Abstract
Background
Renal artery stenosis (RAS) causes significant hypertension in children. Frequently, pediatric RAS occurs with systemic disorders. In these cases, stenoses are often complex and/or include long segments. We believed that hypertensive children without comorbid conditions had a different lesion distribution and that the difference might have implications for imaging and treatment.
Objective
To identify locations of RAS lesions in these hypertensive children without comorbid conditions.
Materials and methods
Patients who had renal angiography for hypertension from 1993 to 2005 were identified. Patients with systemic disorders, renovascular surgery, or normal angiograms were excluded. The angiograms of the remaining patients were reviewed for number, type, and location of stenoses.
Results
Eighty-seven patients underwent renal angiography for hypertension; 30 were excluded for comorbid conditions. Twenty-one of the remaining 57 patients had abnormal angiograms; 24 stenoses were identified in those patients. All were focal and distributed as follows: 6 (25%) main renal artery, 12 (50%) 2nd order branch, 3 (12.5%) 3rd order branch, and 3 (12.5%) accessory renal artery.
Conclusion
Hypertensive children without comorbid conditions who have RAS usually have single, focal branch artery stenoses. This distribution supports angiography in these patients because of its superior sensitivity in detecting branch vessel disease and its therapeutic role in percutaneous transluminal renal angioplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renovascular disease accounts for up to 10% of cases of pediatric hypertension [1, 2]. Many cases of renal artery stenosis (RAS) are associated with established disorders including vasculitides (Takayasu disease, Moya-Moya), syndromes (Turner, Marfan, Williams, Klippel-Trenaunay-Weber, mid-aortic), neurofibromatosis and previous renal artery surgical procedures. Children with these comorbid conditions often have complex lesions that can be multiple and/or include long-segment stenoses [1, 2].
We believed that the subset of hypertensive children without comorbid conditions had a different distribution of lesions and that the differences might have implications for imaging and treatment. In particular, angiography has been shown to have superior sensitivity in detecting renal artery lesions distal to the main renal artery [3, 4]; if lesions occurred in this location, non-invasive evaluations might miss a significant number of these stenoses. This study was, therefore, designed to characterize the location and distribution of RAS as demonstrated by renal angiography in hypertensive children with no known comorbid condition.
Materials and methods
With Institutional Review Board approval, using both a medical free text search engine at our institution and manual review of the interventional radiology procedure logs, we identified patients who had undergone renal angiography for the indication of hypertension from Jan. 1, 1993, through April 15, 2005. Any patients with a history of an underlying systemic vascular disorder or syndrome (neurofibromatosis, Takayasu arteritis, mid-aortic syndrome, Williams syndrome, Turner syndrome, Moya-Moya disease, tuberous sclerosis, and Von Willebrand syndrome type 1), prior renal bypass vascular grafts, or renal transplant were excluded. All of the patients with normal angiograms were also excluded. This left only the patients who had no other systemic comorbid diseases or prior surgical intervention and who had abnormal renal angiograms performed specifically for hypertension. The angiograms from these patients were reviewed in detail.
All patients were referred to the pediatric interventional radiology service for unexplained, persistent hypertension (>95th percentile) by a pediatric nephrologist or by a pediatric vascular surgeon after consultation with a pediatric nephrologist. A flush aortogram was performed on each patient prior to selective renal artery angiography, which included LPO and RPO views as well as selective injections of any accessory renal arteries. The number, location, and type (focal or long-segment) of stenoses were documented for each patient. Lesions were classified as main renal artery (ostial or otherwise), 2nd order branch, 3rd order branch, or accessory renal artery.
Results
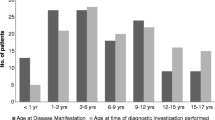
Eighty-seven patients underwent renal angiography for hypertension; 30 (34%) of those were excluded for comorbid conditions. Twenty-one (37%) of the remaining 57 patients had abnormal angiograms. This included 12 males and 9 females, with an age range of 30 months to 18 years (mean 9 years, 3 months).
A total of 24 stenotic lesions were identified, all of which were focal. The lesion distribution was: 6 (25%) in the main renal artery, 12 (50%) in a 2nd order renal artery branch, 3 (12.5%) in a 3rd order branch, and 3 (12.5%) in an accessory renal artery or a branch off the accessory artery (Fig. 1). Of the six stenoses that involved the main renal artery, there was a single ostial lesion and five lesions distal to the origin. Nineteen of the 21 patients (90%) had a single stenosis. One patient had two stenoses (one main renal artery stenosis and one ipsilateral upper pole 2nd order branch stenosis) while another patient had three (one main renal artery stenosis and two ipsilateral 2nd order branch stenoses). The stenoses were equally distributed bilaterally (12 right, 12 left). No angiographic complications occurred in this series.
Discussion
While pediatric hypertension is often silent, the consequences of untreated long-standing hypertension can be significant and include neurologic sequelae, congestive heart failure, renal failure, and shortened longevity [5]. Severe hypertension from RAS occurs when there is a critical narrowing of the renal artery leading to reduced blood flow to the affected kidney or renal segment. That kidney then releases increased amounts of renin, which has several effects, including systemic vasoconstriction, that lead to increased blood pressure [5].
Numerous pediatric disorders have been associated with RAS. Neurofibromatosis, which is characterized by peripheral nerve tumors, is often accompanied by dysplastic abnormalities of the blood vessels, as well [6]. Takayasu arteritis, mid-aortic syndrome, Williams syndrome, Turner syndrome, tuberous sclerosis, and Von Willebrand syndrome type 1 have all been associated with RAS. The lesions that occur in patients with these disorders are frequently multiple and complex with long-segment stenoses [1, 2]. Children who have had renal transplants or prior revascularization procedures can also be affected by RAS, which occurs secondary to scarring at the surgical anastomosis [7]. In children without comorbid conditions, RAS is usually caused by focal fibromuscular dysplasia (FMD) [5]. FMD is a disorder of medium-size arteries, including the renal arteries. It is a non-inflammatory and non-atherosclerotic disease that can affect the intima, media, and adventitia, though usually the term is used to describe medial hyperplasia [2, 8].
Studies that have evaluated the anatomy, imaging, and treatment of RAS in children have generally included patients with and without comorbid conditions as one heterogeneous group [1, 2, 5, 9–11]. Our observations suggest that it is important to consider the patients without comorbid associations separately because the arterial lesions are quite different, and these differences have implications for imaging and for therapy. In our evaluation, we found that all of the lesions in these hypertensive children without associated disease were focal, and 90% of the patients had only a single lesion. In addition, 75% of the lesions were located either in branch arteries or accessory arteries (Figs. 2, 3, 4 and 5).
A 14-year-old hypertensive girl with RAS. a AP projection demonstrates delayed flow to a wedge-shape distribution (triangle) in the left lower pole suggesting a proximal stenosis, though none is seen on this projection. Subsequent views demonstrates a stenosis, which had been obscured by an overlying vessel (circle). b Oblique with caudal angulation reveals the high-grade focal stenosis of a lower pole 3rd order branch artery (arrow)
There is no uniform method for the evaluation of children with hypertension and suspected RAS. Doppler US can be useful in detecting RAS in adults, though it is also very dependent on operator expertise. An increased velocity as blood passes through a narrow lumen is indicative of significant RAS. The presence of a proximal stenotic lesion can also be inferred from a tardus or parvus (late or flat) waveform observed in the distal vessels [12]. However, even in experienced labs, localizing a specific lesion can be challenging and time-consuming, and a negative study might not be definitive. In particular, accessory renal artery stenoses and branch RAS have been shown to be very difficult to document with Doppler US [13].
Measurement of plasma renin activity, the captopril plasma renin test, and renal vein renin sampling have all been used to try to identify patients with possible RAS by measuring the functional consequences of renal artery obstruction. Captopril-enhanced renal scintigraphy, a non-invasive test that evaluates perfusion and renal function after administration of the angiotensin-converting enzyme inhibitor captopril, continues to be recommended to identify RAS. This technique has been reported to have fairly high sensitivity and specificity in adults with normal renal function and unilateral disease [12, 14]. However, none of these tests provides enough sensitivity to reliably eliminate RAS as the cause for hypertension, and because newer, better technologies have become available, they have largely fallen out of favor among clinicians [12, 15].
CT angiography (CTA) and MR angiography (MRA) have also been purported to have benefit in the evaluation of RAS. A meta-analysis on the non-invasive evaluation of renovascular hypertension showed that both CTA and gadolinium-enhanced MRA (Gd-MRA) had significantly better accuracy than ultrasonography and captopril scintigraphy [16]. Both tests have been reported to have very high sensitivity and specificity, though these reports were generally limited to patients with atherosclerotic main RAS [12, 16].
Angiography has long been considered the gold standard for the evaluation of patients with renal vascular hypertension [1, 3, 12]. However, because of the invasive nature of angiography, it has not been universally embraced, nor are there any accepted standard recommendations for its use in children. Several studies have compared CTA and MRA with angiography for the diagnosis of RAS in adults. Schoenberg et al. [4] directly compared Gd-MRA with digital subtraction angiography (DSA) and concluded that Gd-MRA was a safe and noninvasive alternative to DSA. Vasbinder et al. [3] also performed a large prospective trial directly comparing CTA and MRA with DSA and found that CTA and MRA were not reproducible or sensitive enough to rule out RAS in hypertensive adults. However, both of these studies noted that because of inadequate spatial resolution, the sensitivity of CTA and MRA diminished significantly when evaluating lesions distal to the main renal artery, and angiography was more sensitive for those lesions. We think it is likely that because children have smaller-caliber vessels than adults, as well as a higher frequency of branch vessel disease, the sensitivity of CTA and MRA would be even more compromised.
Shahdadpuri et al. [10] developed and used two clinical criteria to guide the use of renal angiography in children: hypertension exceeding the 99th percentile for age and sex, and failure to normalize the blood pressure with a single medication. When these criteria were enforced they found abnormal results in 43% of patients. While this prevalence was found in a tightly screened group of children including both those with and without comorbid conditions, we found a similar prevalence in our series, with 37% of our hypertensive patients without comorbid conditions having abnormal angiograms.
Our study did not directly compare the lesions in this select patient population with lesions in a similar group of children with comorbid conditions. It also did not directly compare the sensitivity of angiography with other imaging modalities in detecting these lesions. However, what we did document was a significant incidence of branch arterial disease in these hypertensive patients without comorbid disease. Angiography has been shown to provide the best spatial resolution to optimally identify such branch stenoses in adults. It is our opinion, therefore, that renal angiography should be used for the evaluation of renovascular causes of pediatric hypertension in this patient population. We acknowledge that many of the hypertensive patients who are referred for renal angiography will have normal studies. However, the major negative health consequences that result from renovascular hypertension make detection imperative.
Angiography is also important in this select patient group because of the potential for treatment through transcatheter intervention. As we have shown, hypertensive children without significant other disease tend to have single focal stenotic lesions. Percutaneous transluminal renal angioplasty (PTRA) has been shown to be a safe and effective treatment for children with hypertension related to RAS [1, 11, 17]. The single focal lesions are much more amenable to PTRA than longer or multiple lesions [1, 11, 17]. PTRA is particularly successful in treating RAS caused by FMD [18, 19]. Even lesions not amenable to PTRA can be successfully treated through selective microcatheter embolization [20, 21].
Traditionally, discrete non-ostial stenotic lesions of the main renal artery have been considered the best candidates for PTRA. Recent evidence, however, has shown that branch artery stenoses might also be successfully treated with PTRA. Cluzel et al. [18] were successful in using PTRA in 21 of 25 (84%) renal branch artery stenoses in adults. Further studies will be needed to evaluate both the short- and long-term benefits of PTRA in branch vessel stenoses in children.
We recommend that the work-up of unexplained hypertension in otherwise healthy children include an initial US to exclude global nephropathy, mass, or focal scarring. Negative non-invasive studies such as CTA, MRA, or captopril scintigraphy do not exclude renovascular disease. Patients with such negative studies, especially those without comorbid disease, should undergo angiography.
Conclusions
Hypertensive children with RAS who do not have significant comorbid diseases have a different pattern and location of stenoses than those who do have systemic disease or previous surgery. The lesions in these patients tend to be single and focal and involve smaller branch vessels. Renal angiography should be the imaging modality of choice in evaluating these children because of its superior sensitivity in detecting branch vessel disease, as well as its therapeutic role in PTRA.
References
Courtel JV, Soto B, Niaudet P, et al (1998) Percutaneous transluminal angioplasty of renal artery stenosis in children. Pediatr Radiol 28:59–63
McTaggart SJ, Gelati S, Walker R, et al (2000) Evaluation and long-term outcome of pediatric renovascular hypertension. Pediatr Nephrol 14:1022–1029
Vasbinder GB, Nelemans PJ, Kessels AG, et al (2004) Accuracy of computed tomographic angiography and magnetic resonance angiography for diagnosing renal artery stenosis. Ann Intern Med 141:674–682
Schoenberg SO, Knopp MV, Londy F, et al (2002) Morphologic and functional magnetic resonance imaging of renal artery stenosis: a multireader tricenter study. J Am Soc Nephrol 13:158–169
Hiner LB, Falkner B (1993) Renovascular hypertension in children. Pediatr Clin North Am 40:123–140
Hamilton SJ, Friedman JM (2000) Insights into the pathogenesis of neurofibromatosis 1 vasculopathy. Clin Genet 58:341–344
Bruno S, Remuzzi G, Ruggenenti P (2004) Transplant renal artery stenosis. J Am Soc Nephrol 15:134–141
Kolluri R, Ansel G (2004) Fibromuscular dysplasia of bilateral brachial arteries - a case report and review. Angiology 55:685–689
Deal JE, Snell MF, Barratt TM, et al (1992) Renovascular disease in childhood. J Pediatr 121:378–384
Shahdadpuri J, Frank R, Gauthier BG, et al (2000) Yield of renal arteriography in the evaluation of pediatric hypertension. Pediatr Nephrol 14:816–819
Mali WP, Puijlaert CB, Kouwenberg HJ, et al (1987) Percutaneous transluminal renal angioplasty in children and adolescents. Radiology 165:391–394
Bloch MJ, Basile J (2004) Clinical insights into the diagnosis and management of renovascular disease. Minerva Med 95:357–373
Garel L, Dubois J, Robitaille P, et al (1995) Renovascular hypertension in children: curability predicted with negative intrarenal Doppler US results. Radiology 195:401–405
Lagomarsino E, Orellana P, Munoz J, et al (2004) Captopril scintigraphy in the study of arterial hypertension in pediatrics. Pediatr Nephrol 19:66–70
Slovut DP, Olin JW (2004) Fibromuscular dysplasia. N Engl J Med 350:1862–1871
Vasbinder GB, Nelemans PJ, Kessels AG, et al (2001) Diagnostic tests for renal artery stenosis in patients suspected of having renovascular hypertension: a meta-analysis. Ann Intern Med 135:401–411
Tyagi S, Kaul U, Satsangi D, et al (1997) Percutaneous transluminal angioplasty for renovascular hypertension in children: initial and long-term results. Pediatrics 99:44–49
Cluzel P, Raynaud A, Beyssen B, et al (1994) Stenoses of renal branch arteries in fibromuscular dysplasia: results of percutaneous transluminal angioplasty. Radiology 193:19–21
Surowiec SM, Sivamurthy N, Rhodes JM, et al (2003) Percutaneous therapy for renal artery fibromuscular dysplasia. Ann Vasc Surg 17:650–655
Ishijima H, Ishizaka H, Sakurai M, et al (1997) Partial renal embolization for pediatric renovascular hypertension secondary to fibromuscular dysplasia. Cardiovasc Intervent Radiol 20:383–386
Kunzendorf U, Keller F, Schwietzer G, et al (1990) Control of renovascular hypertension by renal embolization. Am J Nephrol 10:339–343
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vo, N.J., Hammelman, B.D., Racadio, J.M. et al. Anatomic distribution of renal artery stenosis in children: implications for imaging. Pediatr Radiol 36, 1032–1036 (2006). https://doi.org/10.1007/s00247-006-0253-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-006-0253-8