Abstract
Early and accurate diagnosis of invasive aspergillosis (IA) is one of the most critical steps needed to efficiently treat the infection and reduce the high mortality rates that can occur. We have previously found that the Aspergillus spp. secondary metabolite, bis(methylthio)gliotoxin (bmGT), can be detected in the serum from patients with possible/probable IA. Thus, it could be used as a diagnosis marker of the infection. However, there is no data available concerning the sensitivity, specificity and performance of bmGT to detect the infection. Here, we have performed a prospective study comparing bmGT detection with galactomannan (GM), the most frequently used and adopted approach for IA diagnosis, in 357 sera from 90 episodes of patients at risk of IA. Our results, involving 79 patients that finally met inclusion criteria, suggest that bmGT presents higher sensitivity and positive predictive value (PPV) than GM and similar specificity and negative predictive value (NPV). Importantly, the combination of GM and bmGT increased the PPV (100 %) and NPV (97.5 %) of the individual biomarkers, demonstrating its potential utility in empirical antifungal treatment guidance and withdrawal. These results indicate that bmGT could be a good biomarker candidate for IA diagnosis and, in combination with GM, could result in highly specific diagnosis of IA and management of patients at risk of infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive aspergillosis (IA) is a severe opportunistic infection with high morbidity and mortality rates caused by fungi of the genus Aspergillus, which mainly affects neutropenic patients (Kousha et al. 2011). The high mortality rates are in part due to deficiencies associated with early and specific diagnosis. IA diagnosis has evolved during the last years thanks to the introduction of galactomannan (GM) detection (Maertens et al. 1999, 2001, 2002). In 2008, this biomarker was included by the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) as defining criteria of probable IA (De Pauw et al. 2008). Nevertheless, there is increasing concern about its reliability due to false positives primarily caused by beta-lactam antibiotics or intravenous solutions (Sulahian et al. 2003; Martín-Rabadán et al. 2012) and false negatives due to antimould prophylaxis (Marr et al. 2005). Although other non-culture-based diagnostic tools have been developed, its routine use in clinical diagnosis is unequal due to several reasons: 1,3-beta-D-glucan is not specific of Aspergillus species since it is a cell wall component of many fungi; PCR is a promising tool but the lack of standardization has precluded its widespread clinical adoption (White et al. 2010; Arvanitis et al. 2014). The clinical utility of the first commercially available PCR assay MycAssay Aspergillus (Myconostica, Ltd) has to be properly evaluated in large prospective studies (White et al. 2011; Danylo et al. 2014). The same applies to the recently commercialized lateral flow device which detects an extracellular glycoprotein (White et al. 2013). Finally, it has been described that certain volatile organic compounds such as 2-pentylfuran can be detected in the breath of patients infected with Aspergillus spp. as they tend to produce them (Chambers et al. 2009). However, large studies are needed to warrant its clinical utility.
Due to the above-mentioned problems, investigation of new biomarkers is required (Arvanitis and Mylonakis 2015). Gliotoxin (GT) has been proposed as a diagnostic biomarker of IA (Lewis et al. 2005a; Puri et al. 2010; Cerqueira et al. 2014). GT belongs to a class of toxins with a common epipolythiodioxopiperazine structure, characterized by an internal disulphide bridge which is responsible of its biological activity (Müllbacher et al. 1986). It is well known that GT mediates immunosuppressive and proapoptotic effects, acting as virulence factor during hyphal growth (Waring et al. 1988; Sutton et al. 1996; Tsunawaki et al. 2004; Sugui et al. 2007). The most important GT producing opportunistic human pathogen is Aspergillus fumigatus, responsible of the majority of the IA cases (Latgé 1999). Other non-A. fumigatus Aspergillus species (A. flavus, A. terreus, A. niger) commonly causing IA can also produce GT (Lewis et al. 2005b). Penicillium spp., Gliocladium spp., Trichoderma virens, Colletotrichum gloeoporoides or Pseudallescheria sp. MFB165 are also able to produce GT (Gardiner et al. 2005; Li et al. 2006; Guimarães et al. 2010; Dolan et al. 2014), but they are not common opportunistic human pathogens. The genus Candida, the most frequent cause of invasive fungal infection, lacks to produce GT (Kupfahl et al. 2007). All these characteristics make GT suitable as a specific IA biomarker. However, GT is a very reactive compound that it is rapidly took up by tissues and circulating cells and hard to detect in body fluids (Amitani et al. 1995; Bernardo et al. 2003; Domingo et al. 2012). This could be due to the high reactivity of GT since its disulphide bridge is very unstable, and it is rapidly cell associated and removed from body fluids (Waring et al. 1988). Conversely, bis(methylthio)gliotoxin (bmGT) is a more stable inactive metabolite produced by the blockage of the disulphide bond present in GT by methylation (Müllbacher et al. 1986). GT methylation seems to be used by the fungus to regulate GT synthesis. Thus, active GT activates a fungal methyltransferase that induces the synthesis of bmGT (Dolan et al. 2014). This methyltransferase is called gliotoxin bis-thiomethyltransferase (GtmA), and it is encoded by the gene gtmA. It has been described that all species belonging to the filamentous ascomycetes contain a GtmA homolog and thus, the potential ability of producing bmGT. Accordingly, bmGT has been identified in several of the GT-producing fungal species like A. fumigatus, Penicillium spp., T. virens, Gliocladium spp., C. gloeosporoides or Pseudallescheria sp. MFB165 (Kirby et al. 1980; Guimarães et al. 2010; Domingo et al. 2012; Sun et al. 2012). Studies describing the distribution of bmGT production within the Aspergillus genus are lacking. We have been able to identify bmGT production in cell cultures from A. fumigatus, A. flavus, A. niger and A. nidulans but not from A. terreus (manuscript in preparation). Our group demonstrated that bmGT is produced by a higher percentage of isolates of A. fumigatus than GT. BmGT is also recovered from serum of a higher amount of patients at risk of IA than GT (Domingo et al. 2012). These results suggest that bmGT is a more reliable indicator of infection than GT. Thus, bmGT has the potential to be a suitable biomarker for IA diagnosis. However, results on the clinical validity of bmGT to accurately diagnose IA are not yet available. In this study, we have assessed the diagnostic validity of bmGT compared to GM for IA diagnosis. As a secondary outcome, we have analysed its correlation with mortality and antifungal treatment.
Material and methods
Patients and study design
Patients hospitalized in a tertiary care center to whom GM detection was requested from May to December 2013 were included in the study. They were prospectively and consecutively recruited if they met the inclusion criteria: underlying disease (hematologic or oncologic malignancy and solid organ transplant recipients) or host factors according to the EORTC/MSG criteria (neutropenia for more than 10 days, allogenic stem cell transplant, prolonged use of corticosteroids, treatment with T cell immunosuppressants) (De Pauw et al. 2008). GM was requested as a screening tool of IA regardless of clinical symptoms. Clinicians were unaware of GT and bmGT results. The study followed a double-blind protocol where investigators involved in the analysis of GT and bmGT were different from those involved in medical record revision. Data collection was retrospective; if the medical record was not available, the patients were excluded from the study. The study was approved by the local ethics committee CEICA (PI12/0041 and PI15/0197). Standards for reporting of diagnostic accuracy (STARD) were followed (Altman and Bossuyt 2005).
GM, bmGT and GT assays
GM detection was performed in serum samples with the commercially available Platelia™ Aspergillus Ag Kit (BioRad, Hercules, CA, USA) twice weekly, according to the manufacturer’s recommendations. A result was considered positive for optical reading index ≥0.5. A second sample was requested for confirmation of low indexes (<0.7).
BmGT and GT detection was performed by high-performance thin layer chromatography (HPTLC) as described by Domingo et al. (2012). Briefly, GT and bmGT were extracted with dichloromethane from serum samples and applied onto HPTLC plates. Separation and quantification were performed using the mixture tetrahydrofuran/n-heptane/acetonitrile (40:58:2 (v/v/v)) for 25 min in a horizontal development chamber. Peak area after ultraviolet scanning densitometry was measured for GT and bmGT quantification. Any result of GT and bmGT was considered positive.
Data analysis
Receiver operator characteristic (ROC) curves were constructed using EPIDAT 3.1. Sensitivity, specificity, positive and negative predictive values (PPV, NPV) were calculated. The cut-off value was calculated by the Youden index. As EORTC/MSG criteria include GM within the definition of probable IA, it introduces a bias for the direct comparison with bmGT. As previously described by Barnes et al. (2013), we resolved this problem by two different strategies: (i) modifying EORTC/MSG criteria to exclude GM from the definition and taking as probable cases those with positive microbiology to Aspergillus spp. and (ii) adding bmGT to EORTC/MSG criteria, giving the same value to bmGT as to GM. The association between qualitative variables was calculated by hypothesis testing chi-square; odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. Comparison between categorical and quantitative variables was analyzed by Mann-Whitney U test. Two-sided P values <0.05 were considered statistically significant.
Results
Patient’s baseline characteristics
From May to December 2013, sera from 105 consecutive patients were sent for GM determination to the laboratory. It was not possible to review the medical record from 18 patients. Eight patients did not meet inclusion criteria. Finally, a total of 79 patients met inclusion criteria, corresponding to 90 hospitalization events (Fig. 1). Sixty seven percent of the patients were male. The average age was 64.9 ± 16.9 years. The most frequent underlying disease was hematological (75.6 %); oncological patients were 18.9 % and solid organ transplant recipients 4.4 % (Table 1).
Incidence of IA
According to the revised definitions provided by the EORTC/MSG, there were 10 episodes (11.1 %) of possible IA, five episodes of probable IA (5.5 %) and a proven episode of IA (1.1 %). The incidence of proven/probable aspergillosis was 6.6 %. The proven case was histologically confirmed by brain biopsy. A. fumigatus was isolated from respiratory samples from three patients with probable disease; the fourth patient suffered a mixed infection with isolation of A. flavus and A. terreus. The fifth probable case was diagnosed by positive GM.
Diagnostic accuracy for the detection of IA
During the study period, a total of 357 sera from the 79 patients fulfilling inclusion criteria were analyzed. GT was analyzed in all the sera; none of the samples tested was positive. For this reason, henceforth, we will exclusively refer to bmGT. A summary of the analyses is shown in Table 2.
Probable/proven cases
There were 13 sera from six cases of probable/proven IA, 12 from probable IA and one from proven IA. Four of these six cases were positive for both biomarkers (GM and bmGT) in at least one serum (cases 1, 2, 4 and 6). Another one was negative for both biomarkers (case 3), and the last one was positive for bmGT but negative for GM (case 5) (Table 2).
Possible cases
There were 34 sera from 10 cases of possible IA without mycological evidence (culture or GM) of fungal disease but showing clinical and radiological evidences of disease. This group was considered to have no IA. From these ten cases, two patients had a GM index between 0.5 and 0.7, which was not confirmed in the following sample. Both patients (11 and 16) died between 8 and 16 days after initiating broad spectrum antimould treatment, suggesting probable disease. In contrast to GM index that was considered negative, both cases were positive for bmGT supporting a diagnosis of probable infection and the potential utility of bmGT for IA detection. From the remaining 8 cases, four were positive for bmGT; three of them required different antimould treatments and died between 33 and 55 days after (cases 8, 13 and 15). Among the patients with negative bmGT, two died in less than 25 days, one receiving voriconazole (case 14) (Table 2).
Patients not fulfilling EORTC/MSG criteria
There were 310 sera from 24 cases that did not fulfill EORTC/MSG criteria. Within this group, 20 sera corresponding to 15 cases were falsely positive in GM, and 12 sera corresponding to 9 cases were falsely positive in bmGT. The remaining sera were negative for both biomarkers.
Diagnostic performance according to EORTC/MSG criteria:
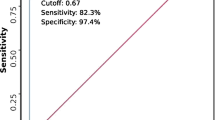
bmGT showed higher sensitivity, PPV and NPV but slightly lower specificity than GM for probable/proven IA as shown in Table 3. ROC curve analysis showed a higher area under curve (AUC) for bmGT (0.768, 95% CI, 0.631–0.904) than for GM (0.659, 95% CI, 0.521–0.798) although the difference was not statistically significant (p = 0.06). The difference in AUC between GM and bmGT may be due to the fact that we have considered any value of bmGT as positive. Youden Index suggests a cut-off value of 2.17 mg/l for bmGT, with a sensitivity of 61.5 % and a specificity of 93.6 %. We looked for the correlation between quantitative bmGT and EORTC/MSG category. The Mann-Whitney U test showed statistical differences (p < 0.01) between the median bmGT quantity among the no IA/possible IA cases (1.31 mg/l ± 7.12 mg/l) compared to probable/proven cases (7.13 mg/l ± 10.38 mg/l).
(i) Consensus criteria without GM: similar results were obtained when GM was withdrawn from the criteria and only patients with a positive mycological culture were taken into account. This is likely due to the contribution of GM detection contributing to the category of probable IA only in one patient. Sensitivity, specificity, PPV and NPV were 55.6, 92.2, 15.6 and 98.8 %, respectively, for bmGT and 33.3, 94.0, 12.5 and 98.2 %, respectively, for GM. AUC for bmGT was 0.734 (95% CI, 0.563–0.904) and 0.637 for GM (95% CI, 0.468–0.805) without significant differences (p = 0.17).
(ii) Consensus criteria with bmGT: when bmGT was included in defining criteria, a bias was introduced as possible cases with detectable bmGT were considered as probable cases. Thus, higher sensitivity and PPV were got for this biomarker, 76 and 59.4 %, respectively. In contrast, for GM, the lowest sensitivity was found (20 %) without lowering PPV. Specificity and NPV were high (>93 %) for both biomarkers. AUC for bmGT (0.865, 95% CI, 0.778–0.952) was higher than for GM (0.566, 95% CI, 0.485–0.647), and in this case, the difference was statistically significant (p < 0.01). See Fig. 2.
When both biomarkers were used in combination, specificity, PPV and NPV reached encouraging high values, 100, 100 and 97.5 %, respectively, (Table 3), suggesting its potential utility in preemptive approaches for guiding antifungal treatment.
Correlation with mortality
Overall 30-day mortality was 21.1 % (19/90). Among patients with possible IA, 30-day-mortality was 40 % (4/10), and among patients with probable/proven IA, it was 83.3 % (5/6). In the group without IA, mortality was 13.5 % (10/74) within 30-days. We have analyzed the correlation between the presence of individual biomarkers and mortality and found a significant correlation between bmGT and mortality (OR, 3.2, 95% CI, 1.1–9.6, p = 0.03) but not between GM and mortality (OR, 1.3, 95% CI, 0.4–4.2, p = 0.62). Moreover, there was a significant difference (p < 0.01) between the amount of bmGT found in patients who died (2.36 mg/l ± 4.76 mg/l) compared to those who survived (1.4 mg/l ± 7.58 mg/l).
Correlation with antifungal treatment
Antimould therapy (voriconazole, amphothericin B, echinocandins) was initiated in 42 episodes. In eight of them (19 %), antifungals were administered as prophylaxis. None of these patients developed IA, and none of them had detectable bmGT but two of them were positive in GM and were considered as false positives by clinicians. Twelve patients (28.6 %) received antimoulds as treatment: six probable/proven IA patients and six patients that did not fulfil EORTC/MSG criteria with detectable GM. The remaining 22 episodes (7 possible IA and 15 without IA), which were GM negative, required antimoulds as empirical treatment due to neutropenic febrile episodes or respiratory infection in patients at high risk of IA. We found a significant correlation between bmGT presence and requirement for antimould treatment (OR, 5.68, 95% CI, 1.61–19.99, p = 0.01). Requirement for increased antifungal could reflect a worse clinical situation, and thus, it could be considered as an indirect marker of illness severity. Accordingly, this result suggests that bmGT might correlate with disease evolution.
Discussion
Despite recent advances, IA diagnosis is still difficult and challenging. The clinical manifestations of IA are often non-specific, and a definitive IA diagnosis depends on invasive procedures that are not always feasible due to the patient’s condition. A sensitive and specific test is required to early diagnose this life-threatening complication and guide rational antifungal treatment to increase efficacy and reduce side effects and costs (Thornton 2010). Here, we compared the diagnostic accuracy of bmGT with that of GM and, in addition, the combination of both. Results are promising and suggest that bmGT and GM could be used in combination to specifically detect IA and guide antifungal therapy.
Some groups have suggested that detection of the mycotoxin GT in serum could be used for IA diagnosis (Lewis et al. 2005a; Puri et al. 2010; Cerqueira et al. 2014). In contrast to these works, we were not able to detect it in our cohort even if our technique is appropriate and shown to be sensitive (Domingo et al. 2012). This finding has been confirmed and expanded in the present work where GT was not detected in any of the analyzed sera. This is explained by the fact that we and others have shown that active GT is quickly incorporated by tissues and cells being hard to find in body fluids (Amitani et al. 1995; Bernardo et al. 2003; Domingo et al. 2012). In this sense and according to our results, bmGT seems to be a more suitable test as it was reliably detected in a large number of sera.
The detection of GM antigen has improved the managements of patients at risk of infection. In two large meta-analyses assessing diagnostic accuracy of GM for IA, sensitivity was around 70 % and specificity was around 90 %. These values vary depending on the used cut-off; the higher GM index was considered positive; the lower sensitivity and higher specificity were obtained (Pfeiffer et al. 2006; Leeflang et al. 2008). In a recent clinical study, GM screening was performed even in asymptomatic patients, the NPV was 100 % and PPV was 11.8 % (Duarte et al. 2014). PPV reached 89.6 % if only patients with suspected IA were included. The low PPV is in accordance with that observed in our study, 16.7 %.
A single test with low PPV cannot be used to diagnose IA and to guide antifungal use. Therefore, screening algorithms based on high-risk populations, clinical criteria and the use of different biomarkers in combination are essential for diagnosis and management of this kind of patients and have proven to diminish empiric antifungal treatment without increasing mortality (Aguilar-Guisado et al. 2012; Barnes et al. 2013). Our results indicate that the combination of serum GM and bmGT substantially improves the PPV (100 %) in probable/proven IA keeping good specificity (100 %) and NPV (97 %). This finding suggests the potential utility of bmGT and GM in empirical antifungal treatment guidance and withdrawal. Other works have also evaluated the combination of biomarkers for IA diagnosis. In two clinical trials, the combination of PCR and GM detection lowered the empirical antifungal treatment, diagnosis was performed earlier and incidence of IA was reduced (Morrissey et al. 2013; Aguado et al. 2014). In the next steps, we will prospectively test if GM and bmGT detection renders a similar result in the management of patients at risk of IA.
Our study also suggests that bmGT could be more sensitive than GM with similar specificity and higher PPV. The significance of a positive bmGT result merits consideration as it correlates with mortality and increased antimould requirement. These two parameters are indicative of illness severity suggesting that bmGT could correlate with disease evolution. Moreover, high amounts of serum bmGT correlate with mortality and probable/proven IA according to EORTC/MSG criteria. The ROC curve analysis according to EORTC/MSG criteria rendered a cut-off value of 2.17 mg/l for bmGT. All but one probable/proven IA cases had a higher amount of bmGT than 2.17 mg/l. However, it was also detectable in high amounts in five of the ten possible cases. Unfortunately, we did not take samples of the intravenous formulations that patients were receiving, in an attempt to detect sources of false positives. More experiments will be required to show if bmGT presence in patients with negative GM and negative mycological culture is indicative of IA, confirming a low sensitivity of those tests (Mennink-Kersten et al. 2004; Fraczek et al. 2014), or it is a false positive of the novel biomarker. If properly confirmed in large prospective studies, this finding would indicate that bmGT could be used not only as a diagnostic biomarker but also as marker of disease severity.
Retrospective data collection and the small sample size were the main limitations of our study. In addition, the use of HPTLC or high-performance liquid chromatography in clinical laboratories is not common and difficult to implement. On this regard, development of immunochemical methods like ELISA will be required, and our group is working on it. The optimal strategy for management of patients at risk of IA has still to be investigated. It depends on owns institutions particularities including IA prevalence, at-risk population, strategies for antifungal usage (prophylaxis, pre-emptive, empiric therapy), cost-economic studies and diagnostic tool availability. Due to the high morbid-mortality of IA all efforts should be made for early diagnosis of this severe disease that has a high economic impact in healthcare (Menzin et al. 2009; Ashley 2011). According to our study, bmGT shows potential usefulness as diagnostic tool of IA and in the management of patients at risk of aspergillosis. Nevertheless, additional prospective studies using a larger cohort of patients with IA will be required to confirm this conclusion and support the implementation of bmGT in hospitals.
References
Aguado JM, Vázquez L, Fernández-Ruiz M, Villaescusa T, Ruiz-Camps I, Barba P, Silva JT, Batlle M, Solano C, Gallardo D, Heras I, Polo M, Varela R, Vallejo C, Olave T, López-Jiménez J, Rovira M, Parody R, Cuenca-Estrella M (2014) Serum galactomannan versus a combination of galactomannan and polymerase chain reaction-based Aspergillus DNA detection for early therapy of invasive aspergillosis in high-risk hematological patients: a randomized controlled trial. Clin Infect Dis 60(3):405–414
Aguilar-Guisado M, Martin-Pena A, Espigado I, de Ruiz Perez Pipaon M, Falantes J, de la Cruz F, Cisneros JM (2012) Universal antifungal therapy is not needed in persistent febrile neutropenia: a tailored diagnostic and therapeutic approach. Haematologica 97(3):464–471
Altman DG, Bossuyt PMM (2005) Diagnostic (STARD) and prognostic (REMARK) studies. Med Clin 125(Supl. 1):49–55
Amitani R, Taylor G, Elezis EN, Llewellyn-Jones C, Mitchell J, Kuze F, Cole PJ, Wilson R (1995) Purification and characterization of factors produced by Aspergillus fumigatus which affect human ciliated respiratory epithelium. Infect Immun 63(9):3266–3271
Arvanitis M, Mylonakis E (2015) Diagnosis of invasive aspergillosis: recent developments and ongoing challenges. Eur J Clin Investig 45(6):646–652
Arvanitis M, Ziakas PD, Zacharioudakis IM, Zervou FN, Caliendo AM, Mylonakis E (2014) PCR in diagnosis of invasive aspergillosis: a meta-analysis of diagnostic performance. J Clin Microbiol 52(10):3731–3742
Ashley ED (2011) Pharmacoeconomics of antifungal therapy: current considerations. Curr Opin Infect Dis 24(suppl 2):S30–S40
Barnes RA, Stocking K, Bowden S, Poynton MH, White PL (2013) Prevention and diagnosis of invasive fungal disease in high-risk patients within an integrative care pathway. J Infect 67(3):206–214
Bernardo PH, Brasch N, Chai CLL, Waring P (2003) A novel redox mechanism for the glutathione-dependent reversible uptake of a fungal toxin in cells. J Biol Chem 278(47):46549–46555
Cerqueira LB, de Francisco TMG, Gasparetto JC, Campos FR, Pontarolo R (2014) Development and validation of an HPLC-MS/MS method for the early diagnosis of aspergillosis. PLoS One 9(4):e92851
Chambers ST, Syhre M, Murdoch DR, McCartin F, Epton MJ (2009) Detection of 2-pentylfuran in the breath of patients with Aspergillus fumigatus. Med Mycol 47(5):468–476
Danylo A, Courtemanche C, Pelletier R, Boudreault AA (2014) Performance of MycAssay Aspergillus DNA real-time PCR assay compared with the galactomannan detection assay for the diagnosis of invasive aspergillosis from serum samples. Med Mycol 52(6):577–583
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Muñoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46(12):1813–1821
Dolan SK, Owens RA, O’Keeffe G, Hammel S, Fitzpatrick DA, Jones GW, Doyle S (2014) Regulation of nonribosomal peptide synthesis: bis-thiomethylation attenuates gliotoxin biosynthesis in Aspergillus fumigatus. Chem Biol 21(8):999–1012
Domingo MP, Colmenarejo C, Martínez-Lostao L, Müllbacher A, Jarne C, Revillo MJ, Delgado P, Roc L, Meis JF, Rezusta A, Pardo J, Gálvez EM (2012) Bis(methyl)gliotoxin proves to be a more stable and reliable marker for invasive aspergillosis than gliotoxin and suitable for use in diagnosis. Diagn Micr Infec Dis 73(1):57–64
Duarte RF, Sánchez-Ortega I, Cuesta I, Arnan M, Patiño B, de Sevilla AF, Gudiol C, Ayats J, Cuenca-Estrella M (2014) Serum galactomannan–based early detection of invasive aspergillosis in hematology patients receiving effective antimold prophylaxis. Clin Infect Dis 59(12):1696–1702
Fraczek MG, Kirwan MB, Moore CB, Morris J, Denning DW, Richardson MD (2014) Volume dependency for culture of fungi from respiratory secretions and increased sensitivity of Aspergillus quantitative PCR. Mycoses 57(2):69–78
Gardiner DM, Waring P, Howlett BJ (2005) The epipolythiodioxopiperazine (ETP) class of fungal toxins: distribution, mode of action, functions and biosynthesis. Microbiol 151(4):1021–1032
Guimarães DO, Borges WS, Vieira NJ, de Oliveira LF, da Silva CHTP, Lopes NP, Dias LG, Durán-Patrón R, Collado IG, Pupo MT (2010) Diketopiperazines produced by endophytic fungi found in association with two Asteraceae species. Phytochemistry 71:1423–1429
Kirby GW, Robins DJ, Sefton MA, Talekar RR (1980) Biosynthesis of bisdethiobis(methylthio)gliotoxin, a new metabolite of Gliocladium deliquescen. J Chem Soc Perkin Trans 1:119–121
Kousha M, Tadi R, Soubani AO (2011) Pulmonary aspergillosis: a clinical review. Eur Respir Rev 20(121):156–174
Kupfahl C, Ruppert T, Dietz A, Geginat G, Hof H (2007) Candida species fail to produce the immunosuppressive secondary metabolite gliotoxin in vitro. FEMS Yeast Res 7(6):986–992
Latgé JP (1999) Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev 12(2):310–350
Leeflang MM, Debets-Ossenkopp YJ, Visser CE, Scholten RJ, Hooft L, Bijlmer HA, Reitsma JB, Bossuyt PMM, Vandenbroucke-Grauls CM (2008) Galactomannan detection for invasive aspergillosis in immunocompromized patients. Cochrane Database Syst Rev. doi:10.1002/14651858.CD007394
Lewis RE, Wiederhold NP, Chi J, Han XY, Komanduri KV, Kontoyiannis DP, Prince RA (2005a) Detection of gliotoxin in experimental and human aspergillosis. Infect Immun 73(1):635–637
Lewis RE, Wiederhold NP, Lionakis MS, Prince RA, Kontoyiannis DP (2005b) Frequency and species distribution of gliotoxin-producing Aspergillus isolates recovered from patients at a tertiary-care cancer center. J Clin Microbiol 43(12):6120–6122
Li X, Kim SK, Nam KW, Kang JS, Choi HD, Son BW (2006) A new antibacterial dioxopiperazine alkaloid related to gliotoxin from a marine isolate of the fungus Pseudallescheria. J Antibiot 59(4):248–250
Maertens J, Van Eldere J, Verhaegen J, Verbeken E, Verschakelen J, Boogaerts M (2002) Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis 186(9):1297–1306
Maertens J, Verhaegen J, Demuynck H, Brock P, Verhoef G, Vandenberghe P, Van Eldere J, Verbist L, Boogaerts M (1999) Autopsy-controlled prospective evaluation of serial screening for circulating galactomannan by a sandwich enzyme-linked immunosorbent assay for hematological patients at risk for invasive aspergillosis. J Clin Microbiol 37(10):3223–3228
Maertens J, Verhaegen J, Lagrou K, Van Eldere J, Boogaerts M (2001) Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood 97(6):1604–1610
Marr KA, Laverdiere M, Gugel A, Leisenring W (2005) Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis 40(12):1762–1769
Martín-Rabadán P, Gijón P, Alonso Fernández R, Ballesteros M, Anguita J, Bouza E (2012) False-positive Aspergillus antigenemia due to blood product conditioning fluids. Clin Infect Dis 55(4):e22–e27
Mennink-Kersten MA, Donnelly JP, Verweij PE (2004) Detection of circulating galactomannan for the diagnosis and management of invasive aspergillosis. Lancet Infect Dis 4(6):349–357
Menzin J, Meyers JL, Friedman M, Perfect JR, Langston AA, Danna RP, Papadopoulos G (2009) Mortality, length of hospitalization, and costs associated with invasive fungal infections in high-risk patients. Am J Health Syst Pharm 66(19):1711–1717
Morrissey CO, Chen SC, Sorrell TC, Milliken S, Bardy PG, Bradstock KF, Szer J, Halliday CL, Gilroy NM, Moore J, Schwarer AP, Guy S, Bajel A, Tramontana AR, Spelman T, Slavin MA (2013) Galactomannan and PCR versus culture and histology for directing use of antifungal treatment for invasive aspergillosis in high-risk haematology patients: a randomised controlled trial. Lancet Infect Dis 13(6):519–528
Müllbacher A, Waring P, Tiwari-Palni U, Eichner RD (1986) Structural relationship of epipolythiodioxopiperazines and their immunomodulating activity. Mol Immunol 23(2):231–235
Pfeiffer CD, Fine JP, Safdar N (2006) Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis 42(10):1417–1427
Puri A, Ahmad A, Panda BP (2010) Development of an HPTLC-based diagnostic method for invasive aspergillosis. Biomed Chromatogr 24(8):887–892
Sugui JA, Pardo J, Chang YC, Zarember KA, Nardone G, Galvez EM, Müllbacher A, Gallin JI, Simon MM, Kwon-Chung KJ (2007) Gliotoxin is a virulence factor of Aspergillus fumigatus: gliP deletion attenuates virulence in mice immunosuppressed with hydrocortisone. Eukaryotic Cell 6(9):1562–1569
Sulahian A, Touratier S, Ribaud P (2003) False positive test for Aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N Engl J Med 349(24):2366–2367
Sun Y, Takada K, Taemoto Y, Yoshida M, Nogi Y, Okada S, Matsunaga S (2012) Gliotoxin analogues from a marine-derived fungus, Penicillium sp., and their cytotoxic and histone methyltransferase inhibitory activities. J Nat Prod 75(1):111–114
Sutton P, Waring P, Müllbacher A (1996) Exacerbation of invasive aspergillosis by the immunosuppressive fungal metabolite, gliotoxin. Immunol Cell Biol 74(4):318–322
Thornton CR (2010) Detection of invasive aspergillosis. Adv Appl Microbiol 70:187–216
Tsunawaki S, Yoshida LS, Nishida S, Kobayashi T, Shimoyama T (2004) Fungal metabolite gliotoxin inhibits assembly of the human respiratory burst NADPH oxidase. Infect Immun 72(6):3373–3382
Waring P, Eichner RD, Müllbacher A, Sjaarda A (1988) Gliotoxin induces apoptosis in macrophages unrelated to its antiphagocytic properties. J Biol Chem 263(34):18493–18499
White PL, Bretagne S, Klingspor L, Melchers WJG, McCulloch E, Schulz B, Finnstrom N, Mengoli C, Barnes RA, Donnelly JP, Loeffler J (2010) Aspergillus PCR: one step closer to standardization. J Clin Microbiol 48(4):1231–1240
White PL, Parr C, Thornton C, Barnes RA (2013) Evaluation of real-time PCR, galactomannan enzyme-linked immunosorbent assay (ELISA), and a novel lateral-flow device for diagnosis of invasive aspergillosis. J Clin Microbiol 51(5):1510–1516
White PL, Perry MD, Moody A, Follett SA, Morgan G, Barnes RA (2011) Evaluation of analytical and preliminary clinical performance of Myconostica MycAssay Aspergillus when testing serum specimens for diagnosis of invasive aspergillosis. J Clin Microbiol 49(6):2169–2174
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the local ethics committee CEICA (PI12/0041 and PI15/0197).
Funding
This work has been supported by Fondo Social Europeo (FSE/Gobierno de Aragón) and ARAID Foundation (J.P.)
Conflict of interest
M.P. Domingo, J. Pardo and E.M. Gálvez are co-inventors of a patent licensed to Blackhills Diagnostics Resources S.L. that protects the use of bmGT to diagnose IA (PCT/EP2012/058,247). All the other authors declare that they have no competing interests.
Additional information
Eva M. Gálvez and Antonio Rezusta contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Vidal-García, M., Domingo, M.P., De Rueda, B. et al. Clinical validity of bis(methylthio)gliotoxin for the diagnosis of invasive aspergillosis. Appl Microbiol Biotechnol 100, 2327–2334 (2016). https://doi.org/10.1007/s00253-015-7209-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-015-7209-6