Abstract
Background
Little attention has been given to the sonographic appearances of the epididymis in testicular torsion.
Objective
To describe the position and morphology of the epididymis in childhood acute testicular torsion when testicular flow is present on color Doppler sonography.
Materials and methods
We studied the sonographic findings in boys with clinically and surgically proven acute testicular torsion who were examined sonographically from May 2013 to May 2014 and who had preserved intratesticular flow on color Doppler sonography. We retrospectively evaluated the sonograms with emphasis on the epididymal findings.
Results
In all nine boys with confirmed torsion but with preserved intratesticular flow on color Doppler sonography, the epididymal head had an unexpected configuration and size, and no close relationship with the upper pole of the testis. In five of these children the spermatic cord appeared twisted on the affected side. In the remaining four boys the spermatic cord appeared straight.
Conclusion
The position and morphology of the head of the epididymis were abnormal in all boys with acute testicular torsion but with preserved testicular flow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In pediatric emergency departments acute scrotum is common [1]. In children, torsion of testicular appendages, testicular torsion and inflammatory diseases are the main causes of acute scrotum [2]. Their differential diagnosis is very important because management of acute scrotum differs according to its etiology. Urgent surgical exploration is indicated in testicular torsion; however clinical distinction of testicular torsion from epididymitis and torsion of the testicular appendix is often not easy [1].
Color Doppler sonography remains the imaging modality of choice [3–5]. Absent or decreased flow of the affected testis is the diagnostic finding of torsion on color Doppler sonography [6]. However, presence of flow on color Doppler can be misleading, especially in cases of partial torsion [6, 7].
The abnormal course and rotation of the spermatic cord has been reported to be a highly sensitive sonographic sign in the diagnosis of torsion, especially in the presence of testicular flow on color Doppler sonography [8, 9]. No emphasis has been given in the literature, however, to the diagnosis of torsion in the presence of testicular flow with visualization of a straight-looking spermatic cord. In these cases the morphology and position of the head of the epididymis may play a definitive role. In our experience normally the head of the epididymis is shown sonographically to cover a large part of the upper pole of the testis. The body and the tail are visualized posterolateral to the body of the testis. The head of the epididymis appears with a triangular or crescent shape. Its echogenicity is similar to that of the testicular parenchyma. We have observed that the crescent shape is more common in the right scrotum. Other studies have described the shape of the normal head of the epididymis [7, 10, 11].
We describe the sonographic findings in nine boys with testicular torsion and preserved testicular flow — five with a rotated spermatic cord and four with a straight-looking cord — emphasizing the abnormal appearance of the head of the epididymis in all nine children.
Materials and methods
In this retrospective study we included boys with clinically and surgically proven acute testicular torsion who had been examined by US in our department from May 2013 to May 2014; inclusion criteria included having symmetrical or slightly diminished intratesticular flow on the affected side compared with the normal testis on color Doppler sonography. We present these boys with acute testicular torsion but preserved blood flow in order to demonstrate some less-recognized diagnostic findings on gray-scale US, such as abnormal epididymis and abnormal course of the spermatic cord, with emphasis on the epididymal findings. Sonograms in these boys were performed and were re-evaluated by two highly experienced pediatric radiologists independently (P.G. and V.D., with 10 and 15 years of experience in pediatric sonography, respectively).
This retrospective study was approved by the ethics committee of our hospital. The boys had been referred to our department by pediatric surgeons because of acutely painful scrotum with duration of persistent pain <24 h (4–18 h). All scrotal sonograms except one were performed on the same US scanner (Logic 7; GE Healthcare, Tokyo, Japan); the other was performed on a Philips ATL (Royal Philips Electronics, Amsterdam, the Netherlands) scanner. A high-frequency linear transducer was used for all scrotal sonograms.
Sonographic studies were performed using a standardized method. Gray-scale longitudinal and transverse scans of both testicles were obtained and evaluated for echogenicity, size and morphology. Color or power Doppler US was performed for the evaluation of parenchymal flow. The same color Doppler parameters were chosen for the comparison of both sides. The parameters were adjusted at the lowest velocity flow in order to minimize artifacts on the background, as well as at low pulse repetition frequency (PRF), color gain settings of 80–90% and low wall filter. Parenchymal flow was evaluated as normal when central and peripheral vessels were detectable and symmetrical.
The epididymis was examined for its position in relation to the testis and spermatic cord and for its morphology with a standardized method. Initially the head of the epididymis was examined in a sagittal plane with the probe parallel to the long axis of the testis on the anterior surface of the scrotum (Fig. 1). Then the probe was moved slowly laterally to the testis and the rest of the epididymis was evaluated in an oblique coronal plane. This technique was modified in cases of a tilted testis so that the longitudinal scans referred to the long axis of the rotated testis. The position, shape, size, echogenicity and vascularity of the epididymis were compared to those of the contralateral side. Lateral, cephalic or caudal displacement of the head of the epididymis in relation to the upper pole of the testis, with or without interposing spermatic cord, resulting in either non-visualization of the head or visualization of a small part of it, was evaluated as indicative of acute testicular torsion.
Normal testicular morphology in two 12 year-old boys ( a, b) and in a 15 year-old boy (c). a, b Sagittal US image with the probe on the anterior surface of the scrotum and parallel to the longitudinal axis of the testis shows normal morphology and position of the head of the epididymis, with its triangular shape covering a large proportion of the upper pole of the testis. c Sagittal US shows normal morphology and position of the head of the epididymis with a crescent shape covering most of the upper pole of the testis
The spermatic cord was demonstrated with an initial scan of the anterior surface of the scrotum in a sagittal plane, then the posterolateral surface in an oblique coronal plane, from the inguinal canal to the posterior aspect of the testis. Its size, course and vascularity were compared to those of the contralateral side. Any abrupt changes in the straight tubular shape of the cord cephalad, caudal or lateral to the testis were considered abnormal and indicative of torsion.
Spectral analysis of the Doppler waveform in the parenchyma of the affected testis was documented only in two boys.
Results
In nine boys, ages 11–15 years (mean 13 years) the sonographic diagnosis of testicular torsion was made despite the presence of intratesticular flow on color Doppler sonography. In all of the boys, the epididymal head did not have the expected configuration, size and close relationship with the upper pole of the testis. Based on the abnormal gray-scale findings and the presence of acute scrotal pain, the diagnosis of testicular torsion was highly suggested, and all nine boys were treated with open or closed detorsion. In five out of the nine boys the spermatic cord appeared twisted on the affected side. In this group testicular torsion was verified at surgery in four boys, whereas in the fifth child the diagnosis was confirmed clinically, because three successful manual maneuvers resulted in detorsion, which was confirmed clinically by immediate pain relief and sonographically by normal findings. Surgical fixation of the still-viable testis followed.
In the remaining four of the nine children the spermatic cord appeared straight and torsion was sonographically suggested based only on the abnormal position and morphology of the head of the epididymis in regard with the upper pole of the testis. Three of those four boys had been proved at surgery to have partial torsion; one was considered to have transient torsion because spontaneous detorsion was observed during the performance of the sonogram, with immediate relief from pain and hyperemia of the affected testis and epididymis. The testis and epididymis were normal on the sonogram obtained the following day and the boy was completely asymptomatic.
In all nine boys the epididymal head had an unexpected configuration and size, and no close relationship with the upper pole of the testis.
Abnormal configuration and displaced position of the head of the epididymis were the only sonographic findings indicative of torsion in four of the nine boys; no other color Doppler or morphological spermatic cord abnormality was noted in these four boys.
In two of these four boys, the head of the epididymis was laterally displaced and was not visualized at the upper pole of the testis in the sagittal plane. In the oblique coronal plane the body of the epididymis was revealed without flow or edema laterally to the testis and parallel to a straight-looking spermatic cord. Reactive hydrocele was shown at the top of the testis (Fig. 2). Similar intratesticular flow to that of the normal testis was shown.
US scans in patient 1, a 12-year-old boy with 6 h of acute left testicular pain. a Transverse plane shows the left testis with centripetal vascularity and normal size and echogenicity. b Sagittal plane with the probe on the anterior surface of the scrotum and parallel to the longitudinal axis of the testis. In this image the epididymal head is not visualized at the upper pole of the testis; reactive hydrocele is shown. c Oblique coronal plane laterally to the testis shows the spermatic cord with no rotation (small arrow). The epididymis is clearly distinguishable without edema (large arrow). At surgery, 180° torsion was revealed
In one boy, lateral displacement of the head of the epididymis was revealed with visualization of a small triangular part of it at the top of the testis, smaller than half of the size of the contralateral epididymis in the sagittal plane. In the oblique coronal plane the body of the epididymis was revealed without flow or edema laterally to the testis and parallel to a straight-looking spermatic cord (Fig. 3). Similar intratesticular flow to that of the normal testis was present.
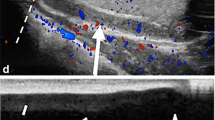
US scans in patient 2, a 12-year-old boy with 6 h of acute left testicular pain. a, b Sagittal plane with the probe on the anterior surface of the scrotum and parallel to the longitudinal axis of the testis shows similar intratesticular flow in the right (a) and left (b) testicles. c Sagittal plane with the probe on the anterior surface of the scrotum shows the course of the spermatic cord, with no rotation (arrow). d Sagittal plane with the probe on the anterior surface and parallel to the longitudinal axis of the testis shows the head of the epididymis with a small triangular shape at the top of the testis (arrow) caused by its lateral displacement. Compare with the normal triangular head of the epididymis in Fig. 1a. At surgery, 180° torsion of the left testis was documented
In one boy the head of the epididymis was shown to be caudally displaced with no flow and enlarged in the sagittal plane. There was no abnormal, twisted, echogenic and enlarged spermatic cord interposed between the epididymal head and the testis, in which the flow was slightly decreased. During the exam the head of the epididymis returned to normal position by 180°. Immediate increase of flow was detected in the head of the epididymis and in the parenchyma of the testis, and the boy was instantly relieved of pain (Fig. 4). We observed no enlargement of the affected testis, and we also noted homogeneity of the testicular parenchyma compared to the healthy side in all four boys.
US scans in patient 3, an 11-year-old boy with 4 h of sudden-onset acute left testicular pain. a Sagittal plane with the probe on the anterior surface of the scrotum and parallel to the long axis of the testis shows the head of the epididymis infratesticularly, swollen and with no vascularity (arrow). Flow of the testis is visualized. b Oblique coronal plane posterior to the testis shows the course of the spermatic cord, with no rotation (arrow) c Sagittal plane with the probe on the anterior surface of the scrotum and parallel to the long axis of the testis 4 min into the exam shows the head of the epididymis cephalad, in normal position and with flow. The perfusion of the testis is also increased. The boy was relieved of the pain simultaneously
In two of these boys complementary spectral Doppler sonography was performed. It was helpful only in one boy, in whom a relatively decreased arterial flow pattern was detected in the affected testis, as compared with the normal side.
Table 1 summarizes the sonographic findings of the abnormal epididymis in the four boys with intratesticular flow on color Doppler sonography and straight-looking spermatic cord. The outcome of each case is also reported.
In the remaining five boys with intratesticular flow on color Doppler sonography, abnormal configuration and position of the head of the epididymis and rotated spermatic cord were the main sonographic findings.
In one of these five boys, the head of the epididymis was demonstrated posterolateral to the rotated testis, with interposing echogenic and enlarged twisted spermatic cord between the head and the testis, in the oblique coronal plane. When the probe was moved caudally and more laterally to the testis the body and the tail of epididymis were also visualized above the twisted cord. The epididymis was enlarged in its full length and with no flow. Slightly decreased flow was shown in the testis, whose anteroposterior (AP) diameter exceeded that of the normal testis by 4 mm (Fig. 5).
US scans in patient 5, a 15-year-old boy with 10 h of sudden-onset acute right testicular pain. a Oblique coronal scan posterolaterally to the testis shows the epididymal head (large arrow), which is not at the upper pole of the testis but cephalad to the twisted spermatic cord (small arrow). b Oblique coronal scan more caudally shows the body and tail of epididymis (large arrow) above the twisted cord (small arrow). The epididymis is enlarged in its full length, heterogeneous and with no flow. The 540° of torsion was manually detorsed with three successful maneuvers. c Sagittal scan after the second maneuver shows the head of the epididymis curved close to the top of the testis with flow (arrow). Flow is visualized in testis. d Oblique coronal scan posterolateral to the testis after second maneuver shows that the cord is curved (small arrow) and the body of the epididymis is still above the curved cord (large arrow). e, f Sagittal scans after the third maneuver show the head of the epididymis with a normal shape at the top of the testis (arrow in e) and the spermatic cord with a normal straight course (arrow in f)
In one boy cephalic displacement of the whole epididymis was shown at the external inguinal ring with interposing echogenic and enlarged spermatic cord between the epididymis and the testis in the sagittal plane. The epididymis was shown coiled around the enlarged rotated spermatic cord with no flow (Fig. 6).
US scans in patient 6, a 13-year-old boy with acute right testicular pain for 12 h. a Right rotated testis with the probe parallel to its long axis and on the anterior surface of the scrotum. Color Doppler image shows intratesticular flow but not the head of the epididymis at the top of the testis. b Sagittal scan at the external inguinal ring and cephalad to the testis shows that the epididymis (large arrow) is coiled around the twisted spermatic cord (small arrow). Surgical exploration found 540° torsion
In one boy lateral displacement of the head of the epididymis was revealed, with visualization of a small ovoid part of it at the top of the testis, smaller than the half-size of the contralateral epididymis in the sagittal plane. In the oblique coronal plane the body of the epididymis was revealed lateral to the testis and parallel to a rotated spermatic cord. The epididymis was demonstrated without edema or flow (Fig. 7).
US scans in patient 7, a 13-year-old boy with 4 h of sudden-onset acute left testicular pain. a Sagittal plane with the probe on the anterior surface of the scrotum and parallel to the longitudinal axis of the testis. Color Doppler image shows intratesticular flow in the affected testis and the head of the epididymis, with a small oval shape at the top of the testis (arrow) caused by its lateral displacement. Compare image with the normal head of the epididymis in Fig. 1. b Oblique coronal plane laterally to the testis shows spiral twist of the spermatic cord (small arrow) with acoustic shadowing. The body of the epididymis is clearly distinguishable (large arrow). At surgery, 540° torsion was revealed
In one boy the head of the epididymis was displaced anteriorly, with increased curve and superior to the testis toward the inguinal canal in the sagittal plane. When the probe was moved caudally and more laterally to the testis, the body and the tail of the epididymis were also visualized above the twisted cord, which was demonstrated as an enlarged, inhomogeneous, echogenic infratesticular mass with flow. The epididymis was slightly enlarged and hypervascular (Fig. 8).
US scans in patient 8, a 13-year-old boy with 8 h of sudden-onset acute left testicular pain. a Oblique coronal scan caudally to the testis shows the spermatic cord as an enlarged, hyperechogenic, inhomogeneous infratesticular mass (large arrow). A part of the epididymis is also visualized infratesticularly (small arrow). b Color Doppler sagittal scan on the anterior surface of the scrotum shows normal intraparenchymal vascularity and increased vascularity in the infratesticular area. c Color Doppler sagittal scan cephalad to the testis on the anterior surface of the scrotum shows that the head of the epididymis is displaced anteriorly in relation to the testis, with cephalad displacement toward the inguinal canal with increased curve and increased perfusion (arrow). At surgery, 360° torsion was revealed
In one boy lateral displacement of the head of the epididymis was revealed with visualization of a small oval part of it in the sagittal plane. In the same plane the spermatic cord was demonstrated superior to the top of the testis, enlarged, echogenic and curved.
Apart from one child, as mentioned above, similar intratesticular flow to that of the normal testis was demonstrated in the remaining four boys, in whom the testis was visualized with no enlargement.
The testicular parenchyma was homogeneous in all boys.
Table 2 summarizes the sonographic findings of the abnormal epididymis and twisted spermatic cord in the five boys with intratesticular flow on color Doppler sonography. The outcome of each case is also reported.
Discussion
Testicular torsion is one of the most common causes of acute scrotum [12, 13]. Prompt establishment of the correct diagnosis of testicular torsion leads to appropriate management and prevention of testicular loss. Our patients, all with acute testicular torsion but with still-existing intratesticular flow on sonogram, had viable testicles with very good outcome. The presence of intratesticular flow on color Doppler sonography indicates viability of the testis, and early diagnosis of torsion in these cases is of the utmost importance.
Although recent studies have shown high sensitivity (96–100%) and specificity (75.2–95%) of color Doppler sonography in the diagnosis of testicular torsion [3–5], the gradual reduction of testicular perfusion in the initial torsion [14] and the presence of testicular flow in partial torsion of 180° or 90° [5, 6, 12] can lead to missed torsion if the diagnosis is based solely on color Doppler sonography findings.
In our patients the testicular flow was not compromised, compared with the normal side. This finding has been described in cases with partial or complete torsion [8, 9].
Experimental studies have also shown that testicular vessels may not be compromised in incomplete torsion of the spermatic cord [6].
Moreover, Bentley et al. [15] concluded that boys with testicular torsion who have specific anatomical characteristics such as unusually thick spermatic cord preserve intratesticular flow in the affected testis and are at high risk of misleading findings of torsion if the diagnosis is based solely on color Doppler sonography [15].
Several authors have concluded that the key for this diagnostic problem is the visualization of rotated spermatic cord [6, 8, 9, 14, 16]. A large multicenter study showed that the evaluation of the spermatic cord may lead to a higher sensitivity of 97.3% and a higher specificity of 99% in the diagnosis of spermatic cord torsion and, according to their results, a strictly linear cord is an indication to avoid surgical exploration.
The evaluation of the spermatic cord is always included in our protocol of scrotum US examination. Our results in this retrospective study confirmed that the visualization of the twisted spermatic cord can strongly indicate the correct diagnosis, avoiding a false-negative result based solely on color Doppler sonography, as was the case in five of our patients. However, in four of our patients, all incomplete (<270°) torsions, spermatic cord rotation was not demonstrated. Thus, the diagnostic findings that are obtained from the visualization of the cord may not be so striking. In contrary, Arce et al. [8] demonstrated in all six of their pediatric patients with testicular torsion (≥270°) and intratesticular flow on color Doppler sonography that the correct diagnosis of torsion with ultrasonography was based solely on the abnormal course and rotation of the spermatic cord on the affected side. Despite the small number of patients in our review, we can assume that in partial torsion with small degree of twist (<270°) it is possible that the spermatic cord is shown with no rotation on US imaging. Karmazyn et al. [6] have reported the same observation in a boy with partial testicular torsion and normal intratesticular flow, in whom the spermatic cord appeared normal during the US examination while at surgical exploration the cord was demonstrated to be twisted 90°.
In this sonographic review the most consistent observation was lack of visualization caused by abnormal position, or minimal visualization of the epididymal head at the upper pole of the testis in all boys with testicular torsion. Much experience and training are required for the complete evaluation of both epididymis and spermatic cord. The abnormal location and shape of the head of the epididymis can either be the only sonographic finding that may lead to the correct diagnosis of testicular torsion — as was the case in four of our patients, all with partial torsion, with a straight-looking spermatic cord and preserved intratesticular flow — or can be appreciated as an adjunct finding to the presence of twisted spermatic cord, as was the case in five children in this study.
There were no false-positive or false-negative examinations in this study group. Minimal visualization of epididymal head at the upper pole of the testis with a straight-looking spermatic cord and preserved intratesticular flow, as shown in one of our patients (No. 2, Table 1), may be interpreted as a false-negative. In our experience, in a normal testicular sonographic examination, the head of the epididymis is always visualized covering more than half of the superior pole of the testis in the sagittal plane with the probe on the anterior surface of the scrotum. Epididymis with increased flow in acute testicular torsion, as shown in one of our patients (No. 8, Table 2), which is uncommon, could be interpreted as a false-negative. This finding could cause difficulty in differentiating testicular torsion from epididymitis, when the testicular perfusion is similar to that of the contralateral normal testis. In epididymitis the spermatic cord appears swollen but straight, without rotation, and the enlarged epididymis with increased flow retains its normal anatomical position and relationship with the testis and cord, in contrast to torsion [16]. In infants and young children the head of the epididymis is sometimes not visualized, clearly because of its small size and lower echogenicity compared with the epididymis of older children. Therefore in young children more attention and experience is needed in the evaluation of the position and morphology of the epididymis to avoid false-positive results in boys with acute scrotum. No studies describe the occurrence of a false-positive or false-negative abnormal location, size, shape and flow of epididymis, and further studies are needed to validate this observation.
Only in two studies has attention been paid to the position and morphology of the epididymis in testicular torsion. Baud et al. [9] in their series described six boys with normal or slightly abnormal intratesticular flow on color Doppler sonography and absence of visualization of normal epididymal head at the superior pole of the testis. Nussbaum Blask and Rushton [10] postulated that the extratesticular mass in the affected scrotum represents an enlarged epididymis, because they could not clearly distinguish the epididymal structure from the twisted cord. The extratesticular mass that we observed in the affected scrotum of five children in this series was obviously caused, in major part, by the rotated cord that was, however, clearly distinguished from the epididymis, that also was part of the mass.
We need to point out that in cases of constant presence of testicular flow the success of clinical detorsion cannot be based on the changes of flow. This was the case with the only boy in this series with manual detorsion (patient 5, Table 2), in whom the only possible objective sonographic criteria that could be used for the evaluation of successful detorsion were the restoration of the normal appearance and position of the head of the epididymis and the spermatic cord, because testicular blood flow was always present.
We included in our study group a boy with spontaneous detorsion during real-time sonography. Torsion was suspected because of the diametrically opposite position of the avascular head of epididymis in relation to the upper pole of the testis, while the cord was depicted with no rotation and ending up to epididymis. Spontaneous detorsion has been described in the literature in children with spontaneous resolution of the pain and immediate restoration of the flow in an enlarged epididymis and testis, while the spermatic cord remains straight and linear, as in our patient [10].
In one study the diagnosis of partial testicular torsion in seven boys, most of them older than 15 years, was based on abnormal spectral Doppler waveforms [17]. Spectral Doppler sonography was performed in two cases with partial torsion of our study group and had been diagnostic in only one. Spectral Doppler sonography is not easily applied in children because they usually do not collaborate and their testicular volume is not as large as in adults.
The absolute number of children with testicular torsion and abnormal epididymal findings but preserved intratesticular flow in this retrospective study may appear small. However, approximately the same number of cases of preserved testicular flow has been described in the literature in testicular torsion [8, 9]. This may suggest either rarity of this condition from anatomical variations of the spermatic cord or that the findings of abnormal spermatic cord and epididymis are subtle or overlooked and difficult to recognize. Spontaneous regression of testicular torsion may be another explanation. Nevertheless longer prospective studies with a larger number of randomized children are needed to establish the frequency of the findings of our study. The examination of the normal contralateral scrotum outweighed the lack of a control group in the present study.
Conclusion
Preservation of intratesticular flow as well as the visualization of a straight-looking spermatic cord may coexist with acute testicular torsion. In this retrospective study the epididymis was always sonographically abnormal in boys with testicular torsion, being minimally or grossly displaced in relation to the testis and spermatic cord. Therefore careful ultrasonographic evaluation of the epididymis and its relationship with adjacent structures may prove to be a useful adjunct in suspected cases. Moreover, in cases of partial testicular torsion, the abnormal configuration and position of the epididymal head relative to the upper pole of the testis may be the only sonographic abnormality.
References
Beni–Israel T, Goldman M, Bar Chaim S et al (2010) Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med 28:786–789
Gunther P, Schenk JP, Wunsch R et al (2006) Acute testicular torsion in children: the role of sonography in the diagnostic workup. Eur Radiol 16:2527–2532
Altinkilic B, Pilatz A, Weidner W (2013) Detection of normal intratesticular perfusion using color coded duplex sonography obviates need for scrotal exploration in patients with suspected testicular torsion. J Urol 189:1853–1858
Pepe P, Panella P, Pennisi M et al (2006) Does color Doppler sonography improve the clinical assessment of patients with acute scrotum? Eur J Radiol 60:120–124
Waldert M, Klatte T, Schmidbauer J et al (2010) Color Doppler sonography reliably identifies testicular torsion in boys. Urology 75:1170–1174
Karmazyn B, Steinberg R, Kornreich L et al (2005) Clinical and sonographic criteria of acute scrotum in children: a retrospective study of 172 boys. Pediatr Radiol 35:302–310
Dogra V, Gottlieb R, Oka M et al (2003) Sonography of the scrotum. Radiology 227:18–36
Arce J, Cortés M, Vargas J (2002) Sonographic diagnosis of acute spermatic cord torsion. Rotation of the cord: a key to the diagnosis. Pediatr Radiol 32:485–491
Baud C, Veyrac C, Couture A et al (1998) Spiral twist of the spermatic cord: a reliable sign of testicular torsion. Pediatr Radiol 28:950–954
Nussbaum Blask A, Rushton H (2006) Sonographic appearance of the epididymis in pediatric testicular torsion. AJR Am J Roentgenol 187:1627–1635
Leung ML, Gooding GA, Williams RD (1984) High-resolution sonography of scrotal contents in asymptomatic subjects. AJR Am J Roentgenol 143:161–164
Schalamon J, Ainoedhofer H, Schleef J et al (2006) Management of acute scrotum in children — the impact of Doppler ultrasound. J Pediatr Surg 41:1377–1380
Prando D (2009) Torsion of the spermatic cord: the main gray-scale and Doppler sonographic signs. Abdom Imaging 34:648–661
Kalfa N, Veyrac C, Lopez M et al (2007) Multicenter assessment of ultrasound of the spermatic cord in children with acute scrotum. J Urol 177:297–301
Bentley DF, Ricchiuti DJ, Nasrallah PF et al (2004) Spermatic cord torsion with preserved testis perfusion: initial anatomical observations. J Urol 172:2373–2376
Kalfa N, Veyrac C, Baud C et al (2004) Ultrasonography of the spermatic cord in children with testicular torsion: impact on the surgical strategy. J Urol 172:1692–1695
Cassar S, Bhatt S, Paltiel HJ et al (2008) Role of spectral Doppler sonography in the evaluation of partial testicular torsion. J Ultrasound Med 27:1629–1638
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galina, P., Dermentzoglou, V., Baltogiannis, N. et al. Sonographic appearances of the epididymis in boys with acute testicular torsion but preserved testicular blood flow on color Doppler. Pediatr Radiol 45, 1661–1671 (2015). https://doi.org/10.1007/s00247-015-3375-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3375-z