Abstract
Background
Renal Doppler US is used to evaluate suspected vascular causes of hypertension in children, despite mostly unknown diagnostic performance characteristics.
Objective
To evaluate renal Doppler US for detecting vascular causes of hypertension in children with high clinical suspicion of aortic or renal artery narrowing.
Materials and methods
We identified pediatric renal Doppler US examinations performed for hypertension between January 1995 and June 2010 at our institution. We excluded children without follow-up angiography (CT-, MR-, or catheter-based). Two pediatric radiologists reviewed imaging studies and documented relevant findings. Intrarenal spectral Doppler resistive index measurement <0.5 or tardus parvus waveform constituted a positive examination.
Results
Thirty-five boys and 13 girls underwent renal Doppler US and confirmatory imaging (mean age = 9.0 years). Nineteen US examinations were truly negative, two were falsely negative, 18 were truly positive (16 involved narrowing of the aorta or main renal artery) and nine were falsely positive. Sonography had a sensitivity and specificity of 90% and 68%, respectively, for detecting a vascular cause of hypertension.
Conclusion
Renal Doppler sonography reliably detects renin-mediated hypertension caused by aortic or main renal artery narrowing in children. More studies are needed to determine its ability to detect intrarenal and accessory renal artery stenoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Childhood hypertension is uncommon but it is associated with substantial morbidity, including hypertensive encephalopathy, stroke, cardiac diastolic dysfunction, and left ventricular hypertrophy [1]. In infants and children, unlike in adults, secondary hypertension, or elevated blood pressure caused by an identifiable, potentially correctable cause, is commonplace. Secondary hypertension in children has many causes, including: suprarenal aortic and renovascular narrowing, a variety of congenital and acquired renal parenchymal abnormalities, hormone-producing tumors (e.g., reninoma, neuroblastoma, pheochromocytoma and adrenocortical neoplasm) and endocrine dysfunction [2, 3]. A recent study by Gomes et al. [3] demonstrated an identifiable cause for hypertension in 85% of children presenting to a pediatric nephrology clinic specializing in hypertension. The most common cause in that study’s children was intrinsic renal disease, accounting for 78% of cases. A second large study of hypertensive children from Poland demonstrated intrinsic renal disease, most commonly reflux nephropathy, in 68% of cases [2].
Identifying the presence of renin-angiotensin-mediated renovascular hypertension is crucial because interventional and surgical therapies can be curative and spare affected children from a lifetime of anti-hypertensive therapy and hypertension-related complications. Suprarenal aortic or renal arterial narrowings are important causes of hypertension in children, accounting for 2% to 10% of cases [3–8]. There are various categories of pediatric aortic and renovascular hypertension, including those caused by embolus or thrombus related to umbilical artery catheterization in neonates; developmental arterial narrowing (often referred to as fibromuscular dysplasia with combinations of intimal fibroplasia, medial thinning and excess external elastic lamina) [8, 9]; congenital thoracic or abdominal aortic coarctation or interruption; inflammatory aortoarteritis, such as occurs with Takayasu arteritis and radiation-induced vascular injury; congenital aneurysms; and extrinsic renal arterial compression, such as occurs with retroperitoneal tumors like neuroblastoma [1, 5]. Numerous syndromes are associated with vascular causes of hypertension, such as neurofibromatosis type 1 (NF-1), Williams syndrome, Turner syndrome and tuberous sclerosis [1, 8, 10].
Imaging challenges in the assessment of renovascular hypertension are different for children compared to adults. In particular, imaging of pediatric renovascular hypertension can be difficult because of smaller-caliber blood vessels, difficulty timing imaging with respect to intravascular contrast material administration, lack of patient cooperation contributing to increased motion artifacts, and efforts to minimize ionizing radiation exposure. Although catheter-based intra-arterial digital subtraction arteriography (IADSA) is the gold standard for the diagnosis of aortic and renovascular causes of hypertension because of its excellent spatial and contrast resolution, it is an invasive procedure associated with a variety of complications in addition to its exposure to ionizing radiation. Less invasive imaging modalities have been used more recently to assess aortic and renovascular hypertension in children, including renal sonography with Doppler, computed tomography angiography (CTA) and magnetic resonance angiography (MRA). These cross-sectional imaging tests also allow for evaluation of renal size and parenchymal quality and may identify potential non-renal causes of hypertension (e.g., pheochromocytoma or aldosteronoma arising from the adrenal gland) [11, 12].
The purpose of the present study was to retrospectively assess the ability of renal sonography with Doppler to detect the presence of vascular causes of hypertension in children with high clinical suspicion of aortic or renal artery narrowing, using CTA, MRA and intra-arterial digital subtraction arteriography as reference standards.
Materials and methods
This retrospective investigation was approved by our institutional review board and compliant with HIPAA. The need for informed consent was waived.
We identified all children within the University of Michigan Health System who underwent renal sonography for the evaluation of hypertension between January 1, 1995, and June 30, 2010. These children, all younger than 18 years, were identified through a search of institutional electronic medical records for renal US examinations that included the following terms in the provided clinical information: “hypertension,” “renal artery stenosis,” “renovascular hypertension” and “blood pressure.” All children without a follow-up confirmatory imaging test (CTA, MRA or intra-arterial digital subtraction arteriography) were considered to have low clinical suspicion for renin-mediated hypertension and were excluded. Children were also excluded if the identified renal US examination was performed without spectral Doppler US, or if the spectral Doppler data obtained was determined to be nondiagnostic.
Pertinent US examinations were retrospectively reviewed by two fellowship-trained pediatric radiologists (2 and 4 years’ experience interpreting US examinations, respectively). Radiologists were blinded to the original imaging report documented in the medical record. All identified imaging examinations performed prior to the year 2000 were film-based and were successfully retrieved from an off-site storage facility. Imaging performed from 2000 to 2010 was reviewed on a PACS workstation. Renal Doppler US studies were documented as being either positive or negative for evidence of aortic or renovascular stenotic disease based on consensus agreement. The following US findings (either isolated or in combination) were used to establish an examination as being positive: (1) abnormally low intrarenal spectral Doppler resistive index measuring less than 0.5, and (2) tardus parvus morphology of the spectral Doppler waveform (abnormally slow systolic acceleration with decreased peak systolic velocity). Our standardized institutional protocol for renal US with Doppler examination includes gray-scale imaging of the kidneys in both the longitudinal and transverse planes; color Doppler imaging of the kidneys, main renal arteries and main renal veins; spectral Doppler of the main renal arteries and main renal veins; and intrarenal spectral Doppler evaluation of upper-, mid- and lower-pole arcuate arteries with resistive index measurements. If bilateral intrarenal spectral Doppler waveforms are abnormal, then imaging of the suprarenal abdominal aorta is performed to assess for aortic coarctation or middle aortic syndrome. US imaging was performed using numerous machines from a variety of manufacturers over the course of the study period. Examinations performed during the routine workday were scanned by pediatric-dedicated technologists, whereas afterhours and weekend examinations were performed by both pediatric-dedicated technologists and technologists who scan primarily adults within our health system but that have at least some pediatric training.
Pertinent confirmatory angiographic (CTA, MRA or intra-arterial digital subtraction arteriography) examinations (both images and reports) from the same children were also retrospectively reviewed by the same two pediatric radiologists. These imaging examinations were recorded as being either positive or negative for the presence of aortic or renovascular stenoses, and relevant imaging findings were documented. All MRA examinations included a gadolinium-enhanced three-dimensional MRA sequence in the arterial phase, while all intra-arterial digital subtraction arteriography examinations included both frontal and lateral aortography as well as selective (and sometimes superselective) injections of the renal arteries.
Finally, a single author reviewed electronic medical records to record pertinent demographic data and how children were clinically or surgically managed after their index renal US examinations. We reviewed the medical records following confirmatory angiographic imaging in false-positive and true-negative patients to determine whether a renin-mediated cause of hypertension was later identified.
Statistical analysis
Continuous data were summarized using means and ranges, while categorical data were summarized by counts and percentages. The sensitivity and specificity of renal sonography with Doppler for detecting aortic and renovascular causes of hypertension in children were calculated with 95% confidence intervals, using the aforementioned confirmatory imaging tests as the reference standard. Three secondary analyses were also performed. In particular, the sensitivity and specificity of renal sonography with Doppler were determined when using only intra-arterial digital subtraction arteriography as the reference standard, as well as in patients with isolated renal artery stenosis and no aortic narrowing (using IADSA alone as well as using CTA, MRA or IADSA as reference standards). The Wilcoxon rank sum test and Fisher exact test, respectively, were used to compare the mean ages and genders between children with and without the final diagnosis of aortic or renovascular hypertension. The unpaired two-tailed t-test was used to compare the mean minimum resistive index measurements between true-positive and false-positive patients. A P-value of <0.05 was considered statistically significant. The above procedures were performed in SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
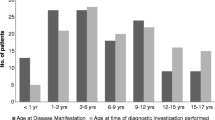
A total of 928 pediatric renal US examinations meeting our initial search criteria were performed during the study period. Forty-eight examinations in 48 children were determined to have diagnostic renal Doppler imaging as well as one or more subsequent confirmatory imaging tests. Among the children with confirmatory testing, there were 35 boys and 13 girls, with a mean age 9.0 years (range, 1 month to 17.7 years).
Primary analysis
Twenty-one of the 48 renal Doppler examinations were negative. Secondary imaging performed in these children because of high clinical suspicion for aortic or renovascular hypertension documented 19 of these examinations to be truly negative and two to be falsely negative (Fig. 1). Twenty-seven of the 48 renal Doppler examinations were positive, including 18 that were truly positive based on confirmatory imaging and nine that were falsely positive (Fig. 2).
False-negative Doppler US imaging in a 3-year-old boy with hypertension for 1 year. a Spectral Doppler evaluation of the kidneys shows normal intrarenal waveform and resistive index (RI = 0.68). b Maximum-intensity projection MRA image demonstrates focal narrowing of the mid descending thoracic aorta (black arrow) as well as abnormal tapering of the infrarenal abdominal aorta. Both renal arteries are diminutive in appearance with more focal proximal narrowing (white arrows)
False-positive Doppler US imaging in an 11-year-old girl with hypertension. a Spectral Doppler interrogation of the left kidney demonstrates an intrarenal tardus parvus waveform and abnormally low resistive index (RI = 0.45). b Maximum-intensity projection MRA image reveals a normal-appearing left renal artery
Based on the aforementioned results, renal sonography with Doppler has a sensitivity of 90% (95% CI, 68–99%) and specificity of 68% (95% CI, 48–84%) for the detection of aortic and renovascular stenoses in our hypertensive pediatric population when using CTA, MRA or intra-arterial digital subtraction arteriography as reference standards. True-positive cases had the following renal Doppler findings: six children with tardus parvus waveforms only (three bilateral, three unilateral), five children with abnormally low resistive indices only (two bilateral, three unilateral) and seven children with tardus parvus waveforms and abnormally low resistive indices (four bilateral, three unilateral). The nine false-positive US cases had the following renal Doppler findings: one child with bilateral tardus parvus waveforms, six children with abnormally low resistive indices only (two bilateral and four unilateral) and two children with bilateral tardus parvus waveforms and abnormally low resistive indices. Mean true-positive minimum resistive index was 0.35 (range, 0.20–0.48), while mean false-positive minimum resistive index was significantly higher, measuring 0.43 (range, 0.38–0.49) (P=0.02).
Confirmatory testing in the 48 children included 23 children who underwent MRA only, 13 who underwent intra-arterial digital subtraction arteriography only, ten who underwent both MRA and IADSA, one who underwent CTA only and one who underwent both MRA and CTA. Among the 18 children with positive confirmatory imaging, nine had aortic pathology–three had thoracic aortic coarctation (Figs. 1 and 3), three had abdominal aortic aneurysms with associated renal artery stenosis, two had suprarenal abdominal aortic narrowing with associated renal artery stenosis and one had an abdominal aortic pseudoaneurysm from recent surgery with resultant renal artery narrowing (Fig. 4). The remaining nine children had primary renal artery narrowings: six with unilateral renal artery stenosis (four ostial, one mid main renal artery and one with stenosis of an accessory inferior polar renal artery) and three with bilateral renal artery narrowing (one bilateral ostial, one bilateral segmental/arcuate arteries and one with a large neuroblastoma causing bilateral renal artery narrowing due to mass effect) (Fig. 5).
Thoracic aortic coarctation in a 12-year-old boy with abdominal pain and incidentally detected hypertension in the Emergency Department. a, b Spectral Doppler interrogation of the kidneys demonstrates bilateral intrarenal tardus parvus waveforms and abnormally low resistive indices (RI = 0.26 and 0.28). c Sagittal black blood MR image demonstrates severe focal narrowing (arrow) of the thoracic aorta, just distal to the left subclavian artery, consistent with an isthmic aortic coarctation
Persistent hypertension following right nephrectomy, patch aortoplasty and left renal artery reimplantation in a 5-year-old boy. a Intrarenal spectral Doppler interrogation of the left kidney demonstrates an abnormally low resistive index (RI = 0.48) without tardus parvus waveform. b Maximum-intensity projection MRA image shows abnormal narrowing of the proximal left renal artery caused by mass effect from a small pseudoaneurysm (arrow) and associated hematoma arising from the suprarenal abdominal aorta. Ectasia and undulation of the infrarenal abdominal aorta is from the aortoplasty (arrowheads)
Primary renal artery narrowing in an 11-year-old boy with incidentally detected hypertension during routine primary care physician visit. a, b Spectral Doppler interrogation of the kidneys demonstrates bilateral abnormally low resistive indices. c Volume-rendered CTA image demonstrates bilateral proximal main renal artery narrowings (arrows). There is also proximal stenosis of an accessory renal artery on the left (arrowhead)
Twelve of the 18 children with positive confirmatory testing were managed surgically, four continued medical management and two underwent aortic stenting. One medically managed child died prior to surgery from hemodynamic collapse related to pulmonary hypertension. Of the surgically treated children, 11 underwent revascularization procedures. A single child underwent unilateral nephrectomy. The kidney that was removed exhibited diffuse renal hypoplasia, including hypoplasia of the renal arterial system, upon pathological analysis.
The mean age of the children found to have an aortic or renovascular cause for hypertension on confirmatory testing was 5.1 years (range, 1 month to 12 years), while the mean age of the children without a confirmed cause of renovascular hypertension was 11.9 years (range, 2–17 years) (P=0.0001). The mean age for children with a true-positive US examination was 4.8 years (range, 1 month to 12 years); false-negative US examination was 8.0 years (two children; both 8 years old); true-negative US examination was 11.9 years (range, 2–17 years); false-positive US examination was 11.8 years (range, 3–17 years). Fifteen boys and five girls were found to have a renovascular cause for hypertension on confirmatory testing, while 20 boys and eight girls were found to have no aortic or renovascular cause (P=1.0).
Secondary analyses
Using intra-arterial digital subtraction arteriography alone as the reference standard (n=23), 11 renal sonography with Doppler examinations were truly positive, three were falsely positive, seven were truly negative, and two were falsely negative. These results yield a renal Doppler sensitivity of 85% (95% CI, 55–98%) and specificity of 70% (95% CI, 35–93%).
When we evaluated children with isolated renal artery stenosis using CTA, MRA or intra-arterial digital subtraction arteriography as reference standards (n=39; 9 of the 48 children found to have aortic abnormalities on CTA, MRA or IADSA were excluded), nine renal Doppler examinations were truly positive, nine were falsely positive, 19 were truly negative and two were falsely negative. These results yield a renal Doppler sensitivity of 82% (95% CI, 48–97%) and specificity of 68% (95% CI, 48–84%).
When the above children with isolated renal artery stenosis were further subdivided to include all children who underwent intra-arterial digital subtraction arteriography, 18 children were identified. Six renal Doppler examinations were truly positive, three were falsely positive, seven were truly negative, and two were falsely negative. Based on these results, renal Doppler has a sensitivity of 75% (95% CI, 35–96%) and specificity of 70% (95% CI, 35–93%) when compared to intra-arterial digital subtraction arteriography.
Discussion
The clinical diagnosis of aortic and renovascular hypertension in children can be difficult. Certain clinical parameters that can direct the pediatrician toward a diagnosis of renin-mediated hypertension include a systolic blood pressure greater than 200 mmHg at presentation and hypertension that is refractory to multiple medications [3, 5]. However these findings are considered neither sensitive nor specific enough to detect renin-mediated hypertension when present and exclude it when absent [5].
Because the clinical diagnosis of renin-mediated hypertension is challenging, imaging evaluation of hypertensive children is frequently performed [13]. Renal sonography with Doppler is commonly used as an initial screening test for both children and adults with suspected aortic and renovascular disease because of its noninvasiveness, low cost, widespread availability and lack of need for ionizing radiation, sedation or intravascular contrast media. However this use in children is supported in neither the pediatric radiology nor pediatric hypertension literature, because sensitivity and specificity are unclear [14].
Direct visualization of the renal arteries using either gray-scale or Doppler US is not always reliable in children based on our institutional experience, and thus assessment for aortic and renovascular causes of hypertension has frequently been performed using evaluation of a variety of secondary gray-scale and Doppler US findings [11]. For example the affected kidney might appear unusually small, abnormally low intrarenal resistive indices might be observed with spectral Doppler interrogation, and the acquired waveform might exhibit a tardus parvus configuration [15]. These spectral Doppler US findings have been described in the setting of renal artery and suprarenal aortic narrowing [11]. Renal sonography with Doppler does have known disadvantages, however, including operator dependence, occasionally inadequate acoustic windows from intervening bowel gas or body habitus, and considerable limitations with respect to identifying accessory renal artery, branch renal artery and intrarenal renal artery stenoses [16–19].
Multiple reports describing the use of sonography in the evaluation of renal artery stenosis have focused almost exclusively on adult populations. Early investigations were limited because of technical difficulties resulting in nondiagnostic studies ranging from 25% to 50% [17, 19]. More recent investigations have demonstrated adequate renal Doppler examinations in up to 96% of adults, likely reflecting a combination of advances in US technology and increased user confidence [20]. Still, some reports describe particular difficulty directly imaging areas of main renal artery narrowing, and even more difficulty identifying narrowed small accessory renal arteries and intrarenal arterial segments [17–19].
In children the small main renal arteries and even smaller accessory renal arteries make direct arterial imaging very challenging and sometimes impossible [5]. As such, renal Doppler examinations performed on children often rely upon interrogation of segmental (arcuate) intrarenal arteries by identifying indirect spectral Doppler evidence of more proximal arterial narrowing, such as tardus parvus waveforms or abnormally decreased resistive indices. Segmental and more peripheral focal renal artery stenoses have also been shown to be a common cause of renovascular hypertension in children [10]. It is interesting to note that a larger surgical series by Stanley et al. [8] that described 97 children with renin-mediated hypertension found ostial and main renal artery stenoses to be more common than distal stenoses based on intra-arterial digital subtraction arteriography. Using catheter-based angiography as their reference standard, Stavros et al. [21] demonstrated that intrarenal spectral Doppler assessment of segmental arteries evaluating for tardus parvus waveforms has a high technical success rate, is highly sensitive and specific and shortens examination times.
An earlier study of 58 adults comparing renal sonography with Doppler to intra-arterial digital subtraction arteriography found the sensitivity and specificity of renal Doppler sonography to be 73% and 71%, respectively [22]. In a second series, with 129 adults, renal sonography with Doppler studies had a sensitivity of 75% and a specificity of 86% compared to intra-arterial digital subtraction arteriography [23]. In a study performed more than a decade ago, 22 children with hypertension underwent both renal Doppler sonography and intra-arterial digital subtraction arteriography [24]. A total of 13 children in that series were shown to have renal artery stenosis by IADSA. Among the 22 children evaluated, there were two false-negative and two false-positive cases by sonography, yielding a sensitivity of 83% and a specificity of 78%.
In the present investigation of 48 children with high clinical suspicion for aortic or renovascular hypertension, there were 18 true-positive, 9 false-positive, 19 true-negative, and 2 false-negative instances when using CTA, MRA or intra-arterial digital subtraction arteriography as reference standards. Consequently, renal sonography with Doppler had a sensitivity of 90% (95% CI, 68–99%) and a specificity of 68% (95% CI, 48–84%). Renal Doppler imaging fared similarly (within the 95% confidence intervals of our primary analysis) based on a variety of secondary analyses, with sensitivities ranging from 75% to 85% and specificities ranging from 68% to 70%. Based on our results and the location of arterial lesions in our patient population, renal sonography with Doppler appears to be very sensitive for detecting narrowings of the suprarenal aortic and main renal arteries, identifying the cause of hypertension in 16 of 16 such patients. Only two true-positive cases were from segmental/arcuate or accessory renal artery narrowings. Our false-negative cases suggest that renal Doppler might be limited for detecting the latter lesions, because one false-negative patient had arcuate artery narrowing and the other had narrowing of an accessory inferior polar renal artery. Ultimately our study is too small to confidently establish the sensitivity and specificity of renal Doppler sonography for detecting renovascular causes of hypertension distal to the main renal artery or caused by accessory renal artery narrowing.
A substantial number of false-positive cases were present in our study that consequently decreased the specificity of renal Doppler US. There are two primary explanations for these false-positive results. First it is possible that renal Doppler US is actually more sensitive than MRA or CTA and that the US examination in reality would be a true positive if compared to intra-arterial digital subtraction arteriography. Second it is possible that our resistive index cut-off of 0.5 was too high and overly sensitive. Eight of nine false-positive cases demonstrated low resistive indices with an average minimum RI measurement of 0.43. Although true-positive cases had resistive index measurements that were significantly lower (mean = 0.35), there was substantial overlap between these the true- and false-positive groups. Thus lowering the resistive index threshold for a positive Doppler examination would improve specificity but lower sensitivity. False-positive resistive indices could be caused by a variety of factors, because measurements can be affected by vascular compliance and resistance, heart rate, downstream cross-sectional area, hydration state and even age [14]. It is important to note that no false-positive or true-negative patient was eventually diagnosed with renin-mediated hypertension upon follow-up, based on a review of available medical records (mean follow-up period 5.8 years, range 6 months to 16 years).
The present investigation has limitations. First it is retrospective in design and might have inherent subject selection bias. For example we included only children with high clinical suspicion for renin-mediated hypertension who had available CTA, MRA or catheter-based confirmatory imaging. Second we looked for only indirect spectral Doppler evidence of aortic or renovascular narrowing, based on intrarenal arterial tardus parvus waveforms and abnormally decreased resistive indices. Prior studies in adults have discussed the use of other imaging parameters not evaluated in our study, including main renal artery peak systolic velocity, velocity of the main renal artery compared to the abdominal aorta (the renal artery–aorta ratio) and spectral Doppler waveform acceleration time [17, 18, 22, 23].
Our primary analysis also assumes that MRA, CTA and intra-arterial digital subtraction arteriography have similar performances for the detection of aortic and renal artery stenoses (both extrarenal and intrarenal), although this has not been definitively demonstrated in children. We have attempted to account for this specific limitation by performing multiple secondary analyses, two of which only use intra-arterial digital subtraction arteriography as the reference standard. As mentioned above, it is conceivable that renal Doppler sonography is more sensitive than MRA or CTA, thus causing several of our false-positive cases and artifactually lowering our specificity calculations. Similarly the use of MRA or CTA as reference standards, if falsely negative (e.g., compared to intra-arterial digital subtraction arteriography, which was not performed), could incorrectly categorize some of our true-negative patients, thus artifactually increasing our sensitivity calculations. Finally, MRA and CTA techniques have changed over time as state-of-the-art has evolved. As a result it is conceivable that MRA and CTA examinations performed later in the study period were more likely to detect aortic and renal artery narrowings than examinations performed early in the study period.
Conclusion
We have shown that renal sonography with Doppler appears to be sensitive for identifying cases of pediatric renin-mediated hypertension caused by aortic and main renal artery narrowings. We cannot definitively establish the sensitivity of renal Doppler US for detecting more distal intrarenal or accessory renal artery stenoses. Aortic abnormalities were as common as renal artery narrowings in our population, suggesting that aortic assessment should likely be mandatory when performing renal Doppler US for hypertension. Because both false-positive and false-negative renal Doppler examinations were identified, children with a high clinical suspicion for renin-mediated hypertension should undergo intra-arterial digital subtraction arteriography to directly visualize the aorta and renal arteries, regardless of whether renal Doppler US findings are positive or negative. If the renal Doppler examination is negative, intra-arterial digital subtraction arteriography is necessary to conclusively exclude the possibility of renin-mediated hypertension (e.g., caused by intrarenal or accessory renal artery narrowing). If the renal Doppler examination is positive, then intra-arterial digital subtraction arteriography is needed to completely evaluate the child’s aorta and renal arteries to direct appropriate medical and surgical management. Because renal US examination can detect several non-renin-mediated causes of hypertension, it is likely that this imaging modality will continue to play an important role in the assessment of hypertensive children and adolescents.
References
Mitsnefes MM (2006) Hypertension in children and adolescents. Pediatr Clin North Am 53:493–512
Wyszynska T, Cichocka E, Wieteska-Klimczak A et al (1992) A single pediatric center experience with 1,025 children with hypertension. Acta Paediatr 81:244–246
Gomes RS, Quirino IG, Pereira RM et al (2011) Primary versus secondary hypertension in children followed up at an outpatient tertiary unit. Pediatr Nephrol 26:441–447
Kim HJ, Son JS, Kim KS (2011) A case of renal artery stenosis in a child confirmed by multidetector computed tomographic angiography. Pediatr Cardiol 32:702–703
Tullus K, Brennan E, Hamilton G et al (2008) Renovascular hypertension in children. Lancet 371:1453–1463
Srinivasan A, Krishnamurthy G, Fontalvo-Herazo L et al (2010) Angioplasty for renal artery stenosis in pediatric patients: an 11-year retrospective experience. J Vasc Interv Radiol 21:1672–1680
Srinivasan A, Krishnamurthy G, Fontalvo-Herazo L et al (2011) Spectrum of renal findings in pediatric fibromuscular dysplasia and neurofibromatosis type 1. Pediatr Radiol 41:308–316
Stanley JC, Criado E, Upchurch GR Jr et al (2006) Pediatric renovascular hypertension: 132 primary and 30 secondary operations in 97 children. J Vasc Surg 44:1219–1228
Devaney K, Kapur SP, Patterson K et al (1991) Pediatric renal artery dysplasia: a morphologic study. Pediatr Pathol 11:609–621
Vo NJ, Hammelman BD, Racadio JM et al (2006) Anatomic distribution of renal artery stenosis in children: implications for imaging. Pediatr Radiol 36:1032–1036
Tullus K, Roebuck DJ, McLaren CA et al (2010) Imaging in the evaluation of renovascular disease. Pediatr Nephrol 25:1049–1056
Soulez G, Olivia VL, Turpin S et al (2000) Imaging of renovascular hypertension: respective values of renal scintigraphy, renal Doppler US, and MR angiography. Radiographics 20:1355–1368
Castelli PK, Dillman JR, Smith EA et al (2013) Imaging of renin-mediated hypertension in children. AJR Am J Roentgenol 200:W661–W672
Coley BD (2004) Pediatric applications of abdominal vascular Doppler: part II. Pediatr Radiol 34:772–786
Roth CG, Spottswood SE, Chan JC et al (2003) Evaluation of the hypertensive infant: a rational approach to diagnosis. Radiol Clin North Am 41:931–944
Garel L, Dubois J, Robitaille P et al (1995) Renovascular hypertension in children: curability predicted with negative intrarenal Doppler US results. Radiology 195:401–405
Desberg AL, Paushter DM, Lammert GK et al (1990) Renal artery stenosis: evaluation with color Doppler flow imaging. Radiology 177:749–753
Baxter GM, Aitchison F, Sheppard D et al (1996) Colour Doppler ultrasound in renal artery stenosis: intrarenal waveform analysis. Br J Radiol 69:810–815
Postma CT, van Aalen J, de Boo T et al (1992) Doppler ultrasound scanning in the detection of renal artery stenosis in hypertensive patients. Br J Radiol 65:857–860
Li JC, Wang L, Jiang YX et al (2006) Evaluation of renal artery stenosis with velocity parameters of Doppler sonography. J Ultrasound Med 25:735–742
Stavros AT, Parker SH, Yakes WF et al (1992) Segmental stenosis of the renal artery: pattern recognition of tardus and parvus abnormalities with duplex sonography. Radiology 184:487–492
Eklof H, Ahlstrom H, Magnusson A et al (2006) A prospective comparison of duplex ultrasonography, captopril renography, MRA, and CTA in assessing renal artery stenosis. Acta Radiol 47:764–774
Rountas C, Vlychou M, Vassiou K et al (2007) Imaging modalities for renal artery stenosis in suspected renovascular hypertension: prospective intraindividual comparison of color Doppler US, CT angiography, GD-enhanced MR angiography, and digital subtraction angiography. Ren Fail 29:295–302
Brun P, Kchouk H, Mouchet B et al (1997) Value of Doppler ultrasound for the diagnosis of renal artery stenosis in children. Pediatr Nephrol 11:27–30
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castelli, P.K., Dillman, J.R., Kershaw, D.B. et al. Renal sonography with Doppler for detecting suspected pediatric renin-mediated hypertension – is it adequate?. Pediatr Radiol 44, 42–49 (2014). https://doi.org/10.1007/s00247-013-2785-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2785-z