follow-up examination in 1997. Subject 6 showed a subtle deterioration of the cartilage in the lateral compartment: at study 1 the surface was considered as smooth with slightly patchy signal intensity (grade I degeneration). At study 2 the surface appeared slightly irregular and was therefore graded as a grade II lesion. Indeed, in this subject, a linear signal alteration within the lateral meniscus gave way to a mild non-linear signal alteration and the lesion was therefore downgraded from II to I between study 1 and study 2. Again, changes between study 1 and study 2 were subtle. Most other pre-existing lesions remained unchanged. Figure 2 shows the medial meniscus of runner 2 at study 1 and 10 years later (study 2). Figure 3 shows the medial meniscus of runner 3 at study 1 and study 2.
Subject number 8 had given up long-distance running 10 years before. After the baseline examination in 1997 he was advised not to take part in a marathon for medical reasons. This person showed severe changes between the first and final MRI scan. Grade II lesions of the retropatellar (Fig. 4) and lateral femoral cartilage (Fig. 5) turned into third-degree defects. He also presented at study 2 with a circumscribed area of high signal intensity on the STIR sequence in the medial femoral condyle, which was interpreted as bone marrow edema (Fig. 6). He did not recall a trauma prior to the MRI scan and reported intermittent minor discomfort in the knee in changing locations. No other new areas of high signal intensity were discovered in the other participants. The state of the medial meniscus had also deteriorated from normal to a degree I signal alteration.
Sagittal gradient-echo dataset: DESS 3D (TR 26.8 ms, TE 9 ms; flip angle 40°; slice thickness 2.8 mm; matrix 197 pixels × 256 pixels). a Irregular surface of the retropatellar cartilage, grade II. High signal intensity and thickening of the proximal patellar tendon are exhibited. b Ten years later, grade III defect of the retropatellar tendon; signal alterations of the tendon are unchanged
In one case the baseline investigation had already shown minimal signal alterations of the posterior cruciate ligament. The anterior cruciate ligaments were all normal. The collateral ligaments were also intact. At study 2 no changes were registered in any of these structures. No joint effusion was observed in any of the participants.
Discussion
Excluding the single case of significant pre-existing damage at the menisci and the joint cartilage (runner 1 in Table 1), and taking only the remaining probands into account, we found no major new internal damage in the knee joints of marathon runners after a 10-year interval between observations. In contrast, the only person who had given up long-distance running showed severe deterioration in the intra-articular structures of his knee. The frequency of meniscus lesions in long-distance runners, reported previously, ranged widely [1–4, 6, 7]. This diversity may be attributable to the different evaluation criteria used. Shellock et al. [6] addressed this phenomenon in one study and concluded that meniscal lesions did not occur more frequently in long-distance runners than they did in the general population. Based on the strict evaluation criteria in this study, the frequency of internal degeneration at the menisci was as high in study 2 as it was in study 1. All baseline and control investigations were assessed by the same team of radiologists, and only those changes that had occurred between study 1 and study 2 were taken into account for the assessment. This minimized the effect of possible inter-observer variance on the outcome of this study regarding progression of intra-articular lesions. As inter-observer variance seems to play an important role with regard to the frequency of reported lesions, comparison of our study with previous studies by other authors has to be treated with caution. In this study inter-observer variance played a role regarding the rating of cartilage lesions. As the cartilage of the medial and lateral compartment was assessed separately, each observer had to rate 16 cartilages. In four cases the rating differed by one degree. In one case the rating for the lateral meniscus was different according to the two readers. The limited spatial resolution of a 256 pixel matrix on a 1.0 T MRI scanner made the rating of chondral signal intensity and surface changes difficult. This was a limitation of the equipment and decreased diagnostic accuracy. As a result, inter-observer variance was much higher for cartilage lesions than all other structures. Reader 1 re-read the studies of the initial trial after 10 years. His ratings in 2007 were identical to the ones from 1997. Intra-observer variance did not play a role in this case.
The hypothesis that there will be no damage in well-trained and healthy persons has been confirmed. It seems that continuous exercise is protective rather than destructive. The probands were all well-trained runners who used appropriate equipment (e.g., suitable shoes) and followed sports medicine guidelines during training and competitions. The influence of this factor cannot be assessed, because no other comparable group was investigated. Hohmann et al. were of the same opinion [8]. Their study group also registered no damage due to long-distance running. According to Satterthwaite et al. [9], only healthy individuals should expose themselves to such strain.
Runner no. 2 was highly remarkable, as he presented with a grade IIIA meniscal tear at study 1. This lesion was an incidental finding. He recalled no event of an injury prior to the examination and reported no clinical symptoms. This person was the most active of all participants and performed long-distance running at a very high level. (His typical pace would have been sufficient to win the marathon in the Olympic games in Athens in 1896. At that time the length of a marathon was not clearly defined. The distance was considerably shorter than it is today.) Meniscal tears are associated highly with local degeneration of the cartilage [10]. In the case of subject 2 there were no changes in signal intensity or deterioration to the surface of the cartilage. The tear itself remained unchanged, as did the cartilage. At the time of writing, this runner still has no knee pain and reports no other symptoms regarding the knee. Cymet and Sinkov [7] reported a possible increase in radiographic evidence of osteoarthritis in endurance sports athletes, but no related increase in symptoms were reported. The severe lesion of the meniscus has not lead to a chondropathy that could be visualized by MRI or any other signs of osteoarthritis. Up to a point, this contradicts the conclusion made in our former study [4]. Pre-existing high-degree meniscal or chondral lesions do not necessarily deteriorate through sports. Runner no. 1, on the other hand, showed increased signs of osteoarthritis. One case of degeneration and one case of no change over a period of 10 years do not allow any final conclusions to be drawn. However, it can be stated that both options occur.
Runner number 5 presented with unchanged grade II degeneration of the medial and lateral meniscus. No other changes were observed. This person reported minor knee pain when he had not been running for more than 2 weeks. Running was an effective “therapy” in this case. No obvious explanation for this can be given.
Subject number 8 originally planned to participate in the Vienna city marathon in 1997. As he finally did not take part in the run and gave up running completely, he did not fulfill the inclusion criteria for study 1 (where he was not mentioned in the results) or study 2, but his case is still highly interesting. Together with runner no.1 this person showed the greatest deterioration regarding the state of the intra-articular structures of the joint.
The findings from one person, of course, do not allow a general statement to be made, but it might be taken as a hint that long-distance running might even have a protective value.
Several limitations were encountered when we were trying to investigate runner number 1, who had progressive signs of arthrosis after meniscal rupture and partial resection of the meniscus. First of all, this sportsman had had a semi-professional career as a football player prior to becoming a long-distance runner. Football is generally regarded as a sport that is not gentle to the knee. According to Larsen et al. [11], knee-injuries in elite football players seem to have a serious long-term outcome, but also uninjured players have a higher risk of developing arthritis than the general population. Whether the progression of arthrosis was accelerated by the strain of running cannot be stated with certainty. The relatively moderate progression in the observation period may well have been due to the 10 years that had elapsed in the intervening period.
A general measure of the deterioration of arthrosis over time does not exist. Moreover, this runner had no clinical symptoms that rendered running impossible or impaired his enjoyment of the sport.
The lack of a control population is a limitation of the study. An age-matched control group of individuals that did not play sport would require a much bigger study. On the other hand, the lack of progression, or only moderate progression, of intra-articular lesions suggests that such a matched group is of minor importance. If such a group had also shown no or little progression, this would add weight to the hypothesis that long-distance running is not harmful to the knee-joint. Conversely, a more rapid progression in non-sports individuals would suggest a protective effect of long-distance running.
As few changes were observed, there were no obvious effects of other activities on the participants’ knees.
The major limitation of the study was the small sample size. According to the inclusion criteria, the maximum number of participants was limited to the nine athletes who had participated in study 1. The ninth person from the initial study could not be traced. Runner number 10, who did not participate in the follow-up studies after the run, refused to give any clinical information about his knee. As there were no other runners who were examined under the same conditions, there was no way in which we could increase the number of participants in order to make statistical analysis possible.
Despite the lack of statistical evidence in this study regarding the impact of long-distance running, these results suggest that, if runners have appropriate training and footwear, damage to their knee as a consequence of marathon running is unlikely. This conclusion is in line with findings in the existing literature. Although there are still insufficient data to provide definitive recommendations to long-distance runners, it seems that in healthy people long-distance running does not increase the risk of osteoarthritis of the knees and does not accelerate “aging” of the knee.
References
Schmitt H, Rohs C, Schneider S, Clarius M. Is competitive running associated with osteoarthritis of the hip or the knee? (in German) Orthopade 2006; 35: 1087–1092.
Hohmann E, Wortler K, Imhoff A. Osteoarthritis from long-distance running? (in German) Sportverletz Sportschaden 2005; 19: 89–93.
Schueller-Weidekamm C, Schueller G, Uffmann M, Bader TR. Does marathon running cause acute lesions of the knee? Evaluation with magnetic resonance imaging. Eur Radiol 2006; 16: 2179–2185.
Krampla W, Mayrhofer R, Malcher J, Kristen KH, Urban M, Hruby W. MR imaging of the knee in marathon runners before and after competition. Skeletal Radiol 2001; 30: 72–76.
Caselli MA, Longobardi SJ. Lower extremity injuries at the New York City Marathon. J Am Podiatr Med Assoc 1997; 87: 34–37.
Shellock FG, Deutsch AL, Mink JH, Kerr R. Do asymptomatic marathon runners have an increased prevalence of meniscal abnormalities? An MR study of the knee in 23 volunteers. AJR Am J Roentgenol 1991; 157: 1239–1241.
Cymet TC, Sinkov V. Does long-distance running cause osteoarthritis? (review) J Am Osteopath Assoc 2006; 106: 342–345.
Hohmann E, Wortler K, Imhoff AB. MR imaging of the hip and knee before and after marathon running. Am J Sports Med 2004; 32: 55–59.
Satterthwaite P, Norton R, Larmer P, Robinson E. Risk factors for injuries and other health problems sustained in a marathon. Br J Sports Med 1999; 33: 22–26.
Christoforakis J, Pradhan R, Sanchez-Ballester J, Hunt N, Strachan RK. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy 2005; 21: 1366–1369.
Larsen E, Jensen PK, Jensen PR. Long Term outcome of knee and ankle injuries in elite football. Scand J Med Sci Sports 1999; 9: 285–289.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krampla, W.W., Newrkla, S.P., Kroener, A.H. et al. Changes on magnetic resonance tomography in the knee joints of marathon runners: a 10-year longitudinal study. Skeletal Radiol 37, 619–626 (2008). https://doi.org/10.1007/s00256-008-0485-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-008-0485-9