Abstract
γ-Aminobutyric acid (GABA) has been reported to play a neurotransmitter in the central nervous system thereby exerting an inhibition in nerve impulse, in turn ameliorating depression; in addition, recent study also reveals the anti-hypertensive effect of GABA in vivo. Edible fungi of the Monascus species have been used as traditional Chinese medicine in eastern Asia for several centuries. Monascus-fermented products possess a number of functional secondary metabolites, including anti-inflammatory pigments (such as monascin and ankaflavin), monacolins, dimerumic acid, and GABA. Several scientific studies have shown that these secondary metabolites have anti-inflammatory, anti-oxidative, and anti-tumor activities. Moreover, many published reports have shown the efficacy of Monascus-fermented products in the prevention or amelioration of some diseases, including hypercholesterolemia, hyperlipidemia, hypertension, diabetes, obesity, Alzheimer’s disease, and numerous types of cancer in recent studies. The current article discusses and provides evidence to elucidate the anti-hypertensive benefit of Monascus-fermented metabolites, including anti-inflammatory pigments and GABA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is a major chronic disease and is defined as a systolic blood pressure (SBP) above 140 mmHg and/or a diastolic blood pressure (DBP) above 90 mmHg. Hypertension can result in stroke, coronary heart disease (CHD), kidney dysfunction, and disability. Moreover, other factors also lead to hypertension, including heredity, age, body weight, environment, and diet. Treatment of moderate to severe hypertension is a life-long commitment and requires drug therapy in combination with changes in lifestyle, which can include weight reduction, limitation of alcoholic intake, and reduction in salt and fat intake (Perez and Musini 2008). Study has shown that hypertension can be improved with one of several types of medications, including diuretics, β-adrenoreceptor blockers, angiotensin-converting-enzyme (ACE) inhibitors (ACEIs), calcium channel blockers, α-adrenoreceptor blockers, vasodilators, and centrally acting agents (Perez and Musini 2008).
Hypertension is a risk factor for cardiovascular diseases (CVDs). ACE mediates blood plasma, interstitial fluid volume, and arterial vasoconstriction in the rennin–angiotensin system (Imig 2004). ACEIs have beneficial effects in hypertension through inhibiting the production of the vasoconstrictor angiotensin II and degradation of the vasodilator bradykinin (Seppo et al. 2003; Chockalingam 2008 ). In recent years, there has been considerable interest in the potential for using natural food components in functional foods to treat hypertension.
Hypertension
The renin–angiotensin system is a powerful mechanism for controlling blood pressure. When blood pressure decreases, the kidneys undergo several intrinsic reactions that convert prorenin to rennin. After rennin enters the bloodstream, it hydrolyzes plasma angiotensinogen to release a peptide called angiotensin I. When angiotensin I circulates in the small vessels of the lungs, it is immediately hydrolyzed by ACE to release an 8-amino peptide, angiotensin II (Chockalingam 2008), which circulates in the blood before it is inactivated by angiotensinase. Studies have indicated that angiotensin II raises blood pressure by severely constricting the arteries, causing an increase in the peripheral resistance (Chockalingam 2008; Rizzello et al. 2008). It is also able to act on the kidneys to retain both salts and water, leading to an increase in the extracellular fluid volume and thus blood pressure. In addition, this hormone causes the adrenal glands to release aldosterone and in turn increases re-absorption of water and salt in the kidney. ACEIs also decrease the formation of angiotensin II as well as increase bradykinin, further lowering blood pressure (Chockalingam 2008; Rizzello et al. 2008) (Fig. 1).
Some foods and herbs contain natural compounds that show medicinal properties in the control of blood pressure. Indeed, a number of medications used in the treatment of blood pressure originated from foods. The mechanism by which some functional foods and nutraceuticals of a phenolic type lowers blood pressure is through the inhibition and downregulation of ACE and rennin expression (Rizzello et al. 2008).
Association between inflammatory factors and hypertension
Vessel wall inflammation and vascular endothelium activation both increase adhesion of mononuclear cells to the injured endothelial layer, and their subsequent extravasation into the vessel wall is an initial event in atherogenesis and hypertension process (Chockalingam 2008).
Elevated endothelial expression of adhesion molecules as mediators of subintimal immunocyte accumulation in atherosclerosis (Chen et al. 2006; Ross 1999) and increased oxidative stress to result in inflammatory mechanisms for the progression of atherosclerosis (Puddu et al. 2005). Inflammatory cytokine tumor necrosis factor (TNF)-α has been shown to promote the adhesion of leukocytes to endothelial cells through an oxidative stress-related mechanism in recent studies (Koga et al. 2002; Silverman et al. 2002). Moreover, transcriptional regulation involving NF–κB activation has been implicated in endothelial cells in TNF-α induction (Chen et al. 2006). Vascular cell adhesion molecule (VCAM-1) and E-selectin expression are both focally elevated in endothelial cells in vascular regions prone to atherogenesis (Ross 1999; Hofmann et al. 2001), which might reflect a link between elevated TNF-α levels and increased leukocyte infiltration in the development of atherosclerosis (Fig. 2). Recently, statins have been shown to reduce reactive oxygen species (ROS) in endothelial cells through a novel antioxidant mechanism. In this mechanism, the statin-mediated S-nitrosylation of thioredoxin enhances antioxidative activity, resulting in a significant reduction in intracellular ROS, and thereby preventing hypertension (Haendeler et al. 2004).
Roles of dyslipidemia in hypertension
Atherosclerosis is a chronic disease that involves the accumulation of lipid deposits in the arterial wall; hypercholesterolemia has been reported to promote atherosclerosis, coronary heart disease, hypertension, and stroke (Libby 2002). Although the development of CVD is associated with a number of life-style factors, as well as heredity, the most significant risk factors are related to diet. Pharmacological drug use suppresses elevations of cholesterol and triglyceride (TG), thereby preventing hypertension and CVD (Lloyd-Jones et al. 2010).
Hyperlipidemia is a major risk factor for the development of CVD and hypertension, and considerable evidence suggests that drugs with the ability to lower low-density-lipoprotein cholesterol (LDL-C) also reduce the probability of cardiovascular death, hypertension, and atherosclerosis (Fig. 2). Dairy consumption has been inversely correlated with the prevalence of overweight, hypertension, diabetes, and metabolic syndrome (Zemel 2002; Pereira et al. 2002; Choi et al. 2005).
Numerous experimental investigations in various animal models of hyperlipidemia have suggested that antioxidants have beneficial effects on lipid profiles and reduce atherosclerotic lesions (Miura et al. 2001; Hayek et al. 1997). Albeit the underlying mechanisms for the lipid-lowering effect of antioxidants are not fully elucidated, some of the evidence suggests that antioxidants reduce cholesterol absorption by lowering the solubility of cholesterol in mixed micelles, thereby preventing hypertension (Ikeda et al. 1992).
Therapy for hypertension
α- and β-Adrenoreceptor blockers
Adrenoreceptor blockers attenuate nerve impulses to the heart and blood vessels and reduce the working load of the heart by slowing the heartbeat, which results in a drop in blood pressure (Perez and Musini 2008). Adrenoreceptor blockers reduce the effect of sympathetic nerve impulses to blood vessels and thus resistance to blood flow (Perez and Musini 2008). Vasodilators relax blood vessels and lower blood pressure. For severely and moderately hypertensive patients, the use of these drugs is necessary to bring the blood pressure down to a healthy range.
ACE inhibitors
ACEIs block the formation of angiotensin II, which normally causes blood vessels to narrow, thereby increasing blood pressure (Hara et al. 1987). Some bioactive peptides have ACEI properties and can be used for preventing hypertension as well as for other therapeutic purposes (Hara et al. 1987; Li et al. 2007). Although most of the known ACEI peptides were detected in functional dairy products, some have been recently been identified and characterized from cereal proteins.
γ-Aminobutyric acid
Apart from ACEIs, γ-aminobutyric acid (GABA) has been shown to have the ability to lower blood pressure in spontaneously hypertensive rats (SHRs) and hypertensive humans. GABA is a major inhibitory neurotransmitter in the sympathetic nervous system and plays an important role in cardiovascular function. GABA has been reported to decrease blood pressure in experimental animals and in humans after oral or systemic administration (Li et al. 2007; Kajimoto et al. 2004).
Calcium channel blockers
Calcium channel blockers prevent calcium from entering the muscle cells of the heart and blood vessels, relaxing these cells and lowering the blood pressure (Perez and Musini 2008; Rizzello et al. 2008; He et al. 2002).
Sodium dietary limitation
The consumption of low- and reduced-salt foods and beverages is growing worldwide. Sodium helps to regulate fluid balance and to maintain blood volume and blood pressure. Growing evidence suggests that a higher intake of sodium than potassium is a contributing factor to hypertension (He et al. 2002).
Endothelial nitric oxide synthase activators
Nitric oxide synthase (NOS) contributes to the blood pressure-lowering activity of many commonly used medicines, nutraceuticals, and functional foods. The three major types of NOS are endothelial nitric oxide synthase (eNOS), neuronal nitric oxide synthase, and inducible nitric oxide synthase. The major function of nitric oxide (NO) is to mediate endothelium-dependent vasodilation (Furchgott and Vanhoutte 1980). NOS catalyzes the oxidation of l-arginine to l-citrulline and forms NO, a freely diffusible gas that exerts a number of physiological functions by acting as an intracellular and intercellular messenger. Endothelium-derived NO diffuses into vascular smooth muscle cells, where it subsequently activates guanylate cyclase which, in turn catalyzes the production of cyclic guanosine monophosphate (cGMP), thereby activating cGMP-dependent protein kinase (PKG) to open the K+ channel and the resulting membrane hyperpolarization to inhibit Ca2+ influx, thereby leading to vasodilation and attenuation of hypertension (Furchgott and Vanhoutte 1980). NO deficiency can lead to clinical hypertension (Furchgott and Vanhoutte 1980; Thomas et al. 2008). Moreover, eNOS knockout mice have been shown to develop mild to moderate hypertension (Huang et al. 1995).
Antioxidants and anti-inflammatory agents
Considerable epidemiological evidence reveals that antioxidant consumption reduces the risk of CVDs and total mortality (Nakachi et al. 2000; Hertog et al. 1993). In general, the mechanisms that have been suggested to explain the ability of these consumed antioxidants to prevent CHD (such as hypertension) primarily entail their powerful radical-scavenging and antioxidative properties (Rice-Evans et al. 1996).
These strong antioxidant properties may also be one explanation for the protective effect of these compounds during the development of atherosclerosis. Oxidative modification of low-density lipoprotein (LDL) is one of the critical steps in the development of atherosclerosis. A class of antioxidants known as flavonoids has been shown to inhibit LDL oxidation, possibly by reducing macrophage superoxide production (Yoshida et al. 1999), thereby preventing the formation of foam cells in atherosclerotic lesions, which results in an anti-hypertensive effect (Hayek et al. 1997; Yang and Koo 2000). On the other hand, phenolic compounds can prevent endothelial cell-mediating LDL lipid peroxidation and may accordingly inhibit heme oxygenase, an enzyme that has been linked with the transformation of monocytes into resident macrophages (Soriani et al. 1998; Wang et al. 1998).
Immune cells dominate in early atherosclerotic lesions, and their effector molecules accelerate the progression of the lesions. The resultant activation of inflammation can elicit acute coronary syndromes. Proliferation and migration of vascular smooth muscles cells from the media to the subendothelial space are major events in the development of atherosclerosis, and particularly of restenosis, after balloon angioplasty. Several lines of evidence demonstrate that components in tea interfere with these processes of proliferation and migration. Antioxidants have been suggested to play an important role as well in modulating the expression of adhesion molecules in endothelial cells (Murase et al. 1999).
Functions of Monascus-fermented products
Prevention of hypertension through Monascus-fermented products
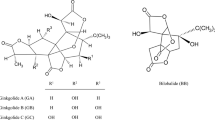
Monascus was classified and named in 1884 by French scientist van Tieghem (van Tieghem 1884). The genus Monascus belongs to the family Monascaceae, order Eurotiales, class Ascomycetes, phylum Ascomycota, and kingdom Fungi. To date, 58 Monascus strains have been deposited in the American Type Culture Collection. However, based on Hawksworth and Pit (1983), most strains belong to only three species: Monascus pilosus, Monascus purpureus, and Monascus ruber. Monascus-fermented products, especially those produced by solid-state rice fermentation, have been used as food colorants and dietary material for more than 1,000 years. In Asian countries, Monascus-fermented rice is both common in the diet and used in traditional health remedies. Monascus-fermented rice contains various chemical components, some of which have been purified and identified, including monacolin K (Fig. 3a), GABA (Fig. 3b), different pigments, and dimerumic acid (Fig. 3c). Their bioactive functions have recently been discovered.
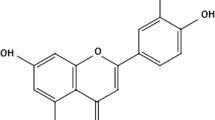
Monascus pigments are widely studied, and eight types of chemical structures have been identified (Martinkova et al. 1995). These structures can be divided into red pigments (monascorubramine and rubropunctamine), orange pigments (monascorubrin and rubropunctatin), and yellow pigments (yellow II, xanthomonascin A, monascin (Fig. 3d), and ankaflavin (Fig. 3e)). The orange pigments have been found to possess antibiotic activities against bacteria, yeast, and filamentous fungi (Martinkova et al. 1999) and to inhibit the growth of Bacillus subtilis and Candida pseudotropicalis. Yellow pigments such as monascin and ankaflavin have been shown to have immunosuppressive activities against mouse T splenocytes (Martinkova et al. 1999).
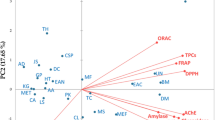
Effects of Monascus-fermented products on the inhibition of serum hyperlipidemia and the prevention of atherosclerosis
The oral administration of a powder derived from Monascus-fermented products has been reported to decrease total cholesterol (TC), TG, and LDL-C levels in a hyperlipidemia hamster model (Lee et al. 2006a). Our laboratory has further found that Monascus-fermented dioscorea shows a more significant hypolipidemic effect than traditional Monascus-fermented rice. This effect may be explained by the higher monascin and/or ankaflavin levels in the Monascus-fermented dioscorea (Lee et al. 2007). In addition, the anti-oxidative activities of Monascus-fermented dioscorea provided by various Monascus metabolites (e.g., dimerumic acid, tannins, and phenols) show greater anti-atherosclerotic effects than the anti-oxidative activities of Monascus-fermented rice and include increased total antioxidant status and catalase levels, and superoxide dismutase activity and the repression of lipid peroxidation and atherosclerotic plaques (Lee et al. 2007). In addition, Monascus-fermented products were able to significantly inhibit atherosclerotic plaque formation in the heart aorta of high-cholesterol diet-induced hamsters (Fig. 4) (Lee et al. 2010).
Effect of Monascus-fermented products (monascin, ankaflavin, and monacolin K) on the atherosclerotic plaque in the heart aorta of hyperlipidemic hamsters: a atherosclerotic plaque presented as the red dye in the graph; b proportion of the area of the atherosclerotic plaque in the aorta. Hamsters were fed a normal diet (NOR group) or a high-cholesterol diet (HC group) without the administration of test materials, respectively. Hyperlipidemic hamsters were administered monacolin K (1.56 mg/kg/day) (MK group), monascin (5.30 mg/kg/day) (MS group), ankaflavin (0.77 mg/kg/day) (AF group), 0.5-fold dose of Monascus-fermented dioscorea (RMD; 53.92 mg/kg/day including 0.16 mg of monacolin K, 0.53 mg of monascin, and 0.08 mg of ankaflavin), a onefold dose of RMD (107.83 mg/kg/day including 0.31 mg of monacolin K, 1.06 mg of monascin, and 0.15 mg of ankaflavin), a twofold dose of RMD (215.66 mg/kg/day including 0.62 mg of monacolin K, 2.12 mg of monascin, and 0.31 mg of ankaflavin), or fivefold dose of RMD (539.15 mg/kg/day including 1.56 mg of monacolin K, 5.30 mg of monascin, and 0.77 mg of ankaflavin) (Lee et al. 2010)
Elevation of high-density lipoprotein cholesterol by Monascus-fermented products
Furthermore, animal studies have been conducted to explore the anti-obesity effects of Monascus-fermented rice. We found that supplementation with Monascus-fermented rice significantly reduced serum TC, serum LDL-C, the ratio of LDL-C to high-density lipoprotein cholesterol (HDL-C), and serum insulin. The study revealed for the first time that Monascus-fermented rice can prevent body fat accumulation and improve dyslipidemia. The anti-obesity effects of Monascus-fermented rice were mainly derived from its lipolytic activity and mild anti-appetite potency (Lee et al. 2010; Chen et al. 2008). Furthermore, monascin and ankaflavin were shown to elevate serum HDL-C levels in high-cholesterol diet-induced hamsters in a recent study (Lee et al. 2010).
GABA and ACEIs in Monascus-fermented products regulate blood pressure in SHR rats
The antihypertensive function of Monascus-fermented rice has been previously shown (Brown and Vaughan 1998; Wang et al. 2010). In addition, the regulation of blood pressure by Monascus-fermented products in high-fructose-induced metabolic syndrome in rats has been reported (Hsieh and Tai 2003). Recent research has focused on the effects of the oral administration of a small amount of Monascus-fermented dioscorea, as fermented by M. purpureus NTU 568, on the SBP, DBP, heart rate, and the aorta in hypertensive rats (Fig. 5) (Wu et al. 2009). Monascus-fermented dioscorea significantly prevented increases in blood pressure and improved vascular elastin remodeling (Fig. 6). The anti-hypertensive effect as well of Monascus-fermented dioscorea was better than that of Monascus-fermented rice. Moreover, Monascus-fermented dioscorea exhibited higher ACEI activity than Monascus-fermented rice, thereby preventing hypertension (Wu et al. 2009). In addition, the elastin fibers in the aortas of SHRs fed the Monascus-fermented products were significantly straighter than those of the controls (Fig. 6) (Wu et al. 2009).
Effect of single oral administration of Monascus-fermented products on a SBP and b DBP in SHRs. One group of the SHRs were fed a normal diet without the administration of test materials (the control group; filled circle). The other SHRs were administrated with a onefold dose of unfermented dioscorea (150 mg/kg/day) (the D-1X group; inverted filled triangle), GABA (0.245 mg/kg/day) (the GABA-1X group; empty circle), a onefold dose of Monascus-fermented rice (150 mg/kg/day including 0.0197 mg of GABA) (the RMR-1X group; inverted empty triangle), and a onefold dose of Monascus-fermented dioscorea (150 mg/kg/day including 0.0245 mg of GABA) (the RMD-1X group; filled square) (Wu et al. 2009)
Microscopic examination (×100 and ×400) of aorta thin section on experimental SHRs: a control group, b D-1X group, c GABA-1X group, d RMR-1X group, e RMD-0.5X group, f RMD-1X group, and g RMD-5X group (Wu et al. 2009)
Other Monascus strain-fermented products are also evaluated for attenuating hypertension in various models (Table 1).
Chronic hypertension is associated with structural changes in the resistance vasculature (Mulvany 2000). Histopathological changes, known as “remodeling,” represent a complex process that may increase (hypertrophy), decrease (hypotrophy), or rearrange (eutrophy) the vascular wall (Mulvany 2000). Elastin fiber is an important determinant of arterial distensibility (Dobrin 1978). Several models of genetic hypertension have reported abnormalities in the elastin content and structure in large arteries (Boumaza et al. 2001). Monascus-fermented products can prevent the rearrangement of the vascular wall; therefore, they may have a hypotensive effect that results from a decrease in the peripheral vascular resistance.
Kohama et al. (1987) found that GABA and acetylcholine chloride were the major compounds in Monascus-fermented products that can lower blood pressure. Acetylcholine acts on a muscarinic receptor of endothelial cells to stimulate the release of a substance that causes relaxation of vascular smooth muscle, resulting in systemic hypotension (Kohama et al. 1987). However, acetylcholine acts only transiently and is easily hydrolyzed by cholinesterase in the body (Kohama et al. 1987). Other studies indicate that beni-food (Monascus-fermented food), such as beni-bread, beni-miso, beni-soy sauce, and beni-somen, has a hypotensive effect (Tsuji et al. 1992, 1993). Moreover, a water-soluble extract of Monascus-fermented product showed the ability to lower blood pressure (Tsuji et al. 1992, 1993).
Anti-inflammation activities of Monascus-fermented products
The arterial and cardiopulmonary baroreceptors are the two most important neural reflex arches associated with the regulation of blood pressure. The aortic baroreceptors lower blood pressure both through parasympathetic activation and sympathetic inhibition. When the afferent signals from the baroreceptors enter the vasomotor center in the medulla of the brain, the efferent signals are transferred via sympathetic nerves to the heart, vasculature, and kidneys (Grassi et al. 1998). Monascus pigments have been reported to have hypotensive ability (Tsuji et al. 1992, 1993). We found that Monascus-fermented dioscorea has a stronger hypotensive effect than Monascus-fermented rice because of the higher levels of monascin and ankaflavin (anti-inflammatory agents) in the Monascus-fermented dioscorea (Wu et al. 2009).
The expression of intercellular adhesion molecule-1 (ICAM-1), VCAM-1, and E-selectin is focally elevated in endothelial cells in vascular regions prone to atherogenesis (Ross 1999). Dietary supplementation with Monascus-fermented products may be a potential means to attenuate TNF-α-stimulated activation of the endothelium and may help reduce the risk of vascular disease associated with inflammation (Lin et al. 2011).
Moreover, monacolin K, ankaflavin, and monascin from Monascus-fermented rice were investigated for their effects on the expression of cell adhesion molecules (ICAM-1, VCAM-1, and E-selectin) in TNF-α-treated human aortic endothelial cells (HAECs). The expression of VCAM-1 and E-selectin were significantly elevated by TNF-α stimulation; furthermore, this elevation could be suppressed by various Monascus-fermented rice metabolite supplements, suggesting that endothelial VCAM-1 and E-selectin expression, rather than ICAM-1 expression, was more critical to monocyte adhesion in this in vitro model. In addition, supplementing the HAECs with these Monascus-fermented rice metabolites significantly suppressed cellular binding between human U937 monocytic cells and TNF-α-stimulated HAECs, suggesting Monascus-fermented rice metabolites may decrease TNF-α-induced endothelial adhesiveness to monocytes, thereby attenuating aortic endothelial cell inflammation and preventing hypertension (Lin et al. 2011).
Furthermore, Monascus-fermented rice metabolites also attenuated ROS generation in vitro and in TNF-α-treated HAECs (Lin et al. 2011). These health-promoting functions of Monascus metabolites could be used to augment the antihypertensive and antiatherogenic effects of Monascus-fermented products.
eNOS activation by Monascus-fermented products
Study has shown antioxidants promoting eNOS expression in endothelial cells via a p38 MAPK-estrogen receptor alpha-dependent pathway (Anter et al. 2005). We showed that monascin and ankaflavin both activated eNOS expression and increased NO production in human umbilical vein endothelial cells (HUVECs) and prevented a decrease in eNOS expression in TNF-α-induced HUVECs (Hsu et al. 2012) (Fig. 7). In addition, both compounds attenuated TNF-α induction of NF–κB activation and suppressed the expression of adhesion factors, including E-selectin and VCAM-1 (Hsu et al. 2012) (Fig. 8).
The preventive effect of ankaflavin and monascin (20 μM) on TNF-α induced a decrease in eNOS expression of HUVECs for 12 h treatment. (#) Significantly different from control group at p < 0.05; (*) significantly different from TNF-α-treated group at p < 0.05 (Hsu et al. 2012)
The inhibitory effects of ankaflavin and monascin (20 μM) on VCAM-1 and E-selectin in HUVECs treatment with 10 ng/mL of TNF-α for 12 h measuring by RT-PCR (a). The levels of VCAM-1 (b) and E-selectin (c) mRNA expression in HUVECs measuring by real-time PCR. (#) Significantly different from control group at p < 0.05; (*) significantly different from TNF-α- treated group at p < 0.05 (Hsu et al. 2012)
In this review, we discussed the potential mechanism for improving hypertension in vitro and in vivo (Fig. 9), including anti-inflammation and NO elevation by Monascus-fermented products and downregulation of hypertension by GABA.
ACEI and GABA production by Monascus fermentation
We have reported that 0.3 % ethanol supplement can promote GABA production by response surface methodology investigation (Wang et al. 2003). In addition, Monascus-fermented dioscorea can produce larger amounts of monascin and ankaflavin than Monascus-fermented rice (Lee et al. 2006b).
Conclusions
Hypertension, commonly recognized as a silent killer, is the most common CVD and is a major risk factor for atherosclerosis, metabolic syndrome, renal dysfunction, myocardial infarction, heart attack, and stroke, which are the most important causes of death in industrialized countries. However, Monascus-fermented products (including monascin, ankaflavin, and GABA) can inhibit inflammation, suppress atherosclerosis, promote eNOS, and improve dyslipidemia and blood pressure regulation, thereby preventing hypertension.
References
Anter E, Chen K, Shapira OM, Karas RH, Keaney JF Jr (2005) P38 mitogen-activated protein kinase activates eNOS in endothelial cells by an estrogen receptor alpha-dependent pathway in response to black tea polyphenols. Circ Res 96:1072–1078
Boumaza S, Arribas SM, Osborne-Pellegrin M, McGrath JC, Laurent S, Lacolley P, Challande P (2001) Fenestrations of the carotid internal elastic lamina and structural adaptation in stroke-prone spontaneously hypertensive rats. Hypertens 37:1101–1107
Brown NJ, Vaughan DE (1998) Angiotensin-converting enzyme inhibitors. Circ 97:1411–1420
Chen YH, Lin SJ, Chen YL, Liu PL, Chen JW (2006) Anti-inflammatory effects of different drugs/agents with antioxidant property on endothelial expression of adhesion molecules. Cardiovasc Hematol Disord Drug Targets 6:279–304
Chen WP, Ho BY, Lee CL, Lee CH, Pan TM (2008) Red mold rice prevents the development of obesity, dyslipidemia and hyperinsulinemia induced by high-fat diet. Int J Obes 32:1694–1704
Chockalingam A (2008) World hypertension day and global awareness. Can J Cardiol 24:441–444
Choi HK, Willett WC, Stampfer MJ, Rimm E, Hu FB (2005) Dairy consumption and risk of type 2 diabetes mellitus in men: a prospective study. Arch Intern Med 165:997–1003
Dobrin PB (1978) Mechanical properties of arteries. Physiol Rev 58:397–460
Furchgott RF, Vanhoutte PM (1980) Endothelium-derived relaxing and contracting factors. FASEB J 3:2007–2017
Grassi G, Cattaneo BM, Seravalle G, Lanfranchi A, Mancia G (1998) Baroreflex control of sympathetic nerve activity in essential and secondary hypertension. Hypertens 31:68–72
Haendeler J, Hoffmann J, Zeiher AM, Dimmeler S (2004) Antioxidant effects of statins via S-nitrosylation and activation of thioredoxin in endothelial cells: a novel vasculoprotective function of statins. Circ 110:856–861
Hara Y, Matsuzaki T, Suzuki T (1987) Angiotensin I converting enzyme inhibiting activity of tea components. Nippon Nogeikagaku Kaishi 61:803–808
Hawksworth DL, Pit JI (1983) A new taxonomy for Monascus species based on cultural and micros Hawksworth copical characters. Aust J Bot 31:51–61
Hayek T, Fuhrman B, Vaya J, Rosenblat M, Belinky P, Coleman R, Elis A, Aviram M (1997) Reduced progression of atherosclerosis in apolipoprotein E-deficient mice following consumption of red wine, or its polyphenols quercetin or catechin, is associated with reduced susceptibility of LDL to oxidation and aggregation. Vasc Biol 17:2744–2752
He FJ, MacGregor GA (2002) Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 16:761–770
Hertog MG, Feskens EJ, Hollman PC, Katan MB, Kromhout D (1993) Dietary antioxidant flavonoids and risk of coronary heart diesase: the Zutphen Elderly Study. Lancet 342:1007–1011
Hofmann MA, Lalla E, Lu Y, Gleason MR, Wolf BM, Tanji N (2001) Hyperhomocysteinemia enhances vascular inflammation and accelerates atherosclerosis in a murine model. J Clin Invest 107:675–683
Hsieh PS, Tai YH (2003) Aqueous extract of Monascus purpureus M9011 prevents and reverses fructose-induced hypertension in rats. J Agric Food Chem 51:3945–3950
Hsu WH, Lee BH, Lu IJ, Pan TM (2012) Ankaflavin and monascin regulate endothelial adhesion molecules and endothelial NO synthase (eNOS) expression induced by tumor necrosis factor-α (TNF-α) in human umbilical vein endothelial cells (HUVECs). J Agric Food Chem 60:1666–1672
Huang PL, Huang ZH, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC (1995) Hypertension in mice lacking the gene for endothelia metric oxide synthase. Nature 377:239–242
Ikeda I, Imasato Y, Sasaki E, Nakayama M, Nagao H, Takeo T, Yayabe F, Sugano M (1992) Tea catechins decrease micellar solubility and intestinal absorption of cholesterol in rats. Biochim Biophys Acta 1127:141–146
Imig JD (2004) ACE inhibition and bradykinin-mediated renal vascular responses: EDHF involvement. Hypertens 43:533–535
Kajimoto O, Hirata H, Nakagawa S, Kajimoto Y, Hayakawa K, Rimura M (2004) Hypotensive effect of fermented milk containing γ-aminobutyric acid (GABA) in subjects with high normal blood pressure. Nippon Shokuhin Kogaku Kaishi 51:79–86
Koga T, Claycombe K, Meydani M (2002) Homocysteine increases monocyte and T-cell adhesion to human aortic endothelial cells. Atheroscler 161:365–374
Kohama Y, Matsumoto S, Mimura T, Tanbe N, Inada A, Nakanishi T (1987) Isolation and identification of hypotensive principles in red-mold rice. Chem Pharm Bull 35:2484–2489
Lee CL, Tsai TY, Wang JJ, Pan TM (2006a) In vivo hypolipidemic effects and safety of low dosage Monascus powder in a hamster model of hyperlipidemia. Appl Microbiol Biotechnol 70:533–540
Lee CL, Wang JJ, Kuo SL, Pan TM (2006b) Monascus fermentation of dioscorea for increasing the production of cholesterol-lowering agent-monacolin K and antiinflammation agent-monascin. Appl Mirobiol Biotechnol 72:1254–1262
Lee CL, Hung HK, Wang JJ, Pan TM (2007) Red mold dioscorea has greater hypolipidemic and antiatherosclerotic effect than traditional red mold rice and unfermented dioscorea in hamsters. J Agric Food Chem 55:7162–7169
Lee CL, Kung YH, Wu CL, Hsu YW, Pan TM (2010) Monascin and ankaflavin act as novel hypolipidemic and high-density lipoprotein cholesterol-raising agents in red mold dioscorea. J Agric Food Chem 58:9013–9019
Li GH, Qu MR, Wan JZ, You JM (2007) Antihypertensive effect of rice protein hydrolysate with in vitro angiotensin I-converting enzyme inhibitory activity in spontaneously hypertensive rats. Asia Pacific J Clin Nutr 16:275–280
Libby P (2002) Inflammation in atherosclerosis. Nature 420:868–874
Lin CP, Lin YL, Huang PH, Ysai HS, Chen YH (2011) Inhibition of endothelial adhesion molecule expression by Monascus purpureus-fermented rice metabolites, monacolin K, ankaflavin, and monascin. J Sci Food Agric 91:1751–1758
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M (2010) Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circ 121:948–954
Martinkova L, Juzlova P, Vesely D (1995) Biological activity of polyketide pigments produced by the fungus Monascus. J Appl Bacteriol 79:609–616
Martinkova L, Patakova-Juzlova P, Kren V, Kucerova Z, Havlicek V, Olsovsky P, Hovorka O, Rihova B, Vesely D, Vesela D, Ulrichova J, Prikrylova V (1999) Biological activities of oligoketide pigments of Monascus purpureus. Food Addit Contam 16:15–24
Miura Y, Chiba T, Tomita I, Koizumi H, Umeqaki K, Hara Y, Ikeda M, Tomita T (2001) Tea catechins prevent the development of atherosclerosis in apoprotein E-deficient mice. J Nutr 131:27–32
Mulvany MJ (2000) Small artery remodeling in hypertension. Curr Hypertens Rep 4:49–55
Murase T, Kume N, Hase T, Shibuya Y, Nishizawa Y, Tokimitsu I, Kita T (1999) Gallates inhibit cytokine-induced nuclear translocation of NF-kappaB and expression of leukocyte adhesion molecules in vascular endothelial cells. Thromb Vasc Biol 19:1412–1420
Nakachi K, Matsuyama S, Miyake S, Suganuma M, Imai K (2000) Preventive effects of drinking green tea on cancer and cardiovascular disease: epidemiological evidence for multiple targeting prevention. Biofactors 13:49–54
Pereira MA, Jacobs DR, Van Horn L, Slattery ML (2002) Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. J Am Med Assoc 287:2081–2089
Perez MI, Musini VM (2008) Pharmacological interventions for hypertensive emergencies: a Cochrane systematic review. J Hum Hypertens 22:596–607
Puddu GM, Cravero E, Arnone G, Muscari A, Puddu P (2005) Molecular aspects of atherogenesis: new insights and unsolved questions. J Biomed Sci 12:839–853
Rice-Evans CA, Miller NJ, Paganga G (1996) Structure-antioxidant activity relationships of flavonoids and phenolic acids. Free Radic Biol Med 20:933–956
Rizzello CG, Cassone A, Di Cagno R, Gobbetti M (2008) Synthesis of angiotensin I-converting enzyme (ACE)-inhibitory peptides and γ-aminobutyric acid (GABA) during sourdough fermentation by selected lactic acid bacteria. J Agric Food Chem 56:6936–6943
Ross R (1999) Atherosclerosis: an inflammatory disease. N Engl J Med 340:115–126
Seppo L, Jauhiainen T, Poussa T, Korpela R (2003) A fermented milk high in bioactive peptides has a blood pressure-lowering effect in hypertensive subjects. Am J Clin Nutr 77:326–330
Silverman MD, Tumuluri RJ, Davis M, Lopez G, Rosenbaum JT, Lelkes PI (2002) Homocysteine upregulates vascular cell adhesion molecule-1 expression in cultured human aortic endothelial cells and enhances monocyte adhesion. Arterioscler Thromb Vasc Biol 22:587–592
Soriani M, Rice-Evans C, Tyrrell RM (1998) Modulation of the UVA activation of haem oxygenase, collagenase and cyclooxygenase gene expression by epigallocatechin in human skin cells. FEBS Lett 439:253–257
Thomas GD, Zhang W, Victor RG (2008) Nitric oxide deficiency as a cause of clinical hypertension. J Am Med Assoc 285:2055–2057
Tsuji K, Ichikawa T, Tanabe N, Abe S, Tarui S, Nakagawa Y (1992) Effect of beni-koji foods on blood pressure in spontaneously hypertensive rats. Nippon Shokuhin Kogyo Gakkaishi 39:919–924
Tsuji K, Nakagawa Y, Ichikawa T (1993) Effect of beni-koji extracts and pigment produced by Monascus spp. on blood pressure, mineral balance and cholesterol levels in spontaneously hypertensive rats. Nihon Kasei Gakkai Shi 44:109–114
van Tieghem M (1884) Monascus genre nouvear de l‘ondre des Ascomycetes. Bull Soc Bot Fr 31:226–231
Wang LJ, Lee TS, Lee FY, Pai RC, Chau LY (1998) Expression of heme oxygenase-1 in atherosclerotic lesions. Am J Pathol 152:711–720
Wang JJ, Lee CL, Pan TM (2003) Improvement of monacolin K, γ-aminobutyric acid and citrinin production ratio as a function of environmental conditions of Monascus purpureus NTU 601. J Ind Microbiol Biotechnol 30:669–676
Wang JJ, Wang HY, Shih CD (2010) Autonomic nervous system and nitric oxidein antihypertensive and cardiac inhibitory effects induced by red mold rice in spontaneously hypertensive rats. J Agric Food Chem 58:7940–7948
Wu CL, Lee CL, Pan TM (2009) Red mold dioscorea has a greater antihypertensive effect than traditional red mold rice in spontaneously hypertensive rats. J Agric Food Chem 57:5035–5041
Yang TT, Koo MW (2000) Inhibitory effect of Chinese green tea on endothelial cell-induced LDL oxidation. Atheroscler 148:67–73
Yoshida H, Ishikawa T, Hosoai H, Suzukawa M, Hisada T, Sawada S, Yonemura A, Higashi K, Ito T, Nakajima K, Yamashita T, Tomiyasu K, Nishiwaki M, Ohsuzu F, Nakamura H (1999) Inhibitory effect of tea flavonoids on the ability of cells to oxidize low density lipoprotein. Biochem Pharmacol 58:1695–1703
Zemel MB (2002) Regulation of adiposity and obesity risk by dietary calcium: mechanisms and implications. J Am Coll Nutr 21:146–151
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, BH., Pan, TM. Benefit of Monascus-fermented products for hypertension prevention: a review. Appl Microbiol Biotechnol 94, 1151–1161 (2012). https://doi.org/10.1007/s00253-012-4076-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-012-4076-2