Abstract
Primary tumors of sacrum are rare. The most common malignant tumors are metastasis, and only 6% of all malignant tumors arise from the sacrum. Chondrosarcoma is the third most common primary bone malignancy following myeloma and osteosarcoma. Surgery is usually the most important therapeutic modality; the wide en bloc excision remains the treatment of choice. These technically demanding procedures require a multidisciplinary expert team (neurosurgery, surgical and orthopedic oncology, colorectal surgery, and plastic surgery) involvement. We present in this article a case of a 52-year-old man who presented less infrequent symptoms, and the diagnosis was made in a very advanced stage. The wide surgical excision of the mass was performed by two different anterior and posterior approaches in one stage. The free surgical margins were difficult to achieve because it presented a voluminous tumor with invasion of the rectum, bone, and sacral plexus, but the age, low histological grade, and extensive experience in extreme pelvic surgery of our multidisciplinary team allowed approaching the patient with debulking surgery en bloc, successfully. Total hospital stay was 20 days. The patient was discharged without any complications. At the 6-months’ follow-up, the patient showed no local recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary tumors of sacrum are rare. The most common malignant tumors are metastasis, and only 6% of all malignant tumors arise from the sacrum [1].
Chondrosarcoma is the third most common primary bone malignancy following myeloma and osteosarcoma [2, 3].
Chondrosarcomas constitute a heterogeneous group of bone malignant neoplasms that have in common the production of chondroid [2, 3]. They occur predominantly in elderly patients with a peak incidence in the sixth decade, and have a predilection for the shoulders, pelvis, proximal femur, and rib, and rarely involve the sacrum [1, 3, 4].
The clinical behavior is variable; 90% are conventional chondrosarcoma of low and intermediate grade [5]. Although the majorities of these tumors have a slow growth rate, rarely metastasize, and have a very good prognosis after surgery, local recurrence is quite common, especially following inadequate excision [5, 6]. Wide experience in the treatment of other tumors showed the role of IOERT in the control of local recurrence [7].
On the other hand, high-grade chondrosarcoma (5–10%) and some rare variants have high potential metastatic and poor prognosis after resection; however, some rare subtypes are sensitive to chemotherapy and radiotherapy [5, 6, 8].
Surgery is usually the most important therapeutic modality; the wide en bloc excision remains the treatment of choice [6, 9, 10].
These technically demanding procedures require a multidisciplinary expert team (neurosurgery, surgical and orthopedic oncology, and plastic surgery) involvement.
Case Report
We report the case of a 52-year-old man who presented to the hospital with back pain, for more than a year of evolution, with worsening and spreading towards both lower limbs, hypoesthesia of the territory L4, and important functional limitation.
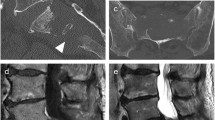
After clinical assessment, the MRI (magnetic resonance imaging) and CT-3D (computed axial tomography) reconstruction images show voluminous S1 sacral mass with invasion of the medullary canal (Image 1).
The histological diagnosis was performed through CT-guided biopsy confirming the presence of chondrosarcoma grade I.
A multidisciplinary team comprising a general surgeon, orthopedic surgeon, plastic surgeon, radiologist, and oncologist in a committee of tumors evaluated the patient’s case. After a joint decision, the patient underwent a selective embolization of both hypogastric arteries and subsequently, surgery.
Before the surgery, inside the operating room, cystoscopy was performed with catheterization of both ureters leaving a simple J catheter.
The surgical excision of the mass was performed by an anterior and posterior approach in one stage. In the abdominal time, the cleavage plane between the tumor and the iliac vessels was dissected; vascular control, ligation of hypogastric arteries and veins, proximal release of the greater omentum, dissection of pararectal space, rectosigmoid resection, and terminal colostomy were performed. A plastic sheet was positioned behind the great vessels in order to protect them from the osteotomy (Image 2).
The intraoperative photograph, abdominal approach shows the chondrosarcoma tumor, dissection, and vascular control. IVC, inferior vena cava; DA, descending aorta; RCIV, right common iliac vein; LCIV, left common iliac vein; RCIA, right common iliac artery; LCIA, left common iliac artery; RU, right ureter; LU, left ureter
During the abdominal time, a right transverse rectus abdominis myocutaneous (TRAM) flap was also performed in order to reconstruct the posterior defect (Image 3).
In the posterior approach, the first step was removing the posterior instrumentation of the previous surgery. The posterior iliac crests, greater sciatic foramina, and sciatic nerves are exposed bilaterally, as well as the L3–5 spinous processes, facet joints, and transverse processes; laminectomy L4 exposes the thecal sac, osteotomy of the left and right iliac wing, and sacroiliac joint; sacral nerve roots are then divided, and the thecal sac is closed with a double layer of sutures, section of the sacrosciatic and sacrospinous ligaments, and medial section of the insertion of both pyramidal muscles; and finally the entire sacrum along with the tumor is then removed en bloc including the rectal stump and L5 (Images 4, 5, and 6). The histopathology performed on the entire specimen revealed the presence of chondrosarcoma G2 (pT2b pN pMx).
In the postoperative period, the patient was held in an intensive care unit (ICU) with prolonged intubation, where he presented infection and partial wound dehiscence which was solved with VAC® Device (Vacuum Assisted Closure, KCI Clinic Spain, S.L.).
Regarding bladder morbidity, the neurogenic bladder with flaccid external sphincter was managed by permanent catheterization. Voluntary bladder control is permanently lost due to sectioning of both S-2 nerve roots, which principally control sphincter function.
The postoperative neurological evaluation with an electromyography showed axonal sensorimotor polyneuropathy of important degree, although it is not possible to rule out a bilateral lumbosacral radicular lesion added. The neurological evolution was progressive and difficult but with the physiotherapy and time, the patient’s gait markedly improved.
Total hospital stay was 20 days. The patient was discharged without any complications.
At the 6-months’ follow-up, the patient showed no local recurrence, and the surgical wound evolved positively.
At the 1-year follow-up review, this patient was able to walk with the use of a cane and regained a good quality of life.
Discussion
The incidence of clinical presentation is more common after the 6th decade, and the onset of symptoms is usually insidious and less often disabling [1, 3, 4].
The key point of our paper is to describe an unusual way of presentation of advanced pelvic chondrosarcoma in a patient under 60 years, with important functional limitation by the invasion of the spinal canal by the sacral mass from S1.
Nowadays, the most important therapeutic modality proven to chondrosarcoma is wide surgical resection with adequate surgical margin, being this the most effective way to reduce tumor recurrence [6, 9,10,11].
The surgeon must keep a delicate balance between ensuring adequate resection margins and the risk of endangering the adjacent vital structures and the structural stability of the pelvis.
In our case, the free surgical margins were difficult to achieve because it presented a voluminous tumor with invasion of bone and nerve (sacral plexus) structures. Therefore, total en bloc sacrectomy of the tumor-bearing sacrum with detachment of the sacroiliac joints was performed, and posterior fixation of the pelvis with iliolumbar instrumentation from L2 with iliac screws and double cross bars to ensure the stability of the pelvis [9,10,11].
The prognosis depends on several factors: histological grade, local recurrence, tumor location (the pelvic location is a negative prognostic factor), tumor volume, and age. According to different series, survival rate is 60–70% at 5 years and 50–60% at 10 years [5, 6, 8].
According to the patient’s history, he had a pelvic tumor with symptoms that limited the functionality and his quality of life. The age, low histological grade, and extensive experience in extreme pelvic surgery allowed approaching the patient with “en bloc” surgical excision, successfully. Despite having complications inherent to the intervention, we think this was the most appropriate therapeutic option to improve the quality of life and the patient’s survival.
The management of tumors of the sacrum is challenging. Radical resection through partial or complete sacrectomy can prolong the overall survival of patients, especially if it is performed by expert surgeons with a long experience in these types of tumors.
References
Mavrogenis AF, Pavlos P, Georgia K, Papagelopoulos Panayiotis J (2009) Tumours of the sacrum. Orthop. 32:5–5
Hogendoorn PCW, Bovee JM, Nielsen GP (2013) Chondrosarcoma (grades I-III), including primary and secondary variants and periosteal chondrosarcoma. In: CDM F, Bridge JA, PCW H, Mertens F (eds) World Health Organization classification of tumours of soft tissue and bone, vol 5, 4th edn. IARC, Lyon, p 264
Gelderblom H, Hogendoorn PCW, Dijkstra SD et al (2008) The clinical approach towards chondrosarcoma. Oncologist 13(3):320–329
Bjornsson J, McLeod RA, Unni KK, Ilstrup DM, Pritchard DJ (1998) Primary chondrosarcoma of long bones and limb girdles. Cancer. 83:2105–2119
Angelini A, Guerra G, Mavrogenis AF et al (2012) Clinical outcome of central conventional chondrosarcoma. J Surg Oncol 106:929
Wirbel RJ, Schulte M, Maier B, Koschnik M, Mutschler WE (2000) Chondrosarcoma of the pelvis: oncologic and functional outcome. Sarcoma 4(4):161–168
Jullien-Petrelli AC, Asencio JM, Orue-Echebarria MI, Lozano P, Álvarez A, Serrano J, Calvo FM, Calvo-Haro JA, Lasso JM, García-Sabrido JL (2017 Sep 4) Role of intraoperative radiotherapy in the treatment of sacral chordoma. Spine J.
Sheth DS, Yasko AW, Johnson ME, Ayala AG, Murray JA, Romsdahl MM (1996) Chondrosarcoma of the pelvis. Prognostic factors for 67 patients treated with definitive surgery. Cancer 78:745–750
Hsieh PC, Xu R, Sciubba DM, MJ MG, Nelson C, Witham TF, Wolinsky JP (2009) Long-term clinical outcomes following en bloc resections for sacral chordomas and chondrosarcomas. Spine. 34(20):2233–2239
Fiorenza F, Abudu A, Grimer RJ et al (2002) Risk factors for survival and local control in chondrosarcoma of bone. J Bone Joint Surg Br 84:93
Gillis CC, Street JT, Boyd MC, Fisher CG (Oct 2014) Pelvic reconstruction after subtotal sacrectomy for sacral chondrosarcoma using cadaveric and vascularized fibula autograft. J Neurosurg Spine 21(4):623–627
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morales, A.G., Sabrido, J.L.G., Calvo, J.A. et al. Total Sacrectomy for the Treatment of Advanced Pelvic Chondrosarcoma. Indian J Surg Oncol 11 (Suppl 1), 27–32 (2020). https://doi.org/10.1007/s13193-019-01009-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-019-01009-1