Abstract
Purpose
The purpose of this study was to evaluate the pattern of tumour spread across the SI articulation, correlating with cadaveric anatomic observations, in order to better understand the local spread of tumour and to assist in the assessment of local staging.
Material and methods
Twenty-four consecutive patients (14 male, 10 female; age range 22–89 years, mean 52 years) with primary bone tumours of the iliac bone or sacrum abutting the SI joint, in whom surgical resection of the SI joint was performed, were studied following institutional ethics approval. In all patients, preoperative magnetic resonance (MR) imaging studies of the pelvis and SI joint were reviewed for imaging evidence of transarticular extension across the SI joint. Gross pathologic and histologic assessment of possible transarticular SI joint tumour extension was performed in all patients. Nine cadaveric pelvic specimens without pelvic neoplastic disease (4 male, 5 female; age range 20–84 years, mean 59 years, median 58 years) were anatomically dissected and the articular anatomy of the SI joint examined macroscopically.
Results
Twelve of the twenty-four patients demonstrated imaging and histological evidence of transarticular SI joint invasion. Eight tumours infiltrated only the interosseous ligamentous aspect of the SI joint. In the remaining four cases, extensive tumour infiltrated both the cartilaginous and ligamentous aspects of the joint. No case showed tumour involvement isolated to the cartilaginous aspect of the joint. Among the cadaveric specimens studied, degenerative changes were found involving the majority of cases (6/9), with cartilage thinning and fibrillation and antero-superior marginal osteophytes seen involving the cartilaginous portion of the SI joint articulation. Four of the nine specimens demonstrated central ossification bridging the iliac and sacral aspects of the ligamentous (interosseous) SI joint.
Conclusion
Tumour invasion across the SI articulation favours its interosseous ligamentous portion. Factors influencing transarticular tumour extension and its preferential course across the interosseous component of the articulation have been discussed. It is particularly important to assess the interosseous ligamentous portion of the SI articulation when locally staging primary pelvic bone tumours subjacent to the SI articulation, as this will have a significant impact on planning surgical management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The sacroiliac (SI) articulation is the most common joint invaded by tumour followed by the intervertebral disc spaces and facet joints [1]. There has been little information on the pattern of transarticular tumour infiltration. The SI articulation consists of two components; the cartilaginous component and the ligamentous component. The cartilaginous component, known at the auricular component [2] due to its shape (Fig. 1), is an atypical synovial joint. The sacral side is covered by hyaline cartilage up to 3 mm in thickness, and the iliac side is covered by a thin 1-mm layer of fibrous (fibrocartilage) cartilage [3]. The ligamentous component of the articulation is composed of corresponding eminences and depressions [3] which interdigitate, markedly restricting its motion and contributing to the strength of the articulation. The interosseous SI ligamentous tissue [4–6], which by definition forms a syndesmosis consisting of numerous short and very resistant bands, is firmly and directly attached to the opposing osseous surfaces [7] (Fig. 2).
Schematic illustration of the opposing aspects of the disarticulated SI joint. The auricular (cartilaginous) (C) and interosseous (I) aspects of the joint are shown with the ilium on the left and sacrum on the right. Reproduced from Grant's Atlas of Anatomy with permission from Agur and Dalley (2005) (Fig. 4.18A) [8]
Schematic illustration of cross section through the pelvis at the level of the SI articulations demonstrating the cartilaginous (arrows) and interosseous (asterisks) portions. The anterior (A) and posterior (P) interosseous ligaments, coccyx (X) and sacrospinous ligaments (C) are shown. Reproduced from Grant's Atlas of Anatomy with permission from Agur and Dalley (2005) (Fig. 4.18B) [8]
The following investigation describes the imaging features of the pattern of transarticular SI joint invasion seen in a series of cases of primary tumours of the iliac bone and sacrum. Correlation is made with anatomic observations of the SI joint in cadaveric specimens, and factors potentially influencing transarticular tumour invasion are discussed.
The extent of surgical resection is altered by transarticular SI tumour involvement. Standard or modified internal or external hemipelvectomy are widely-used and well-established procedures for innominate bone tumours. Tumour involvement of the SI articulation necessitates an extended internal or external hemipelvectomy, which are much more demanding procedures because of the complex anatomy and close relationship to important neural structures. Similarly, a sacrectomy may be extended to include resection of the SI articulation. Assessment of transarticular tumour invasion across the SI articulation is therefore of critical importance in tumour staging, having a direct impact on the extent of surgical resection.
The purpose of this study was to evaluate the pattern of tumour spread across the SI articulation, correlating with cadaveric anatomic observations, in order to better understand the local spread of tumour and to assist in the assessment of local staging.
Materials and methods
Twenty-four consecutive cases of primary pelvic bone tumours of iliac origin abutting the SI joint, treated from May 1997 to November 2002, in whom the SI joint was resected at the time of surgery, were studied following institutional ethics approval. There were fourteen male and ten female patients ranging in age from 22 to 89 years, with a mean age of 51.9 years and median age of 53 years. All the patients underwent preoperative cross-sectional imaging of the pelvis and SI joint with magnetic resonance imaging (MRI) prior to surgical tumoural resection and histological examination. Imaging was performed with a 1.5 Tesla MR imaging system (Signa; General Electric Medical Systems, Milwaukee, WI, USA). A torso coil was employed with a field of view of 36×36 cm and a matrix size of 256×192. Imaging sequences obtained in all patients included axial and coronal oblique spin-echo T1- (repetition time msec/echo time msec, 400–600/8–16) and fast spin-echo fat-saturated T2-weighted sequences (3,550–5000/85–105; echo train length eight). The coronal oblique images were obtained parallel to the long axis of the sacrum. All the imaging sequences used a slice thickness of 4 mm and a 0-mm gap. Intravenous contrast was not given in any of the studies assessed.
All images were evaluated retrospectively and by consensus of two readers who were blinded to clinical and histopathologic findings and who reviewed the images together. Images were assessed for evidence of tumour extension across the SI articulation. The SI articulation was defined to include both the anterior–inferior cartilaginous auricular component and the posterior interosseous ligamentous aspects of the articulation (Fig. 1). Transarticular invasion of the articulation was defined as direct contiguous tumour involvement, manifest by low T1 and intermediate or high T2 signal abnormality, of opposing bones involving either component of the articulation [1, 9]. For each case with imaging evidence of transarticular extension, the site(s) of tumour involvement of the SI articulation (cartilaginous and/or ligamentous) was documented. Histologic correlation of each case was made with documentation of tumour type, grade and histologic evidence of transarticular SI tumour extension made.
Nine cadaveric pelvic specimens with ages ranging from 20 to 84 years and with a mean age of 59 years (4 male, 5 female) were examined. The majority (8/9) were taken from cadavers of individuals over 55 years of age (3 male, 5 female). Two of the cadaveric specimens were fresh (unfixed) and the remaining seven were formalin-embalmed.
Five of the specimens were sectioned in an axial plane with cranial to caudal axial sections obtained through the entire SI articulation with a band saw at a slice thickness of approximately 1 cm. The remaining four specimens were dissected by removing the soft tissues covering the SI articulation, allowing examination of the external aspect of the joint. Each articulation was then carefully opened using a fine chisel and scalpel to reveal both the sacral and iliac surfaces of the auricular and interosseous portions.
Results
Clinical
On MR imaging assessment, transarticular tumour infiltration was demonstrated in 12 of the 24 patients studied (Table 1). Of the 12 cases with evidence of transarticular spread (age range 22–89 years, mean age 48 years, median age 44 years) there were 3 chondrosarcomas, 3 giant cell tumours, 1 malignant fibrous histiocytoma, 2 osteosarcomas, 2 Ewing's sarcomas and 1 unspecified sarcoma. Three of these tumours arose from the sacrum (1 chondrosarcoma, 1 osteosarcoma, 1 giant cell tumour). The 12 cases without evidence of transarticular spread (age range 24–80 years, mean age 56 years, median age 58 years) were 7 chondrosarcomas, 2 osteosarcomas, 1 leiomyosarcoma, 1 chordoma and 1 plasmacytoma. Two of these tumours arose from the sacrum (1 osteosarcoma, 1 chordoma). All 12 cases that demonstrated imaging evidence of transarticular extension also had histological confirmation of transarticular spread. Of the 12 cases without MR imaging evidence of transarticular spread, none illustrated histologic evidence of transarticular extension.
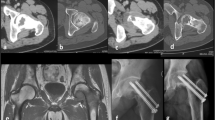
Eight of the 12 tumours with imaging and histologic evidence of transarticular spread illustrated tumour extension only across the posterior interosseous ligamentous portion of the SI articulation (Fig. 3). In the remaining 4 cases (4/12), the extent of disease involvement was considerable, with tumour seen extending across both the anterior (auricular) cartilaginous and posterior interosseous ligamentous portions of the SI articulation (Fig. 4). In no case was tumour spread demonstrated only across the anterior cartilaginous portion of the articulation.
Two axial T2-weighted fat-saturated images through the right SI joint in a 53-year-old female patient showing a giant cell tumour within the posterior aspect of the right ilium. The more cranial section (a) and more caudal section (b) through the SI articulation show an intact cartilaginous portion (asterisks) and tumour involving the interosseous portion of the joint. The extent of the tumour is delineated by arrows. Sacrum (S), ilium (I) and tumour (T)
Axial T1-weighted (a), axial T2-weighted fat-saturated (b), coronal oblique T1-weighted (c) and coronal oblique T2-weighted fat-saturated (d) images through the SI articulations in a 66-year-old female patient with an osteosarcoma arising within the left sacral ala. The tumour (T) extends across the left SI joint and involves both the cartilaginous (asterisks) and ligamentous (dotted) portions of the articulation, which are labelled on the right for comparison. Sacrum (S), ilium (I)
Anatomical
Antero-superior marginal osteophyte formation was present in six of the nine cadaveric specimens examined. The 83-year-old male specimen demonstrated bridging of the marginal osteophytes along this antero-superior margin, with osseous fusion.
Cartilage thinning and fibrillation was seen in each of the 6 cases (6/9) which had osteophyte formation. The specimen of the youngest patient (20-year-old male) demonstrated no degenerative changes. A 50-year-old female specimen and also an 80-year-old male specimen also had a normal “soft” texture to the interosseous ligaments, and showed no macroscopic evidence of degenerative change. In these latter 3 cases, the articular cartilage was smooth and intact, and showed no evidence of thinning or fibrillation.
In all cases, the interosseous SI ligaments (Fig. 5) consisted of numerous short ligamentous bands crossing the articulation in different directions firmly attaching to the adjacent osseous surfaces of the ilium and sacrum. The opposing surfaces of the ilium and sacrum were composed of corresponding eminences and depressions which interdigitated between the two bones.
Five of the nine specimens (5/9) showed evidence of macroscopic ossification within the SI articulation. Of these five cases with evidence of SI joint ossification, four (4/5) showed central-region ossification within the interosseous SI ligaments, which completely bridged the joint (Fig. 6). The fifth case (1/5), that of the 83-year-old male, demonstrated extensive bridging osteophyte formation along the antero-superior aspect of the articulation, which encroached into the cartilaginous component of the joint.
55-year-old formalin-embalmed female cadaveric specimen. (a) Photograph of the sacral surface of a disarticulated SI joint. Ossification within the central region of the interosseous ligamentous region is outlined. Asterisks indicate the interosseous SI ligament. (b) Photograph of axial section through the right SI joint. Extensive central region ossification (arrow) is seen within the interosseous portion of the articulation. Asterisks delineate the cartilaginous portion of the articulation
Discussion
The local staging of pelvic bone tumours of the sacrum or ilium involves an assessment of transarticular tumour involvement of the SI articulation. This is of critical importance, and has a direct impact on the extent of surgical resection. In the case of a sacral lesion, a sacrectomy may be extended to include the SI articulation when there is transarticular involvement. Similarly a standard or modified internal or external hemipelvectomy for innominate bone tumours may be extended to include part of the sacrum in cases with transarticular involvement. This latter procedure becomes much more demanding, owing to the proximity of the surgical field to important neural structures.
In the current study, tumour extension favoured the posterior ligamentous part of the articulation, which is a finding supported by Ozaki [10] and Drnovsek [11]. The configuration of the SI articulation with close osseous apposition and poor mobility are factors that have been previously described [1] as significant in making this site the most commonly involved by transarticular tumour extension. The cartilaginous surfaces are believed to provide some resistance to tumour spread [1]. The interdigitating eminences and depressions within the interosseous component have a thinner cortex, which may allow for easier transmission of tumour.
Sashin in 1930 [5] described changes occurring with age within the SI articulation, which have subsequently been supported by others [3, 12–14]. The degenerative changes described in the literature focus only on the cartilaginous component. The earliest degenerative changes are irregularity and thinning of the articular cartilage followed by fibrillation, fibrous replacement and fibrous ankylosis. True intra-articular bony ankylosis of the joint however is quite rare [12–14]. Osteoarthritic changes occur around the anterior and superior margin of the articulation, and vary from small osteophytes to large osteophytic masses, often with osseous bridging following the 5th to 6th decades of life. There is agreement in the literature regarding degenerative changes being more common in men and commencing earlier—by the 4th decade—whereas in women these changes commonly commence in the 5th decade [14]. The osseous bridging demonstrated within the central portion of the interosseous component of the articulation presumably represents a degenerative enthesopathic process, which would contribute to both osseous bridging and limitation of mobility.
Age-related changes affecting the SI articulation, including osseous ankylosis, cartilage degeneration and progressive immobility, could all be regarded as factors promoting transarticular tumour extension [10]. This was not supported by the findings of the current study. The mean age of patients with transarticular tumour involvement was almost 10 years younger than those without (mean ages 48 and 56 years respectively). This finding could be related to the age distribution of the particular tumour types in each patient group, and could be further evaluated by studying a larger number of cases.
Extension of metaphyseal intraosseous sarcomas across the osseous-tendinous junctions has been demonstrated [15], with tumour extension along the cruciate ligaments of the knee and also the knee-joint capsule. Similarly, tumour extension has been shown across the hip joint along the ligament of the head of the femur, either from the acetabulum to the femoral head or vice versa [16]. Anatomic studies on cruciate ligaments [17, 18] have demonstrated intraligamentous and paraligamentous vessels, and thus the mode of tumour spread along ligaments may be primarily haematogenous. Articular cartilage, being avascular, thus provides no direct anatomic pathway for tumour invasion. It can therefore be understood how the bridging interosseous ligaments could provide a preferential route for transarticular tumour invasion [11].
Ozaki [10] demonstrated tumour histology as an important factor for infiltration, with chondrosarcoma and osteosarcoma infiltrating more frequently than Ewing's sarcoma. The current study also demonstrated this relative frequency of transarticular infiltration for these particular tumour types; however, the total number of patients evaluated does not allow comment on whether this is significant.
Five of the total of 24 cases arose from the sacrum, and three of these demonstrated transarticular tumour extension. Although it is conceivable that tumours of sacral origin may be more likely to invade the articulation due to the confined space available for spread, this was not shown in the current study. The number of patients evaluated in this study was too small to evaluate the difference in the rate of transarticular involvement in tumours of sacral and iliac origin.
This study demonstrated that pelvic tumours often present at a late stage of disease, at a point when there was extensive involvement of the SI articulation. In those cases where the SI articulation was less extensively involved, it was the interosseous ligamentous portion of the articulation which was primarily infiltrated. In no case was the cartilaginous portion of the articulation solely infiltrated without involvement of the interosseous ligamentous portion. The surgical management will be dependent on the overall tumour extent and SI joint involvement. It will not normally be influenced by which component of the articulation is involved; however, when evaluating this region, the interosseous component is the preferred site for tumour invasion.
Conclusion
Tumour invasion across the SI articulation favours its interosseous ligamentous portion. Factors influencing transarticular tumour extension and its preferential course across the interosseous component of the articulation have been discussed. It is particularly important to assess the interosseous ligamentous portion of the SI articulation when locally staging primary pelvic bone tumours subjacent to the SI articulation, as this will have a significant impact on planning surgical management [13].
References
Abdelwahab IF, Miller TT, Hermann G, Klein MJ, Kenen S, Lewis MM. Transarticular invasion of joints by bone tumours: hypothesis. Skelet Radiol 1991;20:279–83
Terminologica Anatomica. International anatomical terminology. 1998:21
Schunke GB. The anatomy and development of the SI joint in man. Anat Rec 1938;72 3:313–31
Resnick D, Niwayama G. Anatomy of individual joints. In: Resnick D, editor. Diagnosis of bone and joint disorders. Philadelphia: WB Saunders; 1995:2 3:717–8
Sashin D. A critical analysis of the anatomy and the pathologic changes of the sacroiliac joints. J Bone Joint Surg 1930;12:892–910
Resnick D. Articular anatomy and histology. In: Resnick D, editor. Diagnosis of bone and joint disorders. Philadelphia: W.B. Saunders; 2002. p. 688–707
Puhakka K, Melsen F, Jurik A, Boel L, Vesterby A, Egund N. MR imaging of the normal sacroiliac joint with correlation to histology. Skelet Radiol 2004;33:15–28
Agur A, Dalley A. Grant's atlas of anatomy. 11th ed. Baltimore, Maryland: Lippincott Williams and Wilkins; 2005
Ozaki T, Lindner N, Hillmann A, Link T, Winkelmann W. Transarticular invasion of iliopelvic sarcomas into the sacrum. Acta Orthop Scand 1997;68 4:381–3
Ozaki T, Rodl R, Gosheger G, et al. Sacral infiltration in pelvic tumours. Clin Orthop Relat Res 2003;407:152–8
Drnovsek V, Zafiroski G, Byron IG, Plavsic BM. Transarticular spread of Ewing's Sarcoma across the sacroiliac joint: CT and MRI correlation. Orthopaedics 1999;22:977–9
Macdonald G, Hunt T, Sacroiliac joints: observations on the gross and histological changes in the various age groups. Can Med Assoc J 1952;66:157–63
Bowen V, Cassidy JD. Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine 1981;6 6:620–8
Walker J. Age related differences in the human sacroiliac joint: a histological study; implications for therapy. J Orthop Sports Rel Ther 1986;7 6:325–34
Simon MA, Hecht JD. Invasion of joints by primary bone sarcomas in adults. Cancer 1982;50 8:1649–55
Alkalay D, Kollender Y, Mozes M, Meller I. Transarticular tumor invasion via ligamentum teres—a clinical pathologic study of 12 patients. Acta Orthop Scand 1998;69 1:29–30
Alm A, Stromberg B. Vascular anatomy of the patella and cruciate ligaments: a micrographic and histologic investigation in the dog. Acta Chir Scand (Suppl) 1974;445:25–35
Arnoczky S, Rubin R, Marshall J. Microvasculature of the cruciate ligaments and its response to injury: an experimental study in dogs. J Bone Joint Surg 1979;61-A:1221–9
Acknowledgements
The authors would like to thank William Wood, Terry Irvine and Jerry Topham (Division of Anatomy, Department of Surgery, University of Toronto) for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chhaya, S., White, L.M., Kandel, R. et al. Transarticular invasion of bone tumours across the sacroiliac joint. Skeletal Radiol 34, 771–777 (2005). https://doi.org/10.1007/s00256-005-0016-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-005-0016-x